Cardiovascular events can happen suddenly, like in cases of cardiac arrest. It’s important to know the feelings of a blocked artery in the leg to catch it early.
Peripheral artery disease (PAD) makes the arteries in the legs narrow or block. This leads to symptoms that need to be recognized to manage the condition well.
Knowing the signs of a blocked artery sensation is key. It helps people get medical help fast, which can save lives and improve health outcomes.
Key Takeaways
- Understanding PAD symptoms is key for early detection.
- A blocked artery in the leg can cause a lot of discomfort.
- Spotting the signs can lead to timely medical help.
- PAD symptoms include pain and discomfort in the legs.
- Early treatment can improve outcomes and save lives.
Understanding Peripheral Artery Disease (PAD)

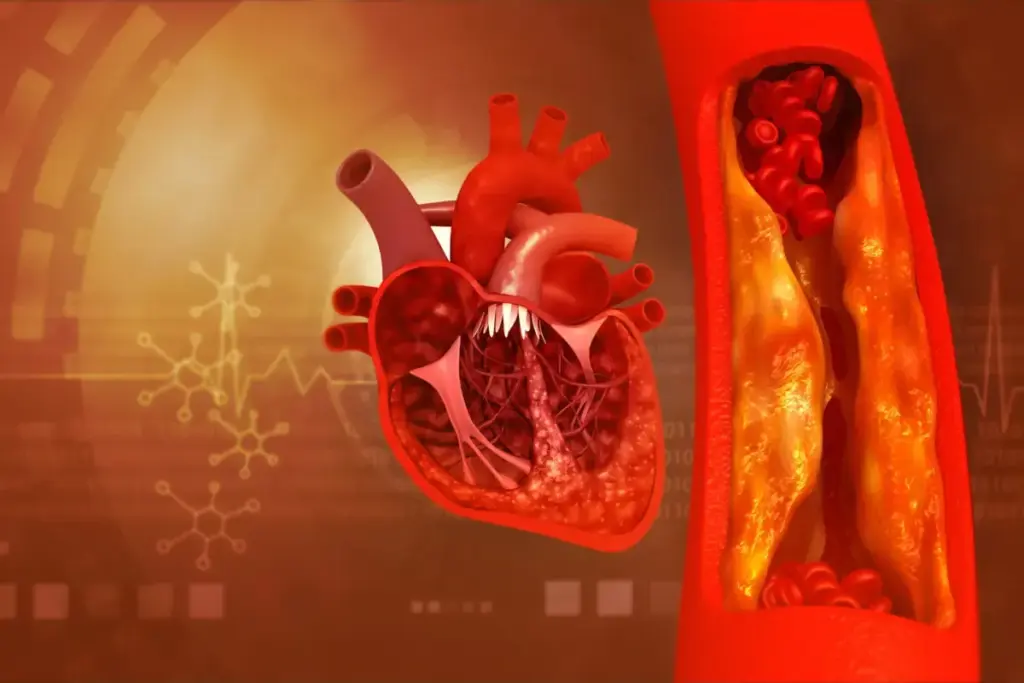
PAD, or Peripheral Artery Disease, is a condition where arteries in the legs narrow. This happens mainly because of atherosclerosis. Atherosclerosis is when plaque builds up in the walls of arteries.
Definition and Prevalence
PAD is a big health issue worldwide. It affects about 8.5 million people in the U.S. who are 40 or older. The more you age, the higher your risk of getting PAD.
Relationship to Atherosclerosis
Atherosclerosis causes PAD. Plaque made of fat, cholesterol, and other stuff narrows or blocks arteries. This problem is not just in the legs. It can also show that you might have heart disease.
Risk Factors
Many things can make you more likely to get PAD. These include:
- Smoking: It harms the blood vessels’ lining.
- Diabetes: High blood sugar damages blood vessels and nerves.
- High Blood Pressure: It damages the walls of arteries.
- High Cholesterol: Too much LDL cholesterol causes plaque.
- Obesity and Physical Inactivity: They harm your heart and blood vessels.
- Family History of PAD or Cardiovascular Disease: Your genes play a part.
Knowing these risk factors helps prevent and manage PAD. By tackling these issues, you can lower your chance of getting PAD and its complications.
Blocked Artery Sensation: The Primary Symptoms

Knowing the main symptoms of a blocked artery in the leg is key to better treatment. A blocked artery can cause pain, discomfort, and changes in skin color and temperature.
Initial Warning Signs
The first signs of a blocked artery in the leg include pain or discomfort when you walk. This pain goes away when you rest. You might also feel fatigue or heaviness in your legs.
Medical sources say symptoms can vary from mild to severe. They can include changes in skin color and temperature. Spotting these signs early is important for quick action.
How Symptoms Progress Over Time
As PAD gets worse, symptoms of a blocked artery get more serious. Pain may happen more often or even when you’re not moving. Skin might look paler or cooler to the touch.
|
Symptom |
Early Stage |
Advanced Stage |
|---|---|---|
|
Pain |
Intermittent claudication during activity |
Pain at rest, more frequent |
|
Skin Color/Temperature |
Mild changes, possibly unnoticed |
Noticeable paleness or coolness |
|
Other Symptoms |
Fatigue, heaviness in legs |
Non-healing wounds, significant mobility issues |
It’s important to understand how symptoms get worse. This helps manage PAD better and avoid more problems.
Common Symptoms of Blocked Arteries in Legs
Blocked leg arteries can cause discomfort and limit how well you can move. These signs are important for spotting Peripheral Artery Disease (PAD) early. Knowing them helps in getting the right medical help fast.
Pain and Discomfort Patterns
Pain or discomfort in the legs is a key symptom of blocked arteries. It often happens when you’re active, like walking or climbing stairs. This is because the muscles don’t get enough oxygen-rich blood.
The pain goes away when you rest, but comes back when you start moving again. Where the pain is felt can tell you where the blockage is. For example, pain in the buttock or thigh might mean a blockage in the thigh or hip. Calf pain could mean a blockage in the lower leg.
Temperature Changes in Affected Limbs
People with blocked leg arteries often feel their affected limb is cold. This is because there’s less blood flow to the area.
It’s not uncommon for one leg to feel colder than the other. Or, you might notice a big difference in temperature between the affected leg and the rest of your body.
Skin Color and Texture Changes
Blocked arteries can also change how your skin looks and feels on the affected leg. The skin might look pale or blue because it’s not getting enough blood.
In serious cases, the skin can get thin, shiny, and might even develop slow-healing ulcers or sores. Hair loss on the affected leg is also a common sign.
Mobility and Functional Limitations
The pain and discomfort from blocked leg arteries can really limit how much you can move. It makes even simple tasks hard.
As the condition gets worse, walking short distances can become a big challenge. This not only hurts your physical health but also affects your mental well-being and quality of life.
|
Symptom |
Description |
|---|---|
|
Pain/Discomfort |
Occurs during activity, relieved by rest |
|
Temperature Changes |
Feeling of coldness in the affected limb |
|
Skin Changes |
Pale or blue-tinged skin, thin and shiny texture |
|
Mobility Issues |
Limited ability to perform daily activities |
“Patients often report pain when walking or climbing stairs, coldness, and changes in skin color.” This shows how different the symptoms of blocked arteries in the legs can be.
It’s important to know these symptoms to catch PAD early. If you or someone you know is showing these signs, seeing a healthcare professional is key for the right diagnosis and treatment.
Intermittent Claudication: The Hallmark Symptom
Leg pain when you’re active is called intermittent claudication. It’s a sign of Peripheral Artery Disease (PAD). This symptom is key for diagnosing PAD and seeing how it affects people’s lives.
Defining the Cramping Sensation
Intermittent claudication is a cramping or aching in the legs during activity, like walking. This pain is usually predictable and happens after a certain distance or exertion level.
The pain can range from mild to severe. It’s so bad that some people have to stop and rest.
Activity-Related Triggers
The pain from intermittent claudication happens when muscles need more oxygen than blocked arteries can provide. Walking uphill, climbing stairs, or brisk walking are common triggers.
Other activities like cycling or heavy lifting can also cause pain. But walking is the most common cause.
Relief Patterns and Timeframes
Resting is the best way to make the pain go away. Stopping and resting for a few minutes usually helps.
The time it takes for the pain to go away varies. But usually, it’s within 2-5 minutes of rest. This pattern is what makes intermittent claudication different from other leg pains.
Critical Limb Ischemia: Advanced Warning Signs
Critical limb ischemia is a serious form of peripheral artery disease. It shows clear warning signs. This stage means the blood flow to the limbs is very low.
Rest Pain Characteristics
Rest pain is a key symptom of critical limb ischemia. It’s a severe pain in the toes or feet that doesn’t go away. This pain happens even when you’re not moving and doesn’t get better by changing your position.
Nocturnal Pain Patterns
Nocturnal pain, or night pain, is another sign of critical limb ischemia. It can really mess up your sleep. The pain gets worse when you’re lying down because blood flow is even lower.
People often find relief by hanging their legs over the bed or walking around.
Tissue Damage and Non-Healing Wounds
Critical limb ischemia can cause tissue damage and non-healing wounds. The lack of blood flow makes it hard for the body to heal. This leads to ulcers or sores that won’t heal.
These wounds can get infected and cause serious problems if not treated right. Non-healing wounds are a big warning sign of advanced limb ischemia.
In summary, critical limb ischemia is a serious condition that needs quick medical help. Spotting the warning signs like rest pain, night pain, and tissue damage is key to getting the right treatment.
How Symptoms Differ Based on Blockage Location
Symptoms of PAD change a lot based on where the blockage is in the leg. The blockage’s location affects the areas it impacts and how bad the symptoms are.
Aortoiliac Disease (Upper Leg/Hip)
Aortoiliac disease blocks blood flow in the aorta and iliac arteries. These arteries supply blood to the hips and legs. People with this disease often feel pain in their hips, buttocks, and thighs, mainly when they’re active.
A medical expert said, “Aortoiliac occlusive disease is a big reason for lower leg problems, causing a lot of pain when walking.” Claudication is the pain felt when walking or exercising because of poor blood flow.
Femoropopliteal Disease (Thigh/Knee)
Femoropopliteal disease blocks the femoral and popliteal arteries. These arteries are key for blood to the thighs and knees. People with this disease might feel pain or cramping in their thighs or calves when they walk or do other activities.
A study found, “Femoropopliteal lesions are a common cause of intermittent claudication, significantly impacting patients’ quality of life.”
Tibial and Peroneal Disease (Lower Leg/Foot)
Tibial and peroneal disease blocks arteries below the knee. It affects the lower legs and feet. Symptoms include pain in the calves or feet, even when not moving, and are linked to more serious PAD.
A medical expert said, “Tibial artery disease can cause severe leg problems, needing quick medical help to avoid losing tissue.”
In summary, where the blockage is in the artery greatly affects PAD symptoms and how severe they are. Knowing these differences is key for the right diagnosis and treatment.
Patient Experiences: What People Report Feeling
Having a blocked artery in the leg can feel very different for everyone. Symptoms can range from a little discomfort to a lot of pain.
It’s important for both patients and doctors to understand these feelings. This helps manage the condition better.
Descriptions of Early Symptoms
In the early stages of peripheral artery disease (PAD), people might feel mild and occasional sensations. These can include:
- Achiness or cramping in the legs during physical activity
- Numbness or tingling sensations
- Coldness in the lower leg or foot
These symptoms can be easily overlooked or thought to be caused by something else. It’s key for people to know the signs of PAD.
Advanced Disease Sensations
As PAD gets worse, the feelings can get stronger and last longer. People often say they feel:
- Severe pain in the legs, even when they’re not moving
- Significant changes in skin color or texture
- Non-healing wounds or ulcers on the feet or legs
Critical limb ischemia, a severe form of PAD, can cause a lot of pain and serious problems if not treated quickly.
Impact on Daily Activities
PAD symptoms can really affect how people do everyday things. Even simple tasks like walking or climbing stairs can be hard because of pain or discomfort.
People often have to change their lifestyle. This includes:
- Reducing physical activity levels
- Avoiding certain activities that trigger pain
- Managing pain through medication or other interventions
Knowing how PAD affects daily life is key to finding good ways to manage it.
Distinguishing PAD from Other Conditions
Getting a correct diagnosis of Peripheral Artery Disease (PAD) is important. It involves looking at symptoms and differentiating it from other diseases. PAD symptoms can be similar to those of other vascular and non-vascular diseases.
Neuropathy vs. Vascular Pain
Diagnosing PAD can be tricky because of its similar symptoms to neuropathy. Neuropathy, often linked to diabetes, causes pain, numbness, and tingling in the legs. But, neuropathy pain is not always linked to physical activity.
PAD pain, on the other hand, is often triggered by walking or exercise. It gets better with rest.
Venous vs. Arterial Insufficiency
Venous insufficiency can also cause leg pain and swelling, similar to PAD. But, venous insufficiency pain is worse after standing for a long time. It also comes with varicose veins and skin changes.
PAD symptoms, caused by arterial blockages, are different. They include pain when walking (intermittent claudication).
Musculoskeletal Pain Differences
Musculoskeletal pain, from arthritis or muscle strain, can also be mistaken for PAD. But, musculoskeletal pain usually affects specific joints or muscles. It doesn’t always get better with rest like PAD does.
To correctly diagnose PAD, a detailed medical history, physical exam, and tests are needed. By looking at the nature, timing, and triggers of leg pain, doctors can tell PAD apart from other conditions. This helps in giving the right treatment.
When to Seek Medical Attention
It’s important to know when to get medical help for PAD. This can prevent serious problems.
Warning Signs That Require Immediate Care
Look out for these signs and get help right away: severe pain in your legs or feet, changes in skin color or temperature, or sores that won’t heal.
Immediate care is key if you see:
- Severe leg pain at rest
- Skin ulcers or gangrene
- A big change in leg color or temperature
- More pain or cramping in the legs when walking
Complications of Untreated Blockages
Not getting medical help on time can cause big problems. This includes critical limb ischemia, which might need amputation if not treated.
Critical limb ischemia is a serious issue. It happens when arteries are blocked a lot, cutting off blood to the limbs. This can cause a lot of pain, tissue loss, and might even lead to amputation.
Knowing the dangers of untreated PAD and spotting warning signs early can really help. It can make a big difference for those affected.
Diagnostic Process for Suspected Artery Blockage
Figuring out if a leg artery is blocked needs a few steps. First, doctors do a physical check. Then, they use non-invasive tests and sometimes advanced imaging. This detailed process helps find PAD and plan the best treatment.
Physical Examination Findings
The first step is a physical check. Doctors look for weak pulses in the legs, cool skin, and slow nail growth. They also check for slow-healing wounds, which can mean less blood flow.
Key findings during a physical examination may include:
- Decreased or absent pulses in the feet or legs
- Lower limb pallor or cyanosis
- Coolness to the touch
- Poor capillary refill
- Muscle atrophy or weakness
Non-Invasive Tests
Non-invasive tests help confirm PAD and its severity. The Ankle-Brachial Index (ABI) is a key test. It compares ankle and arm blood pressure to show PAD levels.
Other tests include:
- Doppler ultrasound to check blood flow and find blockages
- Treadmill testing to see how far you can walk and how symptoms change
- Segmental pressure measurements to find where the blockage is
Advanced Imaging Options
Sometimes, detailed images are needed. Angiography uses dye to show artery details. It’s great for planning treatments.
Other options are:
- Computed Tomography Angiography (CTA)
- Magnetic Resonance Angiography (MRA)
These methods help doctors see the arteries clearly. This makes diagnosing and treating artery blockages more accurate.
Treatment Options for Blocked Leg Arteries
Dealing with blocked leg arteries needs a mix of lifestyle changes, medical treatments, and sometimes surgery. The right treatment depends on how bad the blockage is, the patient’s health, and their medical history.
Lifestyle Modifications
Changing your lifestyle is often the first step in treating blocked leg arteries. These changes can help manage symptoms and slow the disease’s progress.
- Smoking cessation: Quitting smoking is key because smoking greatly increases the risk of Peripheral Artery Disease (PAD).
- Exercise therapy: Regular walking can improve blood flow and lessen symptoms.
- Dietary changes: Eating a diet low in saturated fats, cholesterol, and sodium can help manage the condition.
- Weight management: Keeping a healthy weight reduces leg strain and improves blood flow.
Medication Approaches
Medicines are vital in managing blocked leg artery symptoms and preventing complications.
- Antiplatelet agents: Medications like aspirin or clopidogrel prevent blood clots.
- Cholesterol-lowering medications: Statins are often prescribed to control high cholesterol.
- Blood pressure medications: Keeping blood pressure in check is critical for PAD patients.
Interventional Procedures
For serious blockages, interventional procedures are needed.
- Angioplasty: A procedure where a balloon is used to widen the blocked artery.
- Stenting: A stent is placed to keep the artery open after angioplasty.
- Atherectomy: Removing plaque from the artery.
Surgical Solutions
In severe cases, surgery may be needed to bypass the blocked artery section.
|
Treatment Option |
Description |
Benefits |
|---|---|---|
|
Lifestyle Modifications |
Changes in daily habits and lifestyle |
Manages symptoms, slows disease progression |
|
Medication Approaches |
Use of medications to manage symptoms and risk factors |
Reduces risk of complications, manages symptoms |
|
Interventional Procedures |
Minimally invasive procedures to widen or clear blocked arteries |
Restores blood flow, relieves symptoms |
|
Surgical Solutions |
Surgical bypass or repair of blocked arteries |
Provides a more permanent solution for severe blockages |
Living with PAD: Managing Symptoms Daily
Living with PAD means you need a plan for pain, foot care, and daily activities. It’s about managing symptoms, moving better, and feeling better overall.
Pain Management Strategies
It’s key to manage PAD pain to stay mobile and feel less discomfort. You can use medicine, change your lifestyle, and try other therapies.
- Medications like antiplatelet agents and pain relievers help.
- Changing your lifestyle, like exercising and quitting smoking, is important.
- Therapies like acupuncture and physical therapy can also help.
Pain Management Techniques
|
Technique |
Description |
Benefits |
|---|---|---|
|
Exercise |
Regular physical activity tailored to the individual’s condition |
Improves circulation, reduces pain |
|
Smoking Cessation |
Quitting smoking to reduce vascular constriction |
Enhances blood flow, reduces pain |
|
Medication |
Use of prescribed medications for pain relief |
Reduces pain, improves mobility |
Foot Care Importance
Foot care is vital for PAD patients to avoid ulcers and infections. Daily checks, clean feet, and the right shoes are key.
Daily Foot Inspection means looking for cuts, sores, or color changes. These signs can mean poor circulation or infection.
Adaptive Techniques for Daily Activities
Adjusting daily activities helps manage PAD symptoms. This means pacing yourself, taking breaks, and using aids when needed.
- Pacing activities to avoid overexertion.
- Using assistive devices like canes or walkers to reduce strain on affected limbs.
- Modifying exercise routines to include low-impact activities.
By using these strategies, people with PAD can manage their symptoms better. This improves their quality of life.
Preventing Arterial Blockages in the Legs
Arterial blockages in the legs can be prevented by making healthy lifestyle choices and managing risk factors. Understanding what causes Peripheral Artery Disease (PAD) is key. Taking steps to prevent it can greatly lower your risk.
Lifestyle Factors
Lifestyle is very important in preventing arterial blockages. Regular physical activity is essential. It improves circulation and heart health. Aim for at least 30 minutes of moderate exercise daily.
Eating a healthy diet is also critical. Eat lots of fruits, vegetables, whole grains, and lean proteins. Avoid foods high in saturated fats, cholesterol, and sodium to prevent atherosclerosis and PAD.
- Eating foods high in omega-3 fatty acids, like salmon and walnuts, can reduce inflammation.
- Keeping a healthy weight reduces leg strain and improves circulation.
- Quitting tobacco is key, as smoking is a major risk factor for PAD.
Medical Management of Risk Factors
Managing health conditions is also vital in preventing arterial blockages. This includes controlling high blood pressure and diabetes. Both can damage blood vessels and lead to PAD.
Medicines can help manage these conditions. For example, drugs for high blood pressure and antiplatelet agents to prevent blood clots. Regular check-ups with healthcare providers are important to keep these conditions under control.
- Work with your healthcare provider to manage your blood sugar levels if you have diabetes.
- Take medications as prescribed to control high blood pressure and cholesterol levels.
- Regular check-ups can help identify any changes in your condition early on.
Combining healthy lifestyle choices with effective medical management can greatly reduce the risk of arterial blockages in the legs. This proactive approach not only prevents PAD but also improves overall health and well-being.
Conclusion
Knowing about a blocked artery in the leg is key to catching Peripheral Artery Disease (PAD) early. Symptoms like pain when walking and numbness are warning signs. They mean you should see a doctor right away.
These signs are important because they show PAD is happening. PAD is caused by blocked arteries and is linked to many risk factors. To manage it, you need to change your lifestyle, take medicine, and sometimes have surgery.
By dealing with blocked artery feelings and PAD, you can lower your risk. This summary shows how important it is to know about PAD and act fast. It’s all about making smart health choices and getting help when you need it.
FAQ
What are the common symptoms of peripheral artery disease (PAD)?
PAD symptoms include pain in the legs, thighs, or hips when walking. You might also feel coldness or numbness in your legs or feet. Skin color or texture changes are other signs.
How does a blocked artery in the leg feel like?
A blocked artery in the leg can cause pain, cramping, or aching. This happens when you walk or exercise. You might also feel coldness, numbness, or tingling.
What is intermittent claudication?
Intermittent claudication is a PAD symptom. It’s a cramping or aching feeling in the legs during activity. It goes away when you rest.
Can PAD cause pain at rest?
Yes, in advanced PAD, pain can happen even when you’re not moving. It feels like a burning or aching in your legs or feet.
How is PAD diagnosed?
Doctors use physical exams, medical history, and tests to diagnose PAD. Tests include the ankle-brachial index (ABI), Doppler ultrasound, and angiography.
What are the treatment options for blocked leg arteries?
Treatment for blocked leg arteries includes lifestyle changes and medications. Procedures like angioplasty or stenting are also options. Sometimes, surgery is needed.
Can lifestyle changes help manage PAD symptoms?
Yes, lifestyle changes can help manage PAD symptoms. Regular exercise, quitting smoking, and eating healthy are key.
What is the importance of foot care in PAD management?
Foot care is vital in managing PAD. It helps prevent wounds, infections, and other complications. People with PAD are at higher risk for foot problems.
Can PAD be prevented?
While some risk factors can’t be changed, like age or family history, others can be managed. Lifestyle changes like regular exercise, healthy diet, and not smoking can reduce PAD risk.
What are the complications of untreated PAD?
Untreated PAD can lead to serious problems. These include critical limb ischemia, gangrene, amputation, and increased risk of heart attack and stroke.
How can I manage pain associated with PAD?
Managing PAD pain involves medications, alternative therapies like acupuncture, and lifestyle changes. Regular exercise and stress reduction are important.
Is it normal for one foot to be colder than the other?
A big temperature difference between your feet could mean PAD or other circulatory issues. It’s best to see a healthcare professional for an evaluation.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4696061/








