
Nearly 1 in 500 adults has cardiomyopathy. This is a condition where the heart muscle weakens. It makes it harder for the heart to pump blood.
It’s important to know what not to do when you have this condition. We’ll help you understand what to avoid. This includes managing your treatment and making lifestyle changes.
Managing heart failure treatment is key to a better life. Knowing what to avoid helps. You can work with your doctor to create a care plan that’s right for you.
Learn the crucial mistakes to absolutely avoid when managing cardiomyopathy, especially regarding cardiomyopathy medication. Stay safe.
Key Takeaways
- Understand the importance of managing your treatment plan.
- Make necessary lifestyle adjustments to prevent complications.
- Work closely with your healthcare provider to develop a personalized care plan.
- Be aware of the pitfalls in managing cardiomyopathy.
- Learn how to improve your quality of life with cardiomyopathy.
Understanding Cardiomyopathy and Its Impact
Cardiomyopathy can greatly affect the heart’s function. It’s important to know the different types and their effects. This knowledge helps both patients and healthcare providers manage the condition better.
Types of Cardiomyopathy and Their Differences
There are several types of cardiomyopathy, each with its own characteristics. The main types are dilated cardiomyopathy, hypertrophic cardiomyopathy, and restrictive cardiomyopathy.
|
Type of Cardiomyopathy |
Characteristics |
Effects on Heart Function |
|---|---|---|
|
Dilated Cardiomyopathy |
Enlargement of the heart chambers, reducing the heart’s ability to contract and pump blood effectively. |
Reduced ejection fraction, leading to heart failure symptoms. |
|
Hypertrophic Cardiomyopathy |
Thickening of the heart muscle, potentially obstructing blood flow out of the heart. |
Obstruction of blood flow, leading to symptoms like chest pain and shortness of breath. |
|
Restrictive Cardiomyopathy |
Stiffening of the heart muscle, making it difficult for the heart chambers to fill with blood. |
Impaired diastolic function, leading to heart failure symptoms. |
How Cardiomyopathy Affects Your Heart Function

Cardiomyopathy can severely impair the heart’s ability to pump blood. This can lead to heart failure, where the heart can’t meet the body’s needs for blood and oxygen.
The heart’s pumping ability is compromised in cardiomyopathy. In dilated cardiomyopathy, the heart chambers enlarge, reducing contractility. In hypertrophic cardiomyopathy, thickened muscle obstructs blood flow. In restrictive cardiomyopathy, stiffened muscle impairs filling.
The Consequences of Ignoring Medical Advice
Not following medical advice for cardiomyopathy can quickly worsen the condition and increase serious risks. These include worsening heart failure, arrhythmias, and even sudden cardiac death. Following treatment plans and lifestyle recommendations is key to managing the condition effectively.
Key consequences of ignoring medical advice include:
- Worsening heart failure symptoms
- Increased risk of arrhythmias
- Reduced quality of life
- Increased risk of sudden cardiac death
Understanding cardiomyopathy and its impact helps patients work closely with healthcare providers. This collaboration is vital for managing the condition and improving quality of life.
Dangerous Medications to Avoid with Cardiomyopathy
Knowing which medications to avoid is key for those with cardiomyopathy. It helps prevent complications. A good approach includes knowing which drugs can make the condition worse.
Over-the-Counter Drugs That Can Worsen Heart Function
Some over-the-counter (OTC) drugs can harm the heart of cardiomyopathy patients. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen can cause fluid buildup. This makes the heart work harder and can worsen symptoms.
Also, decongestants in cold and allergy meds can increase blood pressure and heart rate. This puts extra strain on the heart. Always check with a doctor before taking OTC drugs.
Prescription Medications That May Exacerbate Symptoms
Some prescription drugs can also harm cardiomyopathy patients. For example, certain antidepressants and antiarrhythmic drugs can affect the heart. Always tell your doctor about your cardiomyopathy when starting new meds.
|
Medication Type |
Potential Risk |
|---|---|
|
NSAIDs |
Fluid retention, increased heart workload |
|
Decongestants |
Increased blood pressure and heart rate |
|
Certain Antidepressants |
Adverse effects on heart function |
Supplements and Herbal Remedies to Avoid
Even though they seem safe, some supplements and herbal remedies can be risky. Licorice root, for instance, can cause fluid buildup and potassium loss. Both are bad for the heart.
Talking to your doctor about any supplements or herbal remedies is important. This ensures they won’t harm your treatment plan for cardiomyopathy.
Cardiomyopathy Medication: What Not to Do
Managing cardiomyopathy well means using the right medicines and using them correctly. We’ll look at important things about cardiomyopathy medicine. This will help patients avoid problems.
Never Skip or Adjust Doses Without Medical Guidance
Changing doses without a doctor’s say can be very risky. Following your doctor’s advice on medication is key to keeping your heart healthy. Not listening to your doctor can make symptoms worse or even be deadly.
Avoiding Dangerous Medication Interactions
People with cardiomyopathy often take many medicines. This raises the risk of bad drug reactions. It’s vital to tell your doctor about all your medicines. This includes things you buy without a prescription, like vitamins or herbal products.
The Dangers of Abruptly Stopping Treatment
Stopping your medicine suddenly can cause big problems. It might make your heart failure worse or even lead to sudden death. Always keep taking your medicine as your doctor told you, even if you feel better. Changing your treatment should only be done with your doctor’s help.
Not Reporting Side Effects to Your Doctor
Telling your doctor about side effects is very important. Side effects can mean you need to change your medicine. Keep track of any side effects and talk to your doctor about them. This helps make sure your treatment is right for you.
|
Medication Management Tips |
Description |
|---|---|
|
Adhere to Prescribed Regimen |
Take medications exactly as prescribed by your healthcare provider. |
|
Report Side Effects |
Inform your doctor about any side effects you experience. |
|
Avoid Drug Interactions |
Disclose all medications and supplements to your healthcare provider. |
|
Do Not Stop Medication Abruptly |
Continue medication as prescribed; consult your doctor before making any changes. |
Managing Cardiomyopathy Medication Side Effects
Medications for cardiomyopathy can have side effects. It’s important to know about these to manage them well. Patients need to be aware of the side effects and when to ask for help.
Common Side Effects You Shouldn’t Ignore
Common side effects include dizziness, fatigue, and swelling in the legs and ankles. These signs show how your body reacts to the medicine.
Keep an eye on these side effects and tell your doctor if they change. Never ignore side effects that get worse or affect your daily life.
When to Seek Help for Adverse Reactions
Seek medical help right away for severe side effects like trouble breathing, chest pain, or severe dizziness. These could mean a serious reaction to the medicine.
If you have milder but ongoing side effects, talk to your doctor about changing your treatment plan.
Avoiding Self-Adjustment of Dosages
Don’t change your medication dose on your own. Changing it can cause dangerous complications, like making your cardiomyopathy worse or causing other health problems.
Always talk to your doctor before changing your medication.
Not Mixing Medications Without Professional Advice
Mixing medicines without advice can be harmful. Always tell your doctor about any other medicines, supplements, or herbal remedies you’re taking.
|
Medication Type |
Potential Interaction |
Precaution |
|---|---|---|
|
Blood Thinners |
Increased risk of bleeding |
Monitor INR levels closely |
|
Beta Blockers |
Enhanced effect on heart rate |
Regularly check heart rate and blood pressure |
|
Diuretics |
Electrolyte imbalance |
Monitor electrolyte levels |
By understanding the side effects of cardiomyopathy medication and working with your doctor, you can manage your condition well. This helps reduce risks.
Dietary Mistakes That Worsen Cardiomyopathy
For those with cardiomyopathy, what they eat matters a lot. A good diet helps manage symptoms and avoid problems.
High-Sodium Foods to Eliminate
Eating too much sodium can make your heart work harder. It’s key to cut down on sodium-rich foods like processed and packaged items.
Examples of high-sodium foods to limit or avoid:
- Processed meats (e.g., bacon, sausages)
- Canned goods (e.g., soups, vegetables)
- Packaged snacks (e.g., chips, pretzels)
- Restaurant and fast food
Why You Should Avoid Excessive Alcohol
Too much alcohol can harm your heart muscles, making cardiomyopathy worse. It’s best to limit or stop drinking alcohol to keep your heart healthy.
The risks associated with excessive alcohol consumption include:
- Increased heart rate and blood pressure
- Weakened heart muscles
- Potential for arrhythmias
Caffeine and Stimulants to Limit
Caffeine and stimulants can raise your heart rate and blood pressure. This can make cardiomyopathy symptoms worse. Be careful with how much caffeine and stimulants you consume.
Sources of caffeine and stimulants to be mindful of:
- Coffee and energy drinks
- Certain medications (e.g., decongestants)
- Some dietary supplements
Improper Fluid Management Mistakes
Managing fluids is very important for those with cardiomyopathy. Drinking too much or too little can cause problems.
Tips for proper fluid management:
- Monitor daily fluid intake
- Adjust fluid consumption based on activity level and climate
- Follow healthcare provider’s recommendations
Exercise and Physical Activity Restrictions
Exercise is key for health, but it’s different for those with cardiomyopathy. It’s important to be careful with physical activities. While exercise can help manage symptoms, some activities are too risky.
High-Intensity Workouts to Avoid
People with cardiomyopathy should stay away from high-intensity workouts. These can strain the heart too much. Activities like sprinting, heavy weightlifting, and high-impact aerobics can raise heart rate and blood pressure. This can lead to serious problems.
Examples of high-intensity activities to limit or avoid include:
- High-intensity interval training (HIIT)
- Competitive team sports that involve sudden bursts of energy
- Heavy resistance training without proper supervision
Competitive Sports That Pose Risks
Competitive sports can be risky for those with cardiomyopathy. The intense effort and stress of competition can harm the heart.
Talking to your healthcare provider about sports activities is key. They can help you understand the risks and make safe choices.
Warning Signs to Stop Activity Immediately
Knowing when to stop exercising is important. Look out for these warning signs:
- Chest pain or discomfort
- Severe shortness of breath
- Dizziness or fainting
- Rapid or irregular heartbeat
If you see any of these signs, stop exercising right away. Then, get medical help.
Not Exercising Without Medical Clearance
Always get medical clearance before starting or changing an exercise routine. Your healthcare provider can check your condition and suggest safe activities.
Always talk to your healthcare team before trying new or tough exercises. They can help keep your heart safe.
Harmful Lifestyle Habits with Cardiomyopathy
Lifestyle choices are key in managing cardiomyopathy. Some habits can really hurt your health. It’s important to know which daily habits can make your condition worse.
Smoking and Tobacco Use Dangers
Smoking and tobacco use are big risks for heart disease. They can hurt your heart even more if you have cardiomyopathy. These habits can make it harder for blood to reach your heart and raise your blood pressure. Quitting smoking is a big step towards better heart health.
Key risks associated with smoking and tobacco use:
- Increased heart rate and blood pressure
- Reduced blood flow to the heart
- Worsening of heart failure symptoms
- Increased risk of heart attack and stroke
Chronic Stress and Poor Sleep Patterns
Chronic stress and poor sleep can hurt your heart health. Stress can make your heart work harder, and bad sleep can make you tired and feel worse. Try stress-reducing activities like meditation or yoga, and keep a regular sleep schedule.
|
Stress Management Techniques |
Benefits |
|---|---|
|
Meditation |
Reduces stress and anxiety |
|
Yoga |
Improves flexibility and reduces stress |
|
Deep Breathing Exercises |
Lowers blood pressure and heart rate |
Extreme Temperature Exposure Risks
Extreme temperatures can be dangerous for people with cardiomyopathy. Both hot and cold can stress your heart. It’s important to stay safe in extreme weather by staying hydrated and avoiding hard work.
Heavy Lifting and Physical Straining
Heavy lifting and straining can be hard on your heart, which is bad for cardiomyopathy. Try to avoid lifting heavy things and doing hard activities to manage your symptoms and prevent problems.
Tips for avoiding heavy lifting and physical straining:
- Ask for help when lifting heavy objects
- Avoid bending or straining
- Take regular breaks to rest
- Engage in gentle exercises recommended by your healthcare provider
Specific Restrictions for Different Types of Cardiomyopathy
It’s important to know the unique traits of each cardiomyopathy type. This knowledge helps in managing the condition effectively. Each type needs a specific treatment approach and lifestyle changes.
Activities to Avoid with Hypertrophic Cardiomyopathy
Hypertrophic cardiomyopathy (HCM) makes the heart muscle thick. This can block blood flow. People with HCM should stay away from intense workouts and competitive sports. These can raise the risk of sudden heart death.
Here are some activities to avoid:
- High-intensity exercises and sprinting
- Contact sports that might hurt the chest
- Working out in very hot or dry places
Dilated Cardiomyopathy: Dangerous Practices
Dilated cardiomyopathy (DCM) makes the heart big but weak. It can’t pump blood well. People with DCM should avoid things that make their heart weaker or work harder.
Here are some practices to avoid:
- Drinking too much alcohol, which harms the heart
- Smoking and using tobacco, which damage the heart and blood vessels
- Not taking medicines or following treatment plans, which can worsen heart failure
Restrictive and Non-Compaction Cardiomyopathy Precautions
Restrictive cardiomyopathy (RCM) and left ventricular non-compaction cardiomyopathy (LVNC) are serious but less common. RCM makes the heart walls stiff. LVNC has deep pockets in the heart muscle.
Here are some precautions:
- Avoiding hard activities that could cause heart failure or irregular heartbeats
- Keeping an eye on fluid levels to avoid overload
- Following anticoagulation therapy to prevent blood clots
Arrhythmogenic Right Ventricular Cardiomyopathy Risks
Arrhythmogenic right ventricular cardiomyopathy (ARVC) replaces the right ventricle with fatty tissue. This can lead to dangerous heart rhythms. People with ARVC should be careful about activities that might trigger these rhythms.
Here are some risks to watch out for:
- High-intensity exercise that can cause arrhythmias
- Endurance sports that can make the condition worse
- Ignoring symptoms like palpitations or fainting, which need immediate medical help
To summarize, here’s a table of key restrictions for different cardiomyopathy types:
|
Cardiomyopathy Type |
Activities to Avoid |
Precautions |
|---|---|---|
|
Hypertrophic Cardiomyopathy (HCM) |
High-intensity exercises, competitive sports |
Avoid strenuous activities, extreme temperatures |
|
Dilated Cardiomyopathy (DCM) |
Excessive alcohol, smoking |
Adhere to medication, avoid heart strain |
|
Restrictive Cardiomyopathy (RCM) and Left Ventricular Non-Compaction Cardiomyopathy (LVNC) |
Strenuous activities |
Monitor fluid status, adhere to anticoagulation therapy |
|
Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC) |
High-intensity exercise, endurance sports |
Be aware of arrhythmia risks, report symptoms promptly |
Common Medication Management Mistakes
For those with cardiomyopathy, managing medications is more than just taking the right drugs. It’s also about avoiding common errors. Effective management includes several key aspects. If these are overlooked, it can lead to serious problems.
Not Maintaining an Updated Medication List
One big mistake is not keeping an updated list of medications. This list should include all prescription drugs, over-the-counter meds, and supplements. We suggest reviewing and updating this list with your healthcare provider at every visit. An up-to-date list helps avoid dangerous drug interactions and ensures all healthcare providers are informed.
Improper Storage of Heart Medications
Heart medications need proper storage to work well. Some need to be kept in a cool, dry place, while others may need refrigeration. Always follow the storage instructions from your pharmacist or healthcare provider to keep medications effective.
Taking Medications at Incorrect Times
Taking medications at the wrong time can reduce their effectiveness and increase side effects. We recommend setting reminders or using a pill box to stay on schedule. Being consistent is key to managing cardiomyopathy well.
Not Informing All Healthcare Providers About Your Condition
Telling all your healthcare providers about your cardiomyopathy and medications is vital. This includes dentists, specialists, and any new healthcare providers. Understanding your condition and medications helps prevent bad interactions and ensures coordinated care.
By avoiding these common mistakes, people with cardiomyopathy can manage their condition better. We encourage patients to work closely with their healthcare team to create a personalized medication plan.
Warning Signs That Require Immediate Medical Attention
It’s key to know the warning signs for cardiomyopathy that need quick medical help. Some symptoms can mean your condition is getting worse or a heart problem is coming.
Never Ignore Chest Pain or Breathing Difficulties
Chest pain or discomfort and trouble breathing are serious signs. They can mean a heart attack or acute heart failure, both urgent medical issues.
- Chest pain or tightness that spreads to the arm, neck, or jaw
- Shortness of breath or trouble breathing, even when resting
- Severe fatigue or weakness
Dangerous Levels of Swelling and Fluid Retention
Swelling in the legs, ankles, and feet, and sudden weight gain from fluid retention, show the heart isn’t pumping well. These signs need quick checking.
Fainting Episodes and Severe Dizziness
Fainting or near-fainting, and severe dizziness, can mean not enough blood is reaching the brain. This is often due to abnormal heart rhythms or severe cardiomyopathy.
Key symptoms to watch for include:
- Sudden loss of consciousness
- Lightheadedness or feeling like you might pass out
- Severe dizziness that doesn’t get better with rest
Irregular Heartbeat and Persistent Palpitations
Irregular heartbeats or palpitations that last or are severe can be a sign of dangerous arrhythmias. These can cause serious problems if not treated quickly.
It’s vital to get medical help if you notice:
- Rapid or irregular heartbeats
- Pounding in the chest
- Skipped beats or extra beats
Knowing these warning signs and getting medical help right away can greatly help those with cardiomyopathy.
Travel and Environmental Risks to Avoid
Traveling with cardiomyopathy means you need to watch out for certain environmental factors. These can make your heart condition worse. It’s important to know how different conditions can affect your heart health.
Air Travel Without Medical Clearance
Air travel can be tough for people with cardiomyopathy. The air pressure change and dry air on planes can cause dehydration. This can make your heart function worse. Always get medical clearance before flying.
Here are some tips for air travel:
- Drink lots of water to stay hydrated
- Wear loose clothes to avoid blood flow restrictions
- Get up and move often to prevent blood clots
High Altitude Exposure Dangers
High altitudes are risky for those with cardiomyopathy. The air has less oxygen, which strains the heart. Talk to your doctor before traveling to high places.
Here are some tips for high altitude travel:
- Acclimate slowly to higher elevations
- Watch how your body reacts to the altitude
- Avoid hard activities until you’re fully acclimated
Extreme Climate Risks
Extreme weather can be dangerous for people with cardiomyopathy. It makes your heart work harder, which can lead to problems. Take steps to protect your health in extreme climates.
|
Climate Condition |
Potential Risks |
Precautions |
|---|---|---|
|
Extreme Heat |
Dehydration, heatstroke |
Stay hydrated, avoid outdoor activities during peak heat |
|
Extreme Cold |
Increased blood pressure, heart strain |
Dress warmly, avoid sudden changes in temperature |
Traveling Without Adequate Medication Supply
Having enough medication is key when traveling with cardiomyopathy. Running out can cause serious health issues. Before you travel, make sure to:
- Pack enough medication for your trip and extra for delays
- Carry a list of your medications and dosages
- Tell your healthcare provider about your travel plans
By understanding and avoiding these risks, people with cardiomyopathy can travel safely. Always talk to your healthcare provider before traveling to make sure you’re prepared.
Emotional and Mental Health Pitfalls
The emotional toll of cardiomyopathy is often overlooked, but it’s a key part of our well-being. Living with a chronic heart condition can lead to big mental health challenges, like depression and anxiety.
Ignoring Depression and Anxiety Symptoms
Depression and anxiety are common in people with cardiomyopathy. Symptoms include feeling sad all the time, losing interest in things, and worrying too much about health. It’s important to spot these signs early and get help.
Common signs of depression and anxiety include:
- Changes in appetite or sleep patterns
- Difficulty concentrating
- Feelings of hopelessness or guilt
- Panic attacks or severe anxiety
Social Isolation and Lack of Support
Social isolation can make feelings of loneliness and depression worse. It’s key to keep in touch with family, friends, and support groups for emotional health.
Strategies to combat social isolation:
- Joining a cardiomyopathy support group
- Staying connected with loved ones through regular calls or visits
- Participating in online forums or communities
Unhealthy Coping Mechanisms to Avoid
Some people might turn to unhealthy coping, like substance abuse or avoiding problems. These can make mental health worse and should be avoided.
|
Unhealthy Coping Mechanism |
Healthier Alternative |
|---|---|
|
Substance abuse |
Seeking professional counseling |
|
Avoidance behaviors |
Engaging in stress-reducing activities like meditation or yoga |
|
Social withdrawal |
Connecting with support groups or loved ones |
Not Seeking Psychological Support When Needed
Seeking psychological support is a sign of strength, not weakness. Mental health professionals can offer valuable guidance and support to handle the emotional challenges of cardiomyopathy.
By recognizing the emotional and mental health pitfalls of cardiomyopathy, we can take steps to keep our well-being in check. It’s important to face these challenges head-on and seek the support we need.
Special Situations Requiring Extra Caution
Certain life circumstances, like pregnancy and adolescence, need extra care with cardiomyopathy. We must know the unique risks to give the best care.
Pregnancy Risks with Cardiomyopathy
Pregnancy is tough for women with cardiomyopathy. It can lead to complications during and after childbirth. We suggest close monitoring and careful management to reduce these risks.
|
Pregnancy Complications |
Risks |
Management Strategies |
|---|---|---|
|
Heart Failure |
Increased risk of heart failure due to increased blood volume |
Close monitoring of heart function, adjustment of medications |
|
Arrhythmias |
Increased risk of arrhythmias due to hormonal changes |
Regular ECG monitoring, anti-arrhythmic medications |
Children and Adolescents: Activities to Avoid
Children and teens with cardiomyopathy need guidance on physical activities. We advise against high-intensity sports and exercises that can strain the heart too much.
- Avoid competitive sports that involve high-intensity exercise
- Limit strenuous activities that can cause excessive fatigue
- Monitor for signs of heart strain or distress during exercise
Elderly Patients with Multiple Conditions: Medication Conflicts
Elderly patients with cardiomyopathy often have many health issues. They need careful management of their medications to avoid conflicts and interactions that can make their condition worse.
To avoid medication conflicts, we recommend:
- Maintaining an updated medication list
- Regularly reviewing medications with a healthcare provider
- Avoiding duplicate or interacting medications
Athletes: Dangerous Training Practices
Athletes with cardiomyopathy face a risk of sudden cardiac death from high-intensity training without proper precautions. We advise against:
- High-intensity training without medical clearance
- Ignoring symptoms of heart strain or distress during exercise
- Failing to report symptoms to a healthcare provider
By understanding these special situations and taking precautions, we can reduce the risks of cardiomyopathy. This helps improve patient outcomes.
Healthcare Management Mistakes to Avoid
Managing cardiomyopathy well is key for those living with it. It’s important to avoid common mistakes to improve life quality. This includes taking medicine, making lifestyle changes, and getting regular check-ups.
Skipping Follow-up Appointments
Going to regular check-ups with your doctor is vital. It helps keep track of your health and adjust treatments as needed. Missing these appointments can hide changes in your health, leading to serious problems.
- Schedule appointments in advance to ensure you don’t forget.
- Prepare a list of questions or concerns to discuss during your visit.
- Keep your healthcare provider informed about any changes in your symptoms or overall health.
Neglecting Regular Testing and Monitoring
Regular tests and monitoring are key in managing cardiomyopathy. Skipping them can make it hard to understand your health status. This makes it tough to make good treatment choices.
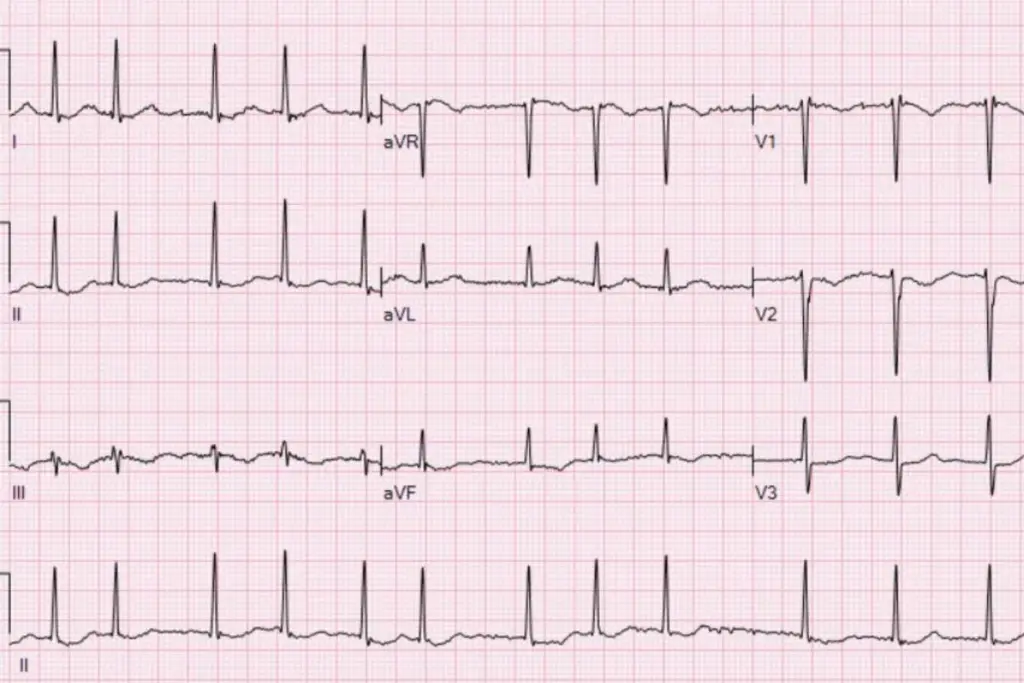
Common tests and monitoring include:
- Echocardiograms to assess heart function.
- Electrocardiograms (ECGs) to monitor heart rhythm.
- Blood tests to check for signs of heart failure or other complications.
Not Communicating Effectively With Your Care Team
Talking openly with your healthcare team is essential for good care. Not sharing your symptoms, concerns, or questions can cause misunderstandings. This can lead to poor management of your condition.
To communicate effectively:
- Be honest about your symptoms and how you’re feeling.
- Ask questions if you’re unsure about any aspect of your care.
- Keep a symptom journal to track changes and patterns.
Failing to Prepare for Medical Consultations
Preparing for medical consultations can greatly improve your care. Not preparing can mean missing chances to discuss important health issues or questions.
To prepare for your consultations:
- Write down your questions and concerns in advance.
- Bring a list of your current medications and dosages.
- Consider bringing a family member or friend for support.
Conclusion: Living Well While Avoiding Cardiomyopathy Risks
To manage cardiomyopathy well, it’s key to know the risks and take steps to avoid them. This way, people with cardiomyopathy can live active and happy lives. We help support patients with detailed management plans.
Dealing with cardiomyopathy means looking at many things, like medicine, lifestyle, and health care. By avoiding common errors and being proactive, people can lower cardiomyopathy risks. This helps improve their life quality, focusing on staying safe.
Good cardiomyopathy care needs a team effort. This includes following medicine plans and talking often with doctors. By doing this, people can lower the chance of serious problems.
FAQ
What are the most common mistakes to avoid when managing cardiomyopathy?
Don’t skip or change your medication without a doctor’s say-so. Ignore dietary rules at your own risk. Regular tests and talking to your care team are key.
What medications should be avoided with cardiomyopathy?
Some over-the-counter and prescription drugs can make symptoms worse. Always check with your doctor before trying new meds or supplements.
How can I manage cardiomyopathy medication side effects?
Tell your doctor about any side effects right away. Don’t change your doses on your own. Your doctor can adjust your treatment to lessen side effects.
What dietary restrictions are essential for managing cardiomyopathy?
Eat heart-healthy foods, avoiding too much salt, alcohol, and caffeine. Managing fluids is also important to avoid symptoms.
Can I exercise with cardiomyopathy?
Exercise is good, but be careful. Avoid high-intensity workouts and competitive sports. Always get a doctor’s okay before starting or continuing any exercise.
What lifestyle habits should I avoid with cardiomyopathy?
Stay away from smoking, tobacco, stress, and bad sleep. Also, avoid extreme temperatures and heavy lifting.
Are there specific restrictions for different types of cardiomyopathy?
Yes, each type needs its own approach. For example, hypertrophic cardiomyopathy means no high-intensity activities. Dilated cardiomyopathy means no heavy lifting.
How can I avoid common medication management mistakes?
Keep your medication list up to date. Store meds right, take them on time, and tell all doctors about your condition.
What are the warning signs that require immediate medical attention?
Watch for chest pain, trouble breathing, irregular heartbeat, fainting, and severe dizziness. Seek help right away if you see these signs.
Can I travel with cardiomyopathy?
Traveling with cardiomyopathy needs careful planning. Avoid flying without a doctor’s okay, high altitudes, and extreme weather. Make sure you have enough meds and talk to your doctor before you go.
How can I manage emotional and mental health with cardiomyopathy?
Recognize signs of depression and anxiety. Don’t isolate yourself. Seek help when you need it. Bad coping habits can make symptoms worse, so find healthy ways to deal with stress.
Are there special considerations for managing cardiomyopathy during pregnancy or in children and adolescents?
Yes, managing cardiomyopathy in pregnancy, childhood, or adolescence needs special care. Always talk to your doctor to create a personalized plan.
How can I avoid healthcare management mistakes?
Go to all follow-up appointments and tests. Talk well with your care team. Be ready for medical visits.
What are the best medications for managing cardiomyopathy?
The best meds manage symptoms, slow disease, and improve life quality. Common ones include beta-blockers, ACE inhibitors, and diuretics. The right one and dosage depend on your type and how severe it is.
How can I manage cardiomyopathy with medication?
Stick to your treatment plan, report any side effects, and avoid drug interactions. Work closely with your healthcare team to adjust your treatment as needed.
What are the latest advancements in cardiomyopathy medication?
New meds and therapies target specific disease mechanisms. They aim to improve symptoms, slow disease, and enhance life quality.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC12250813/





