
Learn the key steps: How do doctors use cardiomyopathy exclusion diagnostic methods to rule out the condition? Be informed. Nearly 1 in 500 adults worldwide have cardiomyopathy. This condition makes it hard for the heart to pump blood. Accurate diagnosis is key for good treatment.
Diagnosing heart muscle disease is complex. Our guide helps you understand the diagnostic approaches for cardiomyopathy. Healthcare experts use cardiomyopathy diagnostic criteria to find the condition and plan treatment.
Key Takeaways
- Understanding the importance of accurate cardiomyopathy diagnosis.
- Overview of the diagnostic methods used for cardiomyopathy exclusion.
- The role of cardiomyopathy diagnostic criteria in effective diagnosis.
- Steps to develop a treatment plan for heart muscle disease.
- The importance of early detection in managing cardiomyopathy.
Understanding Cardiomyopathy: Definition and Types
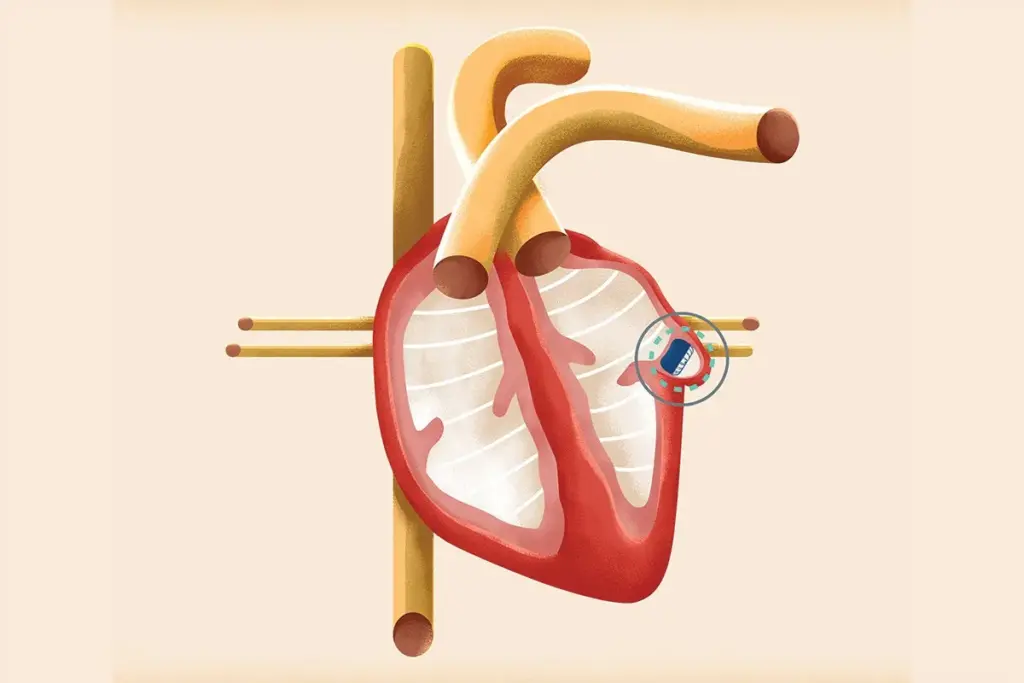
To manage cardiomyopathy well, knowing its definition and types is key. It’s a heart muscle disease that can cause serious problems if not treated right. We’ll look at what cardiomyopathy is and its main types.
What Defines Cardiomyopathy as a Heart Muscle Disease
Cardiomyopathy affects the heart muscle, changing its structure and function. It can make the heart muscle enlarged, thickened, or stiff. This makes it hard for the heart to pump blood well. It can be primary, just affecting the heart, or secondary, caused by another disease.
Primary Classifications: Dilated, Hypertrophic, Restrictive, and Arrhythmogenic
Cardiomyopathy is mainly split into four types based on heart muscle issues:
- Dilated Cardiomyopathy: The heart chamber gets too big, making it hard to pump blood.
- Hypertrophic Cardiomyopathy: The heart muscle gets too thick, blocking blood flow.
- Restrictive Cardiomyopathy: The heart muscle gets stiff, making it hard for chambers to fill.
- Arrhythmogenic Cardiomyopathy: Fatty tissue replaces heart muscle, leading to dangerous heart rhythms.
Knowing these types is vital for cardiomyopathy testing techniques and using the right cardiomyopathy diagnostic criteria. Accurate diagnosis is essential for effective treatment and better patient outcomes.
The Importance of Accurate Diagnosis and Exclusion
Getting a correct diagnosis for cardiomyopathy is very important. This heart muscle disease can cause serious health problems if not treated right. The right diagnosis helps start the right treatment and avoid bad outcomes.
Consequences of Missed Diagnosis
If cardiomyopathy is not caught, it can lead to big problems. Patients might not get the care they need. This can make their heart disease worse, leading to heart failure, irregular heartbeats, and even sudden death. It also causes worry and uncertainty for patients and their families.
Diagnosing heart muscle disorders is challenging, often requiring multiple tests to distinguish them from other conditions. Doctors have to figure out if it’s cardiomyopathy or something else like heart valve problems or blockages in the heart’s blood vessels.
Benefits of Proper Exclusion in Patient Management
Knowing that a patient doesn’t have cardiomyopathy is just as important. It makes patients feel better and avoids extra tests and worry. It also helps doctors focus on other possible causes and treat them properly.
Testing for cardiomyopathy involves many steps. Doctors use special criteria to rule out cardiomyopathy and find other conditions. This helps them make the best choices for patient care.
|
Diagnostic Approach |
Benefits |
Consequences of Missed Diagnosis |
|---|---|---|
|
Comprehensive Diagnostic Workup |
Accurate diagnosis and exclusion of cardiomyopathy |
Disease progression and increased risk of complications |
|
Differential Diagnosis |
Distinguishes cardiomyopathy from other heart conditions |
Unnecessary treatment and monitoring for incorrect diagnoses |
|
Application of Exclusion Criteria |
Informed decision-making for patient care |
Inappropriate management and possible harm to patients |
Initial Clinical Assessment for Suspected Cardiomyopathy
Diagnosing cardiomyopathy starts with checking symptoms and medical history. This first step is key to spotting possible cases and deciding on more tests.
Key Symptoms and Warning Signs
People with cardiomyopathy might feel short of breath, fatigued, or have palpitations. Spotting these signs early is vital for quick action. Other signs include chest pain, dizziness, and leg swelling.
It’s important to record the patient’s symptoms in detail. This helps doctors figure out if cardiomyopathy is likely and what tests to do next.
Family History Evaluation
Looking into a patient’s family history is key, as some cardiomyopathies run in families. We look for patterns of heart disease and sudden deaths.
This helps doctors understand the patient’s risk. It also guides decisions on genetic tests and screenings for family members.
Physical Examination Findings
The physical exam can show signs of cardiomyopathy, like murmurs or heart failure signs. Doctors check for signs like jugular venous distension and peripheral edema.
These findings, along with symptoms and family history, help doctors decide if cardiomyopathy is likely. They then choose the right tests to confirm it.
Basic Diagnostic Tests in Cardiomyopathy Evaluation
Basic tests are key in checking for cardiomyopathy. They give important info on heart function. These tests help find heart muscle diseases and guide more tests.
Electrocardiogram (ECG) Patterns
An electrocardiogram (ECG) is a simple test that shows the heart’s electrical activity. It can spot heart issues like arrhythmias or signs of heart damage. For example, deep and narrow Q waves might show hypertrophic cardiomyopathy. Low voltage QRS complexes could point to dilated cardiomyopathy.
“The ECG is vital in the first steps of checking for cardiomyopathy,” it gives quick info on the heart’s electrical signals.
Chest X-ray Findings
A chest X-ray is another basic tool for checking cardiomyopathy. It shows the heart’s size and shape and if there’s lung congestion. In cardiomyopathy, it might show an enlarged heart or signs of heart failure like pulmonary edema.
- Cardiomegaly (enlarged heart) points to dilated cardiomyopathy
- Pulmonary venous congestion shows heart failure
- Pleural effusions hint at advanced heart disease
Laboratory Blood Tests
Laboratory blood tests are vital in diagnosing cardiomyopathy. They help find causes like metabolic disorders or inflammation. Key tests include:
- Complete Blood Count (CBC) to check for anemia or infection
- Thyroid function tests for thyroid disorders
- Cardiac biomarkers like troponin and BNP for heart injury or stress
- Electrolyte levels to spot imbalances affecting heart function
By looking at ECG, chest X-ray, and blood tests, doctors get a full picture of the patient’s health. This helps them decide on the next steps or treatment.
Cardiomyopathy Exclusion Diagnostic Methods: A Complete Approach
Getting a correct diagnosis for heart muscle disorders is key. A detailed strategy helps rule out cardiomyopathy. This ensures patients get the right treatment.
Systematic Diagnostic Algorithms
Diagnostic algorithms are vital for checking cardiomyopathy. They start with a detailed look at the patient’s health history and physical check-up. They look for symptoms like chest pain and shortness of breath. They also check family history and risk factors.
Next, basic tests like ECGs and chest X-rays are used. These tests help spot heart issues or patterns that might suggest cardiomyopathy.
Ruling Out Secondary Causes
It’s important to find and fix secondary causes of cardiomyopathy. This means looking at things like heart disease and high blood pressure. It also includes checking for metabolic disorders.
- Coronary artery disease evaluation
- Assessment of hypertension and its effects on the heart
- Investigation of metabolic disorders, such as diabetes
By looking at these factors, doctors can make a better diagnosis and treatment plan.
Establishing Definitive Exclusion Criteria
Setting clear criteria for ruling out cardiomyopathy is a detailed process. It involves clinical checks, tests, and looking at the patient’s overall health. This helps doctors be sure if it’s not cardiomyopathy.
Advanced imaging like MRI or CT scans can also help. They give detailed views of the heart, aiding in diagnosis.
By using a thorough and systematic way to diagnose, doctors can give patients the right care. This improves their health and life quality.
Echocardiography as a Primary Diagnostic Tool
Echocardiography is key in finding and ruling out cardiomyopathy. It gives detailed views of the heart’s structure and how it works. This non-invasive test is vital for checking the heart’s health and making treatment plans.
2D and 3D Echocardiography Techniques
Two-dimensional (2D) echocardiography is a basic tool in cardiology. It lets doctors see the heart’s chambers, walls, and valves. This helps spot problems linked to cardiomyopathy.
Three-dimensional (3D) echocardiography adds more detail. It gives a clearer picture of the heart’s shape and function. Using both 2D and 3D echocardiography helps doctors understand the heart better. This is key in finding and diagnosing cardiomyopathy.
Doppler and Tissue Doppler Imaging
Doppler echocardiography looks at blood flow and speed in the heart. It shows how well the heart is working and if there are problems with valves or the heart muscle. Tissue Doppler Imaging (TDI) checks how fast the heart muscle moves. These tools are great for spotting heart function issues linked to cardiomyopathy.
Strain and Speckle Tracking Analysis
Strain imaging and speckle tracking are advanced tests. They measure how much the heart muscle moves. These tests help find heart problems early, even when they’re not obvious.
|
Echocardiographic Technique |
Diagnostic Utility in Cardiomyopathy |
|---|---|
|
2D Echocardiography |
Assessment of cardiac structure and chamber size |
|
3D Echocardiography |
Detailed evaluation of cardiac anatomy and function |
|
Doppler Echocardiography |
Evaluation of blood flow and valvular function |
|
Tissue Doppler Imaging (TDI) |
Assessment of myocardial velocity and function |
|
Strain Imaging and Speckle Tracking |
Quantification of myocardial deformation and function |
Advanced Cardiac Imaging Techniques
Advanced cardiac imaging has changed how we diagnose cardiomyopathy. These techniques give us detailed views of the heart. This helps doctors make better diagnoses and treatment plans.
Cardiac MRI: The Gold Standard for Tissue Characterization
Cardiac MRI is now the top choice for looking at heart tissue. It shows the heart’s details clearly. This lets doctors see if there’s fibrosis or inflammation.
Cardiac MRI is great because it shows the heart’s shape, function, and tissue without harmful radiation. It’s perfect for keeping an eye on patients over time.
Cardiac CT: Role in Structural Assessment
Cardiac CT is also key in diagnosing cardiomyopathy. It quickly checks the heart’s structure, like the coronary arteries and chambers. We use it to find out if there’s disease in the coronary arteries or other heart issues.
Cardiac CT is good at showing the coronary arteries clearly. This helps find coronary artery disease. It’s important for diagnosing and treating cardiomyopathy.
Nuclear Imaging Modalities
Nuclear imaging, like SPECT and PET, is also important. They show how well the heart is working and if it’s damaged. This helps us understand how cardiomyopathy affects the heart.
We use nuclear imaging to find out where the heart might not be getting enough blood. This helps us decide the best treatment for each patient. It’s very helpful in planning care for those with cardiomyopathy.
Genetic Testing in Cardiomyopathy Diagnosis
Genetic testing is key in diagnosing cardiomyopathy. It helps find genetic mutations linked to heart muscle diseases. This leads to early treatment and screening of family members.
When to Consider Genetic Testing
Genetic testing is advised for those with cardiomyopathy, with a family history or unclear diagnosis. It’s also for family members of someone with a known genetic mutation.
Choosing to get tested depends on several things. These include the type of cardiomyopathy, specific symptoms, and how it affects treatment and family screening.
|
Indication |
Description |
|---|---|
|
Family History |
A history of cardiomyopathy or sudden cardiac death in first-degree relatives. |
|
Unclear Diagnosis |
When the diagnosis is uncertain or when distinguishing between different cardiomyopathies. |
|
Known Mutation |
Family members of a person with a known cardiomyopathy-causing mutation. |
Interpretation of Genetic Results
Understanding genetic test results needs expertise. A positive result can show family risk and guide treatment. But, a negative result doesn’t mean you’re safe from cardiomyopathy.
Genetic counseling is vital. It helps people grasp their test results and their health and family implications.
Cascade Family Screening
Cascade screening tests family members of someone with a known genetic mutation. It finds those at risk early, allowing for timely monitoring and treatment.
Good cascade screening needs a team effort. It includes genetic counseling, medical checks, and ongoing support for family members.
Invasive Diagnostic Procedures
Invasive diagnostic procedures are key in diagnosing cardiomyopathy. They give detailed info about the heart’s health. This info is not available from non-invasive tests alone.
Cardiac Catheterization and Hemodynamic Assessment
Cardiac catheterization is a major invasive test for cardiomyopathy. It involves putting a catheter into the heart to check its function. This test measures heart pressures and output, helping to find the right treatment.
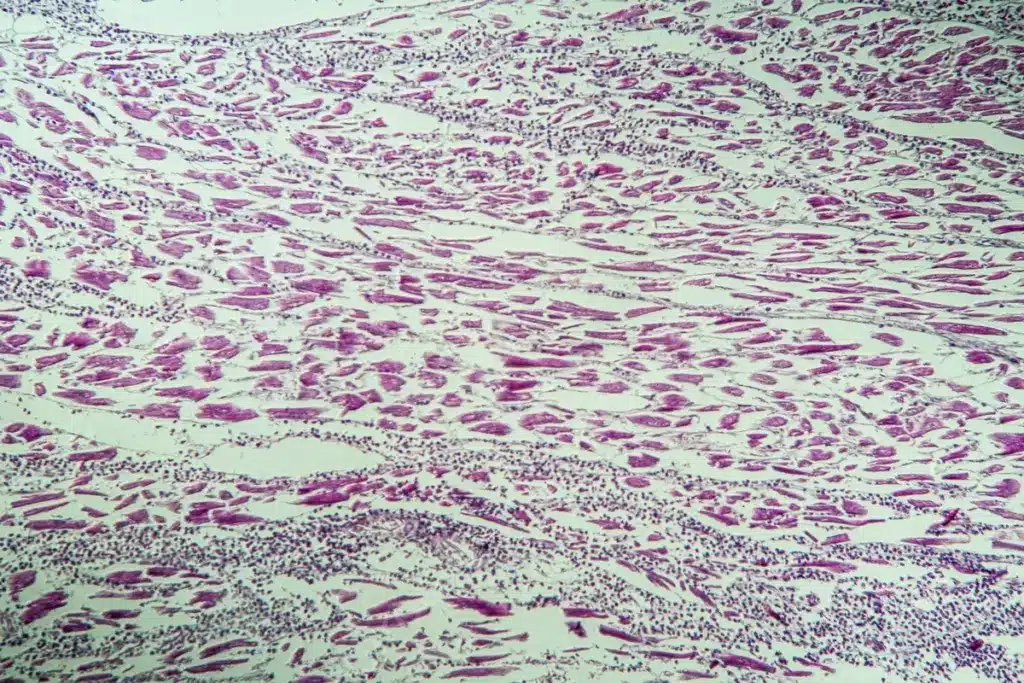
Endomyocardial Biopsy: Indications and Limitations
Endomyocardial biopsy takes a small heart tissue sample for study. It’s great for diagnosing certain cardiomyopathies. But, it carries risks and is not always needed.
Doctors usually choose this test when other tests don’t give clear results. Or when they suspect a treatable condition.
Electrophysiological Studies
Electrophysiological studies (EPS) are used for cardiomyopathy, focusing on arrhythmias. They involve catheters to record heart electrical activity. This helps diagnose arrhythmogenic cardiomyopathy and plan treatments like catheter ablation.
In conclusion, invasive tests are essential for managing cardiomyopathy. They offer detailed insights into the heart’s health. This helps tailor treatments to each patient’s needs.
Differential Diagnosis of Heart Muscle Disorders
Cardiomyopathy can be confused with other heart conditions. This makes it important to tell them apart. Doing so helps in choosing the right treatment for patients.
Distinguishing Cardiomyopathy from Coronary Artery Disease
Coronary artery disease (CAD) and cardiomyopathy share similar symptoms. Yet, CAD is caused by blockages in arteries, while cardiomyopathy is a disease of the heart muscle. We use different tests to tell them apart.
Key Diagnostic Features:
- CAD: Significant blockages in arteries, history of heart attacks
- Cardiomyopathy: No major blockages, heart muscle disease signs
|
Diagnostic Feature |
CAD |
Cardiomyopathy |
|---|---|---|
|
Coronary Artery Stenosis |
Present |
Absent |
|
Myocardial Infarction History |
Common |
Less Common |
|
Left Ventricular Function |
Variable |
Often Impaired |
Valvular Heart Disease vs. Cardiomyopathy
Valvular heart disease can look like cardiomyopathy because both can cause heart failure. But, valvular disease is about faulty valves, while cardiomyopathy is about heart muscle problems.
Differential Diagnostic Considerations:
- Severity of valve disease
- Presence of primary myocardial disease
- Response to valve-specific treatments
Congenital Heart Defects Mimicking Cardiomyopathy
Certain heart defects at birth can be mistaken for cardiomyopathy. It’s key to do a detailed check to tell them apart.
Diagnostic Approaches:
- Echocardiography to check heart structure and function
- Cardiac MRI for detailed heart tissue look
- Genetic testing in some cases
In conclusion, figuring out heart muscle disorders needs a detailed approach. This includes clinical checks, imaging, and other tests to accurately diagnose cardiomyopathy and other heart issues.
Special Considerations in Pediatric Cardiomyopathy Diagnosis
Diagnosing cardiomyopathy in kids is different from adults. Kids’ hearts are growing, and their cardiomyopathy can be caused by genetics, metabolic issues, or heart defects at birth.
Age-Specific Diagnostic Approaches
When diagnosing cardiomyopathy in children, we must know how their hearts are supposed to grow. We use special ways to measure heart size and function. We also look at how old the child is when we read the test results.
- Echocardiography: The main tool for checking the heart in kids.
- Electrocardiogram (ECG): Helps find heart rhythm problems linked to cardiomyopathy.
- Cardiac MRI: Shows detailed heart images, useful in tricky cases.
Congenital and Metabolic Causes
It’s key to find out why a child has cardiomyopathy. Some causes are genetic or metabolic, like fatty acid disorders or mitochondrial myopathies.
Key considerations include:
- Family history of heart problems or sudden death.
- Signs of syndromes or other health issues.
- Results of metabolic tests.
Long-term Monitoring Strategies
Children with cardiomyopathy need ongoing care to watch how their heart does. They’ll have regular heart tests and might need other scans.
Good long-term care means watching for heart failure or rhythm problems. It also means helping the child grow and live well.
Diagnostic Challenges in Specific Cardiomyopathy Types
Cardiomyopathy is hard to diagnose because it shows up in many ways. Each type needs its own special look to get it right. Knowing this helps doctors make accurate diagnoses.
Hypertrophic Cardiomyopathy: Beyond Wall Thickness
Hypertrophic cardiomyopathy (HCM) makes the heart muscle thick. This can block blood flow and increase the risk of sudden death. To diagnose HCM, doctors look at symptoms, family history, and other signs.
- Symptoms such as chest pain, shortness of breath, and syncope
- Family history of HCM or sudden cardiac death
- Echocardiographic findings, including left ventricular hypertrophy and outflow tract obstruction
Dilated Cardiomyopathy: Identifying Reversible Causes
Dilated cardiomyopathy (DCM) makes the heart chambers big. This makes it hard for the heart to pump blood well. Finding out why this happens is a big challenge in DCM.
Key considerations include:
- Coronary artery disease assessment
- Nutritional deficiencies (e.g., thiamine or selenium deficiency)
- Toxic exposures (e.g., alcohol or certain chemotherapeutic agents)
Arrhythmogenic Cardiomyopathy: Early Detection Strategies
Arrhythmogenic cardiomyopathy (ACM) has the heart muscle replaced by fibrofatty tissue. This can cause dangerous heart rhythms. Finding it early is key and involves several steps.
Diagnostic approaches for ACM include:
- Electrocardiogram (ECG) abnormalities, such as T-wave inversion
- Signal-averaged ECG for detecting late potentials
- Cardiac MRI to visualize fibrofatty infiltration
Restrictive Cardiomyopathy: Diagnostic Pearls
Restrictive cardiomyopathy (RCM) is rare. It makes the heart walls stiff, making it hard to fill the heart during diastole. Spotting RCM early is important, mainly in those with heart failure symptoms and a normal ejection fraction.
Key diagnostic features include:
|
Diagnostic Feature |
Description |
|---|---|
|
Bi-ventricular hypertrophy |
Thickening of both ventricles |
|
Dip-and-plateau pattern |
Characteristic pressure tracing in cardiac catheterization |
|
Preserved systolic function |
Normal ejection fraction despite diastolic dysfunction |
Cost Considerations and Insurance Coverage in the US
It’s important for patients to know about insurance and costs when getting tested for cardiomyopathy. The money needed for tests can affect how easily patients get the care they need.
Insurance Coverage for Diagnostic Testing
In the US, insurance plans differ in what they cover for cardiomyopathy tests. Most plans pay for basic tests like ECGs and echocardiograms. But, more detailed tests like MRI or CT scans might need extra approval.
We suggest patients check their insurance to see what’s covered. Talking to doctors can help figure out the best tests for their case.
Key factors to consider when reviewing insurance coverage:
- Types of diagnostic tests covered
- Requirements for pre-authorization
- Out-of-network coverage
- Deductibles and co-payments
Out-of-Pocket Expenses and Financial Resources
Even with insurance, patients might face big costs for cardiomyopathy tests. These can include deductibles, co-payments, and uncovered tests.
There are ways to help with these costs. Some testing places offer financial help or lower fees based on income. Patient groups also offer support and resources.
Talking to doctors about money worries is key to finding solutions.
Navigating Prior Authorizations for Advanced Imaging
Getting approval for advanced tests like MRI or CT scans can be tough. It’s hard for both patients and doctors.
To make it easier, doctors should:
- Make sure all needed info is correct and complete
- Send in requests on time
- Check with insurance on their requests
Understanding the process and working with doctors can help patients get tests faster.
Emerging Technologies in Cardiomyopathy Diagnosis
New technologies are making it easier to diagnose cardiomyopathy. These tools help us understand the disease better. They also make it easier to care for patients.
Artificial Intelligence in Cardiac Imaging
Artificial intelligence (AI) is changing cardiac imaging. It makes analysis more precise and detailed. AI can:
- Automate image analysis, reducing mistakes
- Spot patterns that humans might miss
- Find small changes in the heart’s structure and function
AI in cardiac imaging will make diagnoses more accurate and fast. For example, AI can quickly and accurately analyze echocardiograms, MRIs, and CT scans. This means doctors can act faster.
Novel Biomarkers and Liquid Biopsies
New biomarkers are key for catching cardiomyopathy early. Liquid biopsies, which check blood or other fluids, are also promising. They can:
- Find genetic changes linked to cardiomyopathy
- Watch how the disease grows and how it responds to treatment
- Help tailor treatments to each patient
Using new biomarkers and liquid biopsies is a big step forward. It could lead to earlier treatment and better results for patients.
Wearable Technology for Continuous Monitoring
Wearable devices are getting better at tracking the heart. They can:
- Keep an eye on heart rate and rhythm as it happens
- Spot irregular heartbeats and other issues
- Collect data for long-term tracking and study
Wearable tech is improving care by letting patients monitor their heart at home. This could mean fewer hospital visits and a better life for patients.
Conclusion: Optimizing the Diagnostic Journey in Cardiomyopathy
Diagnosing cardiomyopathy needs a detailed approach. We’ve shown how to use different methods to find the right diagnosis. Cardiac imaging is key in this process.
Knowing about cardiomyopathy and its types is essential. A systematic approach helps doctors rule out other causes. This leads to better care for patients.
Techniques like echocardiography and cardiac MRI are very important. They help doctors get accurate results. This leads to better care for those with cardiomyopathy.
New technologies like artificial intelligence and wearable devices will help us more. They will make diagnosing and treating cardiomyopathy even better. By keeping up with these advancements, we can improve care for patients.
FAQ
What is cardiomyopathy and how is it diagnosed?
Cardiomyopathy is a heart muscle disease. It can be found through echocardiography, cardiac MRI, and genetic tests. We use many methods to find cardiomyopathy, starting with a check-up and tests, then advanced imaging.
What are the different types of cardiomyopathy?
There are main types of cardiomyopathy: dilated, hypertrophic, restrictive, and arrhythmogenic. Each type needs its own way to be diagnosed.
Why is accurate diagnosis and exclusion of cardiomyopathy important?
Getting the right diagnosis is key for treatment. Missing it can lead to serious problems like heart failure. It helps us know who needs special care.
What is the role of echocardiography in diagnosing cardiomyopathy?
Echocardiography is a main tool for finding cardiomyopathy. It shows how the heart works and looks. We use different types of echocardiography to check the heart.
How does genetic testing contribute to cardiomyopathy diagnosis?
Genetic tests find genes linked to cardiomyopathy. This helps us catch it early. We test people with a family history or certain signs.
What are the benefits of advanced cardiac imaging techniques in cardiomyopathy diagnosis?
New imaging like cardiac MRI gives us detailed heart info. This helps us diagnose and manage cardiomyopathy better.
How do we distinguish cardiomyopathy from other heart conditions?
We use different tests and studies to tell cardiomyopathy apart from other heart issues. This includes looking at symptoms, test results, and images.
What are the challenges in diagnosing cardiomyopathy in children?
Diagnosing cardiomyopathy in kids is tricky. We need to think about age and other causes. We also watch them closely over time.
How do emerging technologies improve cardiomyopathy diagnosis?
New tech like AI in imaging and wearable devices helps us diagnose better. They help us find and treat cardiomyopathy more effectively.
What are the cost considerations for cardiomyopathy diagnosis in the US?
The cost of diagnosing cardiomyopathy in the US varies. We help patients understand their insurance and what they might have to pay.
What is the role of cardiac MRI in cardiomyopathy diagnosis?
Cardiac MRI is a key tool for diagnosing cardiomyopathy. It shows the heart’s structure and function. It’s great for seeing tissue damage.
How do we establish definitive exclusion criteria for cardiomyopathy?
We use a detailed plan to rule out cardiomyopathy. This includes looking at test results and images to find other causes.
Reference
Centers for Disease Control and Prevention. Evidence-Based Medical Insight. Retrieved from https://www.cdc.gov/heartdisease/cardiomyopathy.htm










