Every year, thousands of people worldwide die from sudden cardiac arrests. These are often caused by deadly heart rhythm types. It’s vital to know about these life-threatening conditions to get help quickly.
We will look into the important topic of fatal arrhythmia classifications. We’ll learn about the conditions that can cause serious health problems if not treated right away.
It’s key for doctors and people to understand fatal cardiac rhythms. This knowledge helps in reducing risks from heart issues.
Identify the critical five fatal cardiac rhythms. Knowing these rhythms is essential for urgent life-saving action.
Key Takeaways
- Recognizing the signs of fatal cardiac rhythms can save lives.
- Understanding the classifications of fatal arrhythmias is key for diagnosis.
- Quick medical help is essential for treating deadly heart rhythm types.
- Learning about heart conditions can lower risks.
- Early treatment of fatal cardiac rhythms can greatly improve survival chances.
The Heart’s Electrical System and Normal Function
Understanding the heart’s electrical system is key to knowing how it works. The heart beats in sync thanks to its electrical system.
The heart’s electrical network controls its rhythm. It makes sure the heart’s chambers beat together, pumping blood well.
How the Cardiac Conduction System Works
The heart’s electrical system starts with the SA node, or natural pacemaker. It sends out electrical signals to the atrial tissue.
These signals then go to the AV node. From there, they travel through the Bundle of His, bundle branches, and Purkinje fibers. This makes the ventricles contract in sync, keeping a normal rhythm.
|
Component |
Function |
|---|---|
|
Sinoatrial (SA) Node |
Generates electrical impulses |
|
Atrioventricular (AV) Node |
Delays electrical impulses to allow atrial contraction |
|
Bundle of His |
Transmits impulses to the ventricles |
|
Purkinje Fibers |
Causes ventricular contraction |
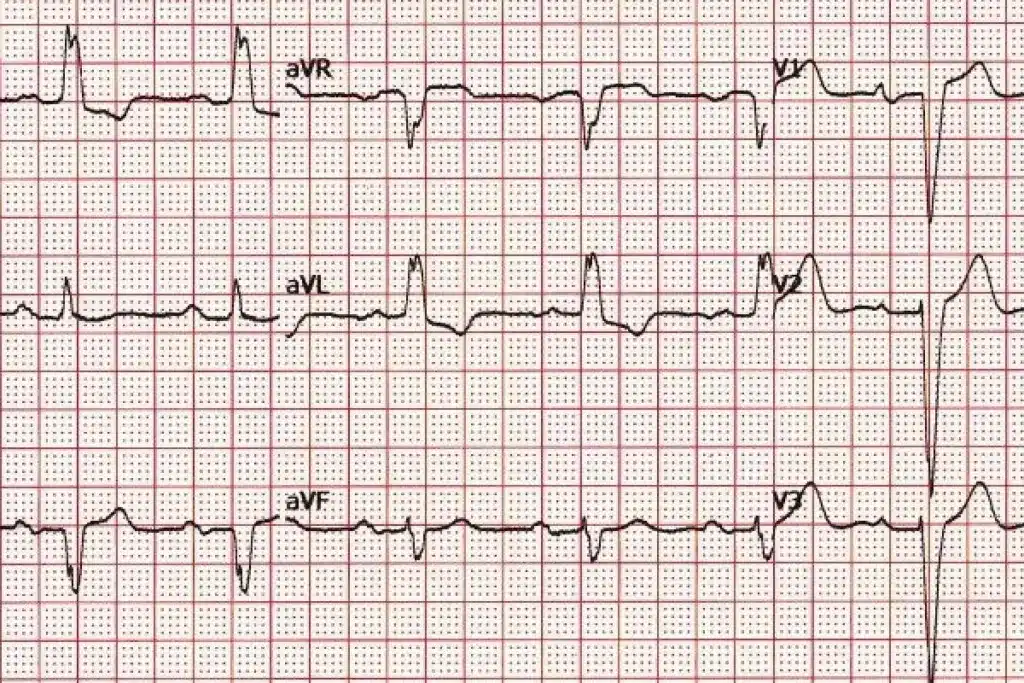
Normal Electrical Patterns on ECG
A normal ECG shows the heart’s electrical activity. It includes the P wave, QRS complex, and T wave.
Knowing these patterns helps spot heart problems. For example, ventricular fibrillation is a dangerous rhythm seen on ECG.
“The electrocardiogram is a fundamental tool in cardiology, providing insights into the heart’s electrical activity and helping diagnose potentially fatal heart conditions.”
Cardiology Expert
It’s important to know the normal ECG patterns. This helps spot dangerous rhythms like ventricular fibrillation, which needs quick medical help.
Understanding Cardiac Arrhythmias
Cardiac arrhythmias happen when the heart’s electrical activity gets disrupted. This can make the heart beat too fast, too slow, or irregularly. Knowing about these arrhythmias is key for finding and treating them.
Definition and Classification of Heart Rhythm Disorders
Arrhythmias are grouped based on where they start in the heart and how they affect the heart rate. There are supraventricular arrhythmias and ventricular arrhythmias. Supraventricular ones start above the ventricles, like atrial fibrillation. Ventricular ones start in the ventricles, like ventricular tachycardia.
Arrhythmias are also sorted by their effect on heart rate and rhythm. Tachyarrhythmias have a fast heart rate over 100 beats per minute. Bradyarrhythmias have a slow heart rate under 60 beats per minute.
Differentiating Benign vs. Life-Threatening Arrhythmias
Not all arrhythmias are dangerous. Some are harmless and don’t need treatment. But others can be deadly. Life-threatening arrhythmias like ventricular fibrillation need quick medical help.
|
Arrhythmia Type |
Characteristics |
Clinical Significance |
|---|---|---|
|
Atrial Fibrillation |
Irregular, rapid heart rhythm originating in the atria |
Can increase stroke risk; may require anticoagulation therapy |
|
Ventricular Tachycardia |
Rapid heart rhythm originating in the ventricles |
Can be life-threatening if pulseless; requires immediate defibrillation |
|
Ventricular Fibrillation |
Chaotic, disorganized heart rhythm in the ventricles |
Life-threatening; requires immediate CPR and defibrillation |
Telling benign from life-threatening arrhythmias is vital for the right treatment. We use clinical checks, ECGs, and sometimes more tests to figure this out.
The Five Fatal Cardiac Rhythms: Overview and Significance
It’s key for doctors to know about the five fatal cardiac rhythms. This knowledge helps them act fast. These rhythms can lead to sudden cardiac death, so quick action is vital.
What Makes These Rhythms Immediately Life-Threatening
The five fatal cardiac rhythms are very dangerous. They can cause cardiac arrest quickly if not treated right away. These rhythms mess up the heart’s work, leading to poor blood flow and oxygen to organs.
Key characteristics of these fatal rhythms include:
- Rapid onset
- Severe hemodynamic compromise
- High risk of degeneration into more severe arrhythmias
Epidemiology and Mortality Statistics
The study of fatal cardiac rhythms shows their big impact on health. Research shows these rhythms cause a lot of sudden cardiac deaths around the world.
Some notable statistics include:
- Cardiac arrest affects about 350,000 people in the United States every year.
- Most cardiac arrests are from ventricular fibrillation or pulseless ventricular tachycardia.
- Survival rates for cardiac arrest are low, showing we need better prevention and treatment.
Knowing about the five fatal cardiac rhythms helps us see why quick medical help is so important. It also shows we need more research into good treatments.
Ventricular Fibrillation (VF)
Ventricular fibrillation is a deadly heart rhythm disorder that needs quick medical help to avoid sudden death. It’s marked by a fast, irregular heart rhythm that stops the heart from pumping blood well.
Mechanism and Pathophysiology
The heart’s electrical and structural issues cause ventricular fibrillation. It happens when the heart’s electrical activity gets disrupted. This leads to chaotic, uncoordinated contractions of the ventricular muscle.
Many things can start VF, like severe heart disease, electrical shock, or certain medicines. Knowing how it works helps doctors find better treatments.
Causes and Risk Factors
Several things can make someone more likely to get ventricular fibrillation. These include:
- Coronary artery disease
- Previous heart attack
- Cardiomyopathy
- Heart valve problems
- Electrolyte imbalances
Spotting these risk factors is key for preventing and treating VF early.
ECG Characteristics and Diagnosis
Doctors use an electrocardiogram (ECG) to diagnose ventricular fibrillation. The ECG shows a chaotic, irregular pattern without clear P waves or QRS complexes.
ECG characteristics include:
- Irregular, erratic rhythm
- Absence of P waves
- No discernible QRS complexes
Quickly spotting these ECG signs is vital for managing VF right away.
Pulseless Ventricular Tachycardia
Pulseless ventricular tachycardia is a serious heart rhythm disorder that needs quick medical help. It shows a fast heart rate without a pulse, which is a sign of a dangerous heart rhythm.
Pathophysiology
This condition happens when the heart’s electrical activity gets disrupted. This leads to fast and uncoordinated heartbeats. As a result, the heart doesn’t pump enough blood, causing no pulse.
It often occurs in people with heart diseases like coronary artery disease or cardiomyopathy.
Common Causes and Predisposing Factors
Several things can lead to or cause pulseless ventricular tachycardia. These include:
- Ischemic heart disease: Reduced blood flow to the heart muscle can lead to dangerous arrhythmias.
- Cardiomyopathy: Diseases affecting the heart muscle can disrupt normal electrical activity.
- Electrolyte imbalances: Abnormal levels of potassium, magnesium, or other electrolytes can affect heart rhythm.
- Medications: Certain drugs can provoke life-threatening heart rhythms.
ECG Patterns and Diagnostic Criteria
Doctors use electrocardiogram (ECG) analysis to diagnose pulseless ventricular tachycardia. The ECG shows a fast ventricular rate. It typically displays:
- A wide QRS complex tachycardia.
- Absence of P waves or evidence of AV dissociation.
- A rate typically between 150-250 beats per minute.
Quickly spotting these patterns is key for timely treatment.
Asystole: Cardiac Standstil
Asystole is a serious heart emergency that needs quick action. It happens when the heart’s electrical system stops working. This leads to no heartbeats and no blood flow.
Mechanism and Pathophysiology
Asystole happens when the heart’s electrical system fails. This can be caused by many things that mess with the heart’s electrical signals. The heart’s cells and ions play a big role in this failure.
Knowing how asystole works is key to finding good treatments. It’s about studying the heart’s electrical signals and what goes wrong.
Etiologies of Asystole
Many things can cause asystole, like serious heart disease or imbalances in electrolytes. Finding out why it happens is important for treating it right.
- Severe cardiac disease
- Electrolyte imbalances
- Certain medications
- Hypoxia
- Trauma
Confirming True Asystole vs. Fine VF
Telling asystole apart from fine ventricular fibrillation (VF) is very important. Both look like a flatline on the ECG, but they need different treatments.
|
Characteristics |
Asystole |
Fine VF |
|---|---|---|
|
ECG Appearance |
Flatline |
Fine fibrillatory waves |
|
Treatment Approach |
Focus on pacing or medication |
Defibrillation |
Diagnosing asystole means looking closely at the ECG and how the patient feels. It’s important to check the ECG in different leads to make sure it’s asystole and not fine VF.
Pulseless Electrical Activity (PEA)
PEA, or Pulseless Electrical Activity, is a state where the heart’s electrical activity goes on, but it can’t move blood. This is a serious part of cardiac arrest and needs quick action.
Understanding the Paradox: Electrical Activity Without Mechanical Function
In a normal heart, electrical signals cause it to contract and pump blood. But in PEA, there’s no pulse or blood flow, even though electrical signals are present. This is what makes PEA so unique.
Many things can cause this problem, like severe metabolic issues or heart diseases. Knowing what causes it is key to treating PEA well.
The “H’s and T’s” of PEA Causes
PEA often has causes that can be remembered with the “H’s and T’s”. These include:
- Hypovolemia – Low blood volume
- Hypoxia – Not enough oxygen
- Hydrogen ion (acidosis) – Too much blood acidity
- Hyperkalemia or Hypokalemia – Wrong potassium levels
- Hypothermia – Too cold
- Tension pneumothorax – Air trapped in the chest
- Tamponade, cardiac – Fluid around the heart
- Toxins – Poisonous substances
- Thrombosis, coronary – Heart attack from a clot
- Thrombosis, pulmonary – Clot in the lungs
|
Cause |
Description |
Clinical Implication |
|---|---|---|
|
Hypovolemia |
Low blood volume |
Fluid resuscitation needed |
|
Hypoxia |
Not enough oxygen |
Oxygen therapy required |
|
Hyperkalemia |
Too much potassium |
Cardiac membrane stabilizers needed |
Clinical Assessment and Diagnosis
To diagnose PEA, we check for no pulse but electrical activity on an ECG. We also look for the cause.
Quickly checking the patient’s situation is key. We look for signs of “H’s and T’s” and other causes. Treating PEA well means finding and fixing the cause fast, along with good CPR.
Torsades de Pointes
Torsades de Pointes is a serious heart rhythm disorder that needs quick medical help. It’s a complex abnormal heart rhythm that’s hard to diagnose and manage.
Mechanism and Distinctive Characteristics
Torsades de Pointes, or “twisting of the points,” is a fast, irregular heartbeat. It can cause sudden cardiac death if not treated fast. It happens when the QT interval is too long, which can be from birth or caused by other factors like electrolyte imbalances or certain medicines.
The unique thing about Torsades de Pointes is its ECG pattern. It shows a “twisting” of the QRS complex around the baseline. This pattern is key for diagnosing the condition.
Risk Factors and Triggers
Many risk factors and triggers can lead to Torsades de Pointes. These include:
- Congenital long QT syndrome
- Electrolyte imbalances, like low potassium and magnesium
- Certain medicines, like antiarrhythmics, antibiotics, and antipsychotics
- Slow heart rates
It’s important to manage these risk factors to prevent Torsades de Pointes.
ECG Recognition and Monitoring
Recognizing Torsades de Pointes on an ECG is key for diagnosis. The twisting pattern is a clear sign. It’s also important to watch patients at risk, like those on medicines that can lengthen the QT interval, for early detection.
In summary, Torsades de Pointes is a dangerous arrhythmia that needs quick action. Knowing how it works, its risk factors, and how to spot it on an ECG is essential for managing it well.
Immediate Response to Fatal Cardiac Rhythms
Fatal cardiac rhythms need an immediate and effective response to save lives. Cardiac arrest can happen suddenly. Knowing how to respond quickly is key for both healthcare providers and individuals.
The Chain of Survival
The chain of survival is a series of steps to increase survival chances from cardiac arrest. It includes:
- Recognizing the cardiac arrest and starting the emergency response
- Starting CPR early to keep blood flowing and oxygen levels up
- Using a defibrillator quickly for shockable rhythms
- Providing advanced life support (ALS) for further care
- Managing the patient’s condition after the arrest to prevent future episodes
The American Heart Association says, “The chain of survival is only as strong as its weakest link.” This shows how important a quick and effective response is.
“The chain of survival is only as strong as its weakest link.” – American Heart Association
High-Quality CPR Techniques
High-quality CPR is essential for saving a patient in cardiac arrest. Important aspects include:
|
CPR Component |
Guideline Recommendation |
|---|---|
|
Compression Rate |
100-120 compressions per minute |
|
Compression Depth |
At least 2 inches (5 cm) in adults |
|
Recoil |
Allow complete chest recoil after each compression |
|
Ventilation |
30:2 compression-to-ventilation ratio for adults |
Good CPR means following these guidelines and keeping chest compressions going without breaks. Mechanical CPR devices can help in some cases, but manual CPR is the usual method.
Defibrillation: When and How
Defibrillation is vital for patients in ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT). The sooner it’s done, the better the chances of saving the patient.
Important things to consider for defibrillation include:
- Using an automated external defibrillator (AED) when it’s available and right
- Putting the electrodes correctly
- Keeping CPR going without breaks during defibrillation tries
- Following the maker’s guidelines for energy levels
For manual defibrillators, start with a higher energy level for biphasic defibrillators, as recommended by the maker.
Advanced Cardiac Life Support Protocols
Advanced Cardiac Life Support (ACLS) protocols are key in handling cardiac arrest and serious arrhythmias. They offer a structured way to deal with heart emergencies. This approach helps improve patient results by providing quick and effective care.
Rhythm-Specific Treatment Algorithms
ACLS guidelines stress the need to spot the heart rhythm to decide treatment. Each arrhythmia needs a unique approach, from defibrillation for ventricular fibrillation (VF) to pacing for slow heart rates.
Key steps in rhythm-specific treatment include:
- Rapid identification of the cardiac rhythm
- Choosing the right interventions based on ACLS algorithms
- Keeping a close eye on treatment and making changes as needed
Medication Interventions in Cardiac Arrest
Medicines are vital in ACLS, mainly during cardiac arrest. The right medicine depends on the type of cardiac arrest and the patient’s health.
Common medications used in cardiac arrest include:
- Epinephrine (adrenaline) for its vasoconstrictive effects
- Amiodarone for treating hard-to-treat VF or pulseless VT
- Lidocaine as an alternative to amiodarone in some cases
These medicines are given based on ACLS rules, with careful thought about their benefits and risks.
Post-Resuscitation Care and Management
Good care after a cardiac arrest is key to saving lives and reducing harm. After a patient is brought back from cardiac arrest, the next phase is critical. It’s a chance to improve care and possibly better outcomes.
Targeted Temperature Management
Targeted temperature management (TTM) is a mainstay in caring for post-cardiac arrest patients. TTM cools the patient to a certain temperature to protect the brain. The aim is to keep the body between 32°C and 36°C for at least 24 hours.
This cooling helps reduce brain damage by lowering energy use and stopping harmful chemicals. Keeping the right temperature is important to avoid problems like shivering and infections. We use special systems to control the temperature and watch how the patient responds.
Hemodynamic Stabilization
Keeping vital organs well supplied with blood is key after a cardiac arrest. We work to keep blood pressure right with medicines and fluids. It’s a delicate balance to ensure enough blood flow without too much.
We watch blood pressure, heart function, and oxygen levels closely. This helps us adjust care to meet each patient’s needs, improving their blood flow.
Neurological Assessment and Prognosis
Checking the brain is vital in post-resuscitation care. It helps predict outcomes and guide treatment. We use checks, scans, and tests to see how much brain damage there is.
Early predictions help us know who might not recover well. This allows us to talk with families about treatment options. We do this with care and hope, balancing reality with the chance for recovery.
Prevention Strategies for High-Risk Patients
To prevent cardiac arrest in high-risk patients, we need a mix of advanced technology, medicines, and lifestyle changes. We’ll look at how to lower the risk of cardiac arrest in these patients.
Implantable Cardioverter-Defibrillators (ICDs)
ICDs are small devices implanted under the skin. They watch the heart’s rhythm and shock it back to normal if needed. ICDs have been shown to greatly lower death rates in high-risk patients, like those with serious heart rhythm problems or heart failure.
A study in the New England Journal of Medicine showed ICDs cut sudden cardiac death risk by 31% compared to just medicine. Below is a table with key findings from major ICD trials.
|
Trial Name |
Year |
Population |
Outcome |
|---|---|---|---|
|
MADIT-II |
2002 |
Post-MI, EF ≤ 30% |
31% reduction in mortality |
|
SCD-HeFT |
2005 |
NYHA Class II-III HF |
23% reduction in mortality |
|
DEFINITE |
2004 |
Non-ischemic cardiomyopathy |
35% reduction in mortality |
Antiarrhythmic Medications
Antiarrhythmic medicines are key in preventing cardiac arrest. They help keep the heart’s electrical activity stable, lowering the risk of dangerous heart rhythms. Beta-blockers, for example, are often used to prevent dangerous heart rhythms.
“The use of beta-blockers has become a cornerstone in the management of patients at risk of cardiac arrhythmias, significantly improving survival rates.” –
AHA Guidelines
Other medicines like amiodarone and sotalol are also effective but can have more side effects. The right medicine depends on the patient’s condition, medical history, and any other health issues.
Lifestyle Modifications and Risk Factor Management
Changing your lifestyle is important in preventing cardiac arrest. Patients should eat heart-healthy, exercise regularly, and not smoke. It’s also key to manage risk factors like high blood pressure, diabetes, and high cholesterol.
- Dietary changes: Eat more fruits, vegetables, whole grains, and lean proteins.
- Exercise regularly: Aim for 150 minutes of moderate-intensity aerobic activity weekly.
- Smoking cessation: Use smoking cessation programs and resources.
By combining lifestyle changes with medical treatments, high-risk patients can greatly lower their chance of cardiac arrest.
Emerging Technologies in Arrhythmia Detection and Treatment
New technologies are changing cardiology, focusing on arrhythmia detection and treatment. These advancements are making patient care better and helping us prevent dangerous arrhythmias.
Wearable Cardiac Monitors
Wearable cardiac monitors are changing how we watch for and find arrhythmias. Smartwatches and fitness trackers with ECG can watch your heart all the time. This means we can catch arrhythmias early and act fast.
Key Features:
- Continuous ECG monitoring
- Alert systems for abnormal heart rhythms
- Data analytics for personalized insights
Subcutaneous ICDs and Leadless Pacemakers
Subcutaneous ICDs (S-ICDs) and leadless pacemakers are big steps forward in treating serious arrhythmias. S-ICDs save lives without the need for leads, cutting down on complications.
Leadless pacemakers are a new, less invasive option compared to traditional pacemakers. They don’t need leads, which lowers the chance of infection.
Artificial Intelligence in Arrhythmia Prediction
Artificial intelligence (AI) is being used to predict arrhythmias before they happen. AI looks at lots of data, like ECGs and health records, to spot patterns that might mean an arrhythmia is coming.
AI in cardiology is creating new ways to prevent arrhythmias. It lets doctors take steps to stop arrhythmias before they start.
As we keep using these new technologies, we’re making arrhythmia detection and treatment better. We’re also improving patient care and results. The future of cardiology is all about combining technology, data, and medical knowledge.
Public Health Approaches to Sudden Cardiac Death Prevention
Public health plays a key role in lowering sudden cardiac death rates. Community-based efforts can greatly boost survival chances from cardiac arrest.
Community CPR and AED Training
Community CPR and AED training are vital for preventing sudden cardiac death. Teaching people how to handle cardiac emergencies can save lives.
Training should be easy to find and fit all ages and groups. Schools and community centers should offer these classes.
Key Components of Effective CPR Training:
- Hands-on practice with mannequins
- Instruction on AED use
- Recognition of cardiac arrest symptoms
Public Access Defibrillation Programs
Public access defibrillation programs place AEDs in public spots where cardiac arrests happen. These programs, with CPR training, can save more lives.
|
Location |
AED Availability |
Survival Rate |
|---|---|---|
|
Schools |
Yes |
60% |
|
Public Gyms |
Yes |
55% |
|
Shopping Malls |
Yes |
50% |
By placing AEDs in key spots and teaching their use, we can better fight sudden cardiac death.
Conclusion
It’s key to understand and quickly handle the five fatal cardiac rhythms to stop cardiac arrest. These serious heart rhythm problems need fast action. They include ventricular fibrillation, pulseless ventricular tachycardia, asystole, pulseless electrical activity, and Torsades de Pointes.
We’ve talked about how these dangerous heart rhythms work, how to diagnose them, and how to treat them. It’s important to use defibrillation, CPR, and advanced life support quickly. This helps save lives by improving patient care.
Preventing these issues is also important. This includes using devices like implantable cardioverter-defibrillators and medicines. Changing lifestyles and using new tech like wearable monitors and AI can help too.
By working together, we can better prevent and manage cardiac arrest. This will help save more lives and improve health outcomes for everyone.
FAQ
What are the five fatal cardiac rhythms?
The five fatal cardiac rhythms are ventricular fibrillation, pulseless ventricular tachycardia, asystole, pulseless electrical activity, and torsades de pointes. These rhythms are life-threatening and need immediate medical help.
What is ventricular fibrillation?
Ventricular fibrillation is a dangerous heart rhythm. It happens when the heart’s ventricles beat too fast and irregularly. This stops blood from flowing and causes cardiac arrest.
How is ventricular fibrillation diagnosed?
Doctors use an electrocardiogram (ECG) to spot ventricular fibrillation. The ECG shows a chaotic, irregular pattern of electrical activity.
What is pulseless ventricular tachycardia?
Pulseless ventricular tachycardia is a fast heart rate from the ventricles. It leads to no pulse and poor blood flow.
What is asystole?
Asystole is when the heart stops beating. It means there’s no cardiac contractions or blood flow.
How is asystole differentiated from fine ventricular fibrillation?
Asystole shows no electrical activity on ECG. Fine ventricular fibrillation has a very low, irregular pattern.
What is pulseless electrical activity?
Pulseless electrical activity means the heart’s electrical activity is there, but it doesn’t contract. This results in no blood flow.
What are the common causes of pulseless electrical activity?
Causes include hypovolemia, hypoxia, hydrogen ion (acidosis), hyperkalemia, hypothermia, toxins, tamponade, tension pneumothorax, thrombosis (coronary or pulmonary), and trauma.
What is torsades de pointes?
Torsades de pointes is a fast, irregular heart rhythm. It has a distinctive “twisting” pattern on ECG.
How is torsades de pointes treated?
Treatment involves fixing the cause, like electrolyte imbalances. Medications like magnesium sulfate help stabilize the rhythm.
What is the chain of survival in cardiac arrest?
The chain includes early recognition and calling for help, early CPR, early defibrillation, effective advanced life support, and post-resuscitation care.
What is the role of implantable cardioverter-defibrillators (ICDs) in preventing sudden cardiac death?
ICDs are for patients at high risk. They detect and correct abnormal heart rhythms, preventing sudden death.
How can artificial intelligence be used in arrhythmia prediction?
Artificial intelligence analyzes big data to find patterns. This helps predict arrhythmias, allowing for early action and prevention.
What is the importance of community CPR and AED training?
Community training is key. It helps bystanders respond quickly and effectively in emergencies, improving survival rates.
What are the benefits of public access defibrillation programs?
Public access programs put AEDs in public areas. They let bystanders defibrillate people in cardiac arrest, boosting survival chances.
Reference
New England Journal of Medicine. Evidence-Based Medical Insight. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMra1708126
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK558923/