Gastrointestinal arteriovenous malformation (GI AVM) is a rare condition. It happens when arteries and veins in the GI tract connect in an abnormal way. This skips the usual capillary network.

These malformations can mess with blood flow. This can cause bleeding that doesn’t have a clear cause. The colon is where GI AVMs most often show up. But they can also appear in the esophagus, leading to serious bleeding.
It’s important to know about GI AVMs. This is true, even more so for older adults. They are more likely to have these vascular issues.
Key Takeaways
- GI AVM is a rare vascular anomaly involving abnormal connections between arteries and veins.
- It can cause unexplained bleeding in the GI tract.
- The colon is the most common site, but it can occur in other areas like the esophagus.
- GI AVMs can lead to life-threatening bleeding if not properly managed.
- Understanding GI AVM is key for effective care, mainly for older adults.
Understanding GI AVM: Definition and Prevalence
Gastrointestinal Arteriovenous Malformations (AVMs) are complex vascular anomalies. They need a deep understanding for effective management. GI AVMs are abnormal connections between arteries and veins in the gastrointestinal tract. They bypass the capillary system and can lead to significant health issues.
What Defines a Gastrointestinal Arteriovenous Malformation
A GI AVM is a direct shunt between an artery and a vein, skipping the capillary bed. This abnormal vascular structure can cause bleeding, pain, and other complications. We will explore the specifics of these malformations and their impact on patient health.
Epidemiology and Risk Factors
The epidemiology of GI AVMs shows they affect about 10 per 100,000 people. The incidence rate is about 1 per 100,000 per year. They are equally common among men and women and across all ethnicities. Certain risk factors, such as chronic kidney disease (CKD), increase the likelihood of developing GI AVMs.
While the overall prevalence of GI AVMs is not fully understood, research suggests they are more common in patients with specific underlying conditions. Understanding these risk factors is key for early detection and management.
Anatomical Distribution in the GI Tract
GI AVMs can occur in various parts of the gastrointestinal tract, with the colon being the most common site. They can also be found in other areas, such as the esophagus, stomach, small intestine, and rectum, albeit less frequently. We will examine the implications of AVM location on symptoms and treatment approaches.
By understanding the anatomical distribution of GI AVMs, healthcare providers can better diagnose and manage these complex vascular malformations. This can ultimately improve patient outcomes.
Pathophysiology and Causes of GI AVM
The pathophysiology of GI AVM involves complex vascular abnormalities. These are not yet fully understood. Research shows that GI AVMs develop due to various factors. These include vascular structure abnormalities and genetic predispositions.
Vascular Structure Abnormalities
GI AVMs have abnormal connections between arteries and veins in the gastrointestinal tract. These vascular malformations can cause serious health problems. Issues include bleeding and other complications.
The abnormal vascular structure is thought to result from several factors. These include vascular degeneration and increased venous pressure.
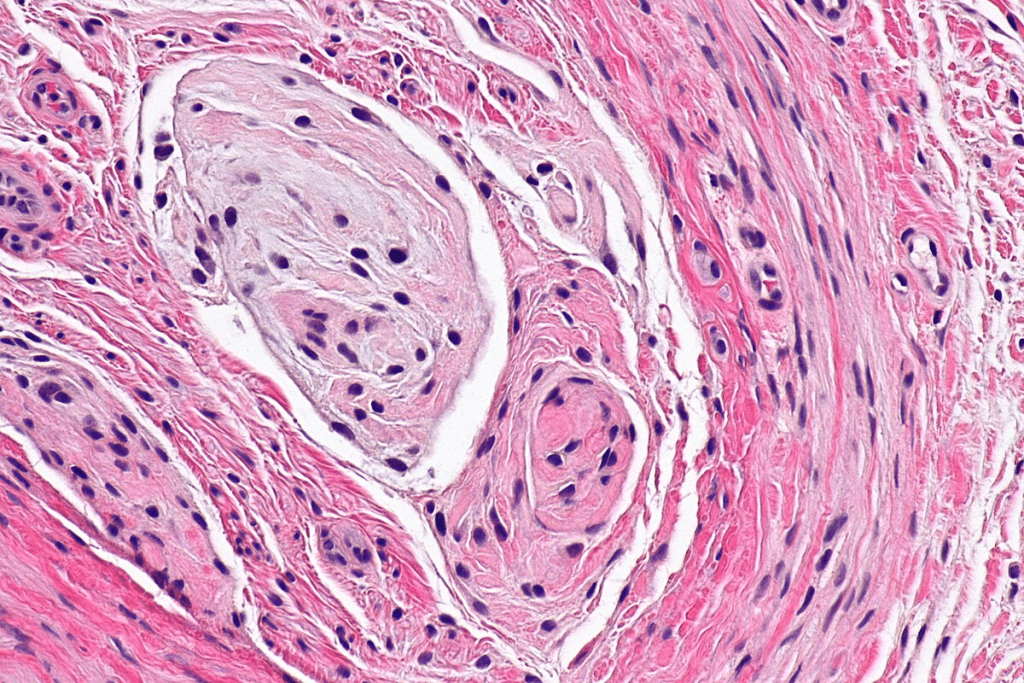
The exact mechanisms behind these abnormal vascular structures are being studied. It’s believed that genetic and environmental factors contribute to their development.
Genetic and Acquired Factors
Genetic and acquired factors both play a role in GI AVMs. Genetic factors may increase the risk of vascular malformations. Acquired factors, like aging and certain medical conditions, also contribute.
About 12% of people with AVMs show symptoms. The annual risk of AVM hemorrhage is between 2“4%. Understanding these risks is key for managing and treating GI AVMs.
The underlying pathology of AVM formation is complex. It involves hypotheses like vascular degeneration and increased venous pressure. More research is needed to understand the causes. This will help in developing prevention and treatment strategies.
Clinical Manifestations and AVM Complications
It’s key to know how GI AVMs show up in patients. They often cause bleeding in the gut, more so in people over 50. The signs can be different and need a detailed check-up to spot.
Common Symptoms of GI AVM
AVM symptoms include hematemesis, melena, bleeding per rectum, unexplained iron deficiency, and anemia. These signs can change and happen often. Doctors must watch closely to catch them early.
“The signs of GI AVMs can differ a lot,” doctors say. “We need to be very careful to find them.” Spotting these signs early is key to helping patients.
Gastrointestinal Bleeding Patterns
Bleeding in the gut is a big sign of GI AVMs. It can show up as blood in the stool or as a drop in iron levels. Each case is different, and how often it happens can change.
- Overt bleeding: hematemesis, melena, or bleeding per rectum
- Occult bleeding: leading to iron deficiency anemia
- Intermittent bleeding: with periods of quiescence between episodes
Potential Complications and Health Risks
If not treated, GI AVMs can cause big problems. These include severe anemia, unstable blood pressure, and even life-threatening bleeding. Quick action is needed to avoid these issues. The chance of bleeding again is a big worry, so we keep a close eye on patients.
When dealing with GI AVMs, knowing the risks is vital. We aim to prevent these problems by acting fast. Understanding these issues helps us give our patients the best care.
Diagnostic Approaches for AVM in the Digestive Tract
Identifying GI AVMs requires a mix of endoscopy, imaging, and lab tests. These vascular anomalies can show up in many ways. They can also lead to serious health issues.
Endoscopic Evaluation Methods
Endoscopy is key in spotting GI AVMs. Capsule endoscopy helps find these lesions in the small intestine. This area is hard to see with a regular endoscopy.
Key endoscopic methods include:
- Conventional upper and lower GI endoscopy
- Capsule endoscopy for small bowel examination
- Double-balloon enteroscopy for deeper small bowel lesions
Imaging Techniques
Imaging is vital for finding and understanding GI AVMs. Angiography helps see the malformation’s blood structure. It also helps plan treatments.
Common imaging modalities used include:
- Angiography
- Computed Tomography (CT) scans
- Magnetic Resonance Imaging (MRI)
Laboratory Tests and Biomarkers
Labs are key for checking how GI AVMs affect health. Biomarkers help spot patients at risk of serious problems.
Relevant laboratory tests include:
- Complete Blood Count (CBC) to assess for anemia
- Coagulation studies to evaluate bleeding risk
- Liver function tests, as some GI AVMs can affect liver function
New tech like capsule endoscopy and angiography has boosted detection rates. While endoscopy is often used, sometimes angiography or surgery is needed for a clear diagnosis.
Treatment Options and Management Strategies
Managing GI AVMs requires a mix of endoscopic, surgical, and supportive therapies. Each treatment plan is made for the patient’s specific needs. This includes the size, location, and how severe the AVM is.
Endoscopic Interventions
Endoscopic therapy is often the first step for GI AVMs. Argon plasma coagulation (APC) is a top choice for stopping bleeding. It uses electric current to coagulate the tissue.
In some cases, hemostasis with clips is used instead or alongside APC. This depends on the situation.
Surgical Management
Surgery is needed for severe or recurring GI AVMs that can’t be treated endoscopically. The surgery can range from removing the affected part to more complex procedures. This depends on where and how big the AVM is.
For example, AVMs in the small intestine might need a segmental resection.
Medication and Supportive Therapies
Along with treatments like endoscopy and surgery, medication and supportive therapies are key. Patients might get iron to treat anemia from bleeding. Medications that help reduce blood flow or clotting might also be used.
Supportive care, like nutrition and monitoring, is vital for the patient’s overall health.
Advanced Treatment at Specialized Centers
For complex or hard-to-treat cases, going to specialized centers is a good idea. These centers have the latest treatments and teams from different fields. They work together to create a treatment plan that fits the patient’s needs.
Conclusion
GI AVM is a rare but serious condition that needs quick diagnosis and treatment. It’s important for doctors to know about GI AVM, its frequency, and risk factors. This is true, even more so for patients with conditions like ESRD.
Liv Hospital is a key player in treating complex conditions like GI AVM. They follow international standards and keep improving. Their patient support and guidance help ensure the best treatment results.
Knowing about GI AVM and its dangers, like severe bleeding, is key. While GI AVM is different from brain AVM or venous malformation, learning about all vascular malformations helps in treating them better.
Healthcare providers should stay updated on GI AVM’s diagnosis and treatment. This way, they can give the best care, even for rare conditions like AVM disease brain or brain AVM.
FAQ’s:
What is a Gastrointestinal Arteriovenous Malformation (GI AVM)?
A GI AVM is a rare condition in the gut. It’s when arteries and veins connect abnormally, affecting blood flow.
What are the common symptoms of GI AVM?
GI AVM symptoms include bleeding in the gut. This can happen suddenly or over time. It might cause anemia or other serious problems.
How is GI AVM diagnosed?
To diagnose GI AVM, doctors use endoscopies and imaging like angiography. They also do lab tests to understand the malformation’s impact.
What are the treatment options for GI AVM?
Treatment for GI AVM varies. It can include endoscopic procedures, surgery, or medication. The choice depends on the AVM’s size, location, and the patient’s health.
Can GI AVMs be treated at any hospital?
Not all hospitals treat GI AVMs. Specialized centers with vascular malformation expertise offer better treatment options and outcomes.
What is the prevalence of GI AVM among different genders and ethnicities?
GI AVMs affect both genders and ethnicities equally. This shows the condition is not biased towards any group.
Are there any genetic factors associated with GI AVM?
Research suggests genetic and acquired factors play a role in GI AVMs. The exact causes are not fully understood yet.
What are the potentially complications of untreated GI AVM?
Untreated GI AVMs can cause serious problems. These include ongoing bleeding, anemia, and even life-threatening hemorrhage. Early diagnosis and treatment are key.
How do GI AVMs disrupt normal blood flow?
GI AVMs disrupt blood flow by creating abnormal connections between arteries and veins. This bypasses the normal capillary network, leading to various symptoms.
What is the role of angiography in diagnosing GI AVM?
Angiography is vital for diagnosing GI AVM. It provides detailed images of the vascular anatomy. This helps identify the malformation’s location and extent.
Can GI AVMs occur in any part of the GI tract?
While most GI AVMs happen in the colon, they can also occur in the esophagus, stomach, or small intestine. These cases are less common.
References
Hirayama, Y., Shiraki, K., & Tanaka, N. (2018). Gastric arteriovenous malformation with characteristic endoscopic findings: A case report. Iranian Red Crescent Medical Journal, 20(3), e13796.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6148157/Sy, E. D., Lu, W.-H., Liu, Y.-S., & Shan, Y.-S. (2025). Intestinal arteriovenous malformation managed with palliative ligation and division of the feeding artery: A case report. Frontiers in Pediatrics, 13, 1496089.https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2025.1496089/pdf



































