Choosing the right anesthesia for surgery is a big decision. It’s a top worry for patients and their families. They want to know it’s safe.
Our team of experts helps patients pick the best anesthesia option. We consider their health, the surgery type, and what they prefer.

The safest anesthetic depends on the patient and the surgery. We’ll look at different anesthetics, their safety, and the latest research. This will help us understand which one is safest.
Key Takeaways
- The safest anesthesia technique is tailored to individual patient needs.
- Patient factors, such as overall health, influence anesthesia choices.
- Different types of anesthesia have varying safety profiles.
- Regional anesthesia, like spinal and epidural, is used for various procedures.
- Local anesthesia can be used alone or with sedation for minor surgeries.
The Science Behind Modern Anesthesia
Modern anesthesia is a complex field. It requires a deep understanding of how anesthetics interact with our bodies. Thanks to medical research and technology, anesthesia has come a long way.

How Anesthesia Affects Your Body
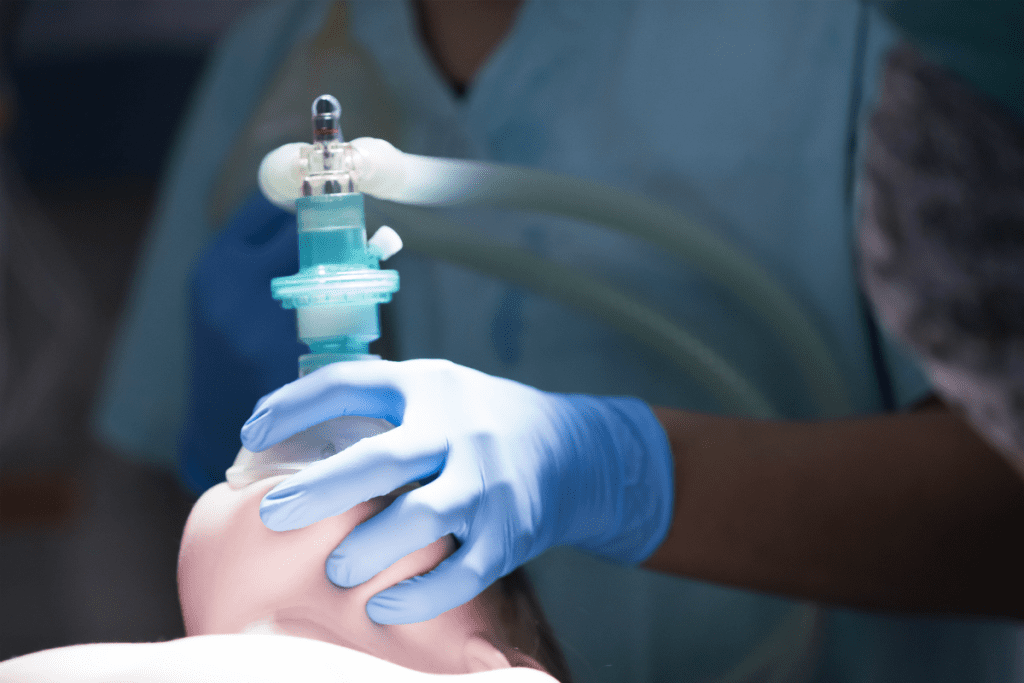
General anesthesia uses a mix of medications and gases. This ensures patients don’t feel pain during surgery. Anesthetics work by depressing the nervous system, reducing the pain response. But how anesthesia affects us can vary a lot.
Recent studies show important trends in anesthesia safety. New anesthetic agents and monitoring systems have reduced complications. These advancements have made anesthesia safer.
- Reduced risk of pulmonary complications: Modern anesthetic techniques minimize the risk of respiratory problems.
- Enhanced patient comfort: Advanced anesthetics provide more effective pain management.
- Improved safety profiles: Newer anesthetic agents have fewer side effects.
Evolution of Anesthetic Techniques
Anesthetic techniques have evolved a lot. Now, we focus on personalized care and advanced monitoring. Personalized anesthesia care means tailoring the anesthetic to each patient’s needs.
Some key developments include:
- The use of regional anesthesia, which numbs a specific region of the body, reduces the need for general anesthesia.
- The development of fast-recovery anesthesia agents enables patients to recover quickly from anesthesia.
- The implementation of advanced monitoring systems allows anesthesiologists to closely monitor patients’ vital signs during surgery.
Understanding how anesthesia works is key. It helps us choose the right anesthesia for each patient. This personalized approach has greatly improved patient outcomes and safety.
Types of Anesthesia and Their Safety Profiles
Anesthesia comes in many forms, each with its own safety and use. The right choice depends on the procedure, the patient’s health, and personal wishes. Knowing these differences helps in making better medical choices.
General Anesthesia
General anesthesia makes you unconscious, perfect for big surgeries. But it can lead to breathing and heart problems. It’s important to pick the right patient and watch them closely to avoid these risks.
Regional Anesthesia
Regional anesthesia numbs a part of your body, like your legs. It includes spinal and epidural methods. It’s safer for the lungs and heart than general anesthesia, making it better for some patients.
Local Anesthesia
Local anesthesia numbs a small area for minor procedures. It’s mostly safe, but the dose and area must be right to avoid harm.
Intravenous Sedation
Intravenous sedation relaxes and eases pain without making you sleep. It’s safe for small procedures when watched closely. The sedation level can be changed, giving flexibility.
Knowing about the safety and uses of these anesthetics helps both patients and doctors make the best choices for each person and procedure.
Why Regional Anesthesia Often Outperforms General Anesthesia
Regional anesthesia is becoming more popular because it’s safer than general anesthesia for many surgeries. It blocks pain in the area being operated on. This makes it safer for patients and doctors.
Lower Rates of Pulmonary Complications
Regional anesthesia has a big advantage: it leads to fewer pulmonary complications. General anesthesia can harm breathing, but regional anesthesia doesn’t. This helps patients breathe better after surgery.
Reduced Cardiovascular Risks
It also has lower cardiovascular risks than general anesthesia. Regional anesthesia doesn’t affect the whole body like general anesthetics do. This is good for people with heart problems.
Equivalent Surgical Outcomes
Regional anesthesia works just as well as general anesthesia for many surgeries. It has the same success rate but with fewer side effects. This makes it a better choice when possible.
In summary, regional anesthesia is safer than general anesthesia. It has fewer risks for the lungs and heart, and it works just as well for surgeries. As medicine gets better, more people will choose regional anesthesia.
Intravenous Sedation: The Safer Choice for Minor Surgeries
Intravenous sedation is now seen as a safer option for minor surgeries compared to general anesthesia. It uses medications through an IV to make patients feel calm and sleepy. This method is great for minor surgeries because it aims to reduce risks and help patients recover quickly.
Comparing Hypotension Events
Intravenous sedation has fewer hypotension events than general anesthesia. Research shows that patients under sedation have a 8.3% chance of hypotension, while general anesthesia has a 21.6% rate. This lower rate of hypotension makes sedation safer for patients, reducing the chance of complications and improving outcomes.
Benefits of Shorter Anesthesia Duration
Intravenous sedation leads to shorter anesthesia times, which is safer. Shorter anesthesia times lower the risk of complications and help patients recover faster. This is key in outpatient settings, where quick and safe discharge is the goal.
Oxygen Level Maintenance Safety
Keeping oxygen levels safe during surgery is vital. Sedation allows for better control over oxygen levels, unlike general anesthesia. By ensuring patients get enough oxygen, we reduce the risk of hypoxia and complications, making minor surgeries safer.
Fast-Recovery Anesthesia Agents: Maximizing Safety in Outpatient Settings
In outpatient surgeries, new safety standards are being set. Fast-recovery anesthesia agents are leading this change. They make outpatient procedures safer and more efficient.
Advantages of Hyperbaric Prilocaine
Hyperbaric prilocaine is a top choice for outpatient anesthesia. It has a fast onset and recovery profile. This means patients can quickly get back to normal, reducing risks and making discharge smoother.
The efficacy of hyperbaric prilocaine in quick recovery is proven. It boosts patient safety and happiness. This makes it perfect for outpatient surgeries.
Other Fast-Acting Agents
Other fast-acting agents are also used for safety in outpatient settings. They have rapid onset and offset. This allows for precise control over anesthesia.
- Agents with a short duration of action, ideal for minor procedures.
- Anesthetics that provide stable hemodynamics, reducing cardiovascular risks.
- Drugs that are quickly metabolized, lowering adverse effect risks.
Using these fast-acting agents improves safety and efficiency in outpatient surgeries. Tailoring anesthesia to each patient’s needs is a big step in modern care.
How Sugammadex Has Revolutionized Anesthesia Safety
Sugammadex has greatly improved anesthesia safety, mainly in surgeries needing muscle relaxation. It has changed how doctors manage muscle blockage. This is because sugammadex quickly and effectively reverses these blocks.
Enhanced Recovery from Neuromuscular Blockade
Sugammadex makes rapid reversal of neuromuscular blockade possible. This is key in surgeries needing muscle relaxation. It works by wrapping around the neuromuscular blockers, allowing for quick recovery and less chance of muscle weakness.
Using sugammadex leads to more consistent and safe recovery times. This is vital in the operating room, where patient safety is top priority.
Comparison with Traditional Reversal Agents
Older reversal agents, like neostigmine, have slower effects and can cause side effects. Sugammadex, on the other hand, starts working faster and has fewer side effects. This is a big plus for anesthesia safety, making it easier to manage muscle blockage.
Research shows sugammadex can reverse muscle blockage much quicker than old agents. This quick action is good for patient outcomes by shortening the time muscles are blocked.
Patient Outcomes and Safety Improvements
Sugammadex has a big impact on patient outcomes and anesthesia safety. It helps patients recover faster from muscle blockage. This reduces the chance of complications from long-lasting paralysis, making care safer and more satisfying for patients.
Using sugammadex also lowers the risk of breathing problems after surgery. This is a big win for anesthesia safety. It makes anesthesia care safer overall.
Patient-Specific Factors That Determine the Safest Anesthesia
The safest anesthesia is chosen based on each patient’s needs and the surgery type. We look at many factors to get the best results for our patients.
Age and Physical Condition
A patient’s age and physical condition are key in picking the safest anesthesia. Older patients or those with physical issues might need special anesthesia care. For example, older adults might process anesthesia differently, so we adjust the doses carefully.
Patients in good health might handle certain anesthetics better than those with health problems. We check each patient’s health to pick the best anesthesia plan.
Medical History Considerations
A patient’s medical history is very important for anesthesia planning. We look at conditions like diabetes, heart disease, or past bad reactions to anesthesia. We go over each patient’s medical history to spot risks and plan how to avoid them.
For instance, patients with heart issues might need more watchful care during anesthesia to avoid problems.
Surgical Context and Procedure Type
The surgical context and procedure type also affect anesthesia choice. Different surgeries need different levels of anesthesia. We work with surgeons to understand each surgery’s needs and tailor our anesthesia plan.
For simple surgeries, local or regional anesthesia might be better to lower risks from general anesthesia. But, more complex surgeries might need general anesthesia.
By carefully looking at these factors and the surgery type, we can give our patients the safest and most effective anesthesia care.
Conclusion: Finding Your Safest Anesthesia Option
We’ve looked at different types of anesthesia and their safety levels. The right choice depends on the patient’s needs and the surgery. Anesthesiologists work with patients to find the safest option for them.
Healthcare providers consider many factors when choosing anesthesia. These include the patient’s age, health, and medical history. This teamwork is key to ensuring the best care for each patient.
FAQ
What is the safest type of anesthesia?
The safest anesthesia depends on many factors. These include the patient’s health and the surgery type. Our team helps choose the best anesthesia for each patient.
How does anesthesia work?
Anesthesia numbs the body to prevent pain during surgery. It comes in different types, like general and local anesthesia. Each type works differently to achieve the goal.
What are the benefits of regional anesthesia compared to general anesthesia?
Regional anesthesia is safer for some patients. It has fewer complications than general anesthesia. It can also offer similar surgery results with fewer risks.
Is intravenous sedation safer than general anesthesia for minor surgeries?
Yes, for minor surgeries, intravenous sedation is safer. It has fewer risks of low blood pressure and shorter recovery times.
What are fast-recovery anesthesia agents, and how do they improve safety?
Fast-recovery agents, like hyperbaric prilocaine, are designed for outpatient surgeries. They reduce recovery times and side effects, making them safer.
How has sugammadex improved anesthesia safety?
Sugammadex has made anesthesia safer by allowing quicker recovery from muscle blockage. This improves patient safety and outcomes.
What patient-specific factors influence the choice of anesthesia?
Many factors influence anesthesia choice. These include age, health, medical history, and surgery type. Each patient’s needs are considered.
What are the possible side effects of anesthesia?
Side effects of anesthesia vary by type and patient. Common ones include nausea, dizziness, and breathing problems.
How long does anesthesia last?
Anesthesia duration varies by type and procedure. Local anesthesia wears off quickly, while general anesthesia takes longer to recover from.
Can I discuss my anesthesia options with my healthcare provider?
Yes, discussing anesthesia options with your healthcare provider is important. It helps choose the safest and most suitable option for you.
References
- Eick, S. M., et al. (2020). The role of personalized medicine in anesthesia. Journal of Personalized Medicine, 10(3), 101.








