It’s important to know about rare heart conditions to help patients. We look into these uncommon diseases, their traits, and the help available for those who have them.
These rare conditions need detailed care and focus. Our goal is to offer top-notch healthcare and support to patients worldwide. By studying these rare heart issues, we hope to highlight their complexities and challenges.
Discover the rarest heart condition disease. Learn amazing facts about unique cardiac issues and how medical experts treat them effectively.
Key Takeaways
- Understanding rare heart conditions is key to the best patient care.
- These conditions need thorough and specialized medical care.
- Support for patients with uncommon cardiac diseases is essential.
- World-class healthcare is vital for treating rare heart conditions.
- International patients can get advanced medical treatments and support services.
Understanding Rare Heart Conditions

Rare heart conditions affect many people worldwide. They are hard to diagnose and treat. These conditions, though rare, have a big impact on health.
To tackle rare heart conditions, we need to know what they are. Rare diseases, like heart diseases, are not common. They affect the heart’s structure or function.
Definition and Classification of Rare Diseases
Rare heart diseases come in many types. They can be classified by cause, symptoms, or where in the heart they occur. This helps doctors diagnose and treat them better.
Some rare heart conditions are genetic. Others may be caused by the environment or a mix of both. Knowing this helps in finding the right treatment.
Classifying rare heart diseases is complex. It involves many factors like symptoms, genetic mutations, and biomarkers. This is key to creating effective treatments and improving care.
Epidemiology and Public Health Impact
Studying rare heart conditions is important for public health. Rare diseases, including heart conditions, affect millions globally. In the U.S., millions live with a rare disease, many of which are heart-related.
Knowing how common rare heart conditions are helps plan health care. It guides public health efforts and raises awareness. It also shows the need for specialized care and support.
Looking into rare heart conditions helps us understand the challenges they pose. It’s essential for research, better diagnosis, and effective treatments. This knowledge is key to helping patients and improving health care systems.
The Rarest Heart Condition Disease

Uhl’s anomaly is one of the rarest heart conditions. It affects the right ventricle in a unique way. This condition means the right ventricle might not have any or very little muscle, leading to serious health issues.
Pathophysiology and Anatomical Features
Uhl’s anomaly is a birth defect. It makes the right ventricle mostly made of fibrous tissue, with almost no muscle cells. This makes the right ventricle unable to pump blood well.
This condition happens when the right ventricular muscle doesn’t develop right during fetal development. This results in a thin-walled right ventricle that can easily get bigger and not work right. It often comes with other heart problems, making it harder to diagnose and treat.
Clinical Presentation and Diagnosis
People with Uhl’s anomaly can show different symptoms. Some might not have any symptoms at all, while others might have severe heart failure or irregular heartbeats. Symptoms can include feeling tired, short of breath, and having an irregular heartbeat. These symptoms usually start in late teens or early twenties.
To diagnose Uhl’s anomaly, doctors use imaging tests like echocardiography, cardiac MRI, and angiography. These tests help see the condition’s unique features, like the missing or thin right ventricular muscle.
Early diagnosis is key for treating Uhl’s anomaly well. Treatment aims to ease symptoms and prevent serious problems like heart failure and irregular heartbeats. Sometimes, surgery or a heart transplant might be needed.
Barth Syndrome: A Rare X-Linked Cardiac Disorder
Barth Syndrome is a rare heart condition that mainly affects males. It’s caused by a unique genetic issue. This condition has a big impact on heart health.
Genetic Basis and Inheritance Pattern
Barth Syndrome comes from a problem with the TAZ gene on the X chromosome. This leads to a lack of the tafazzin enzyme. This enzyme is key for cardiolipin metabolism. Because of this, males are mostly affected, while females can carry the gene without showing symptoms.
We’ll dive deeper into how the TAZ gene affects cardiolipin and heart function.
|
Genetic Aspect |
Description |
|---|---|
|
Gene Involved |
TAZ gene on X chromosome |
|
Inheritance Pattern |
X-linked recessive |
|
Primary Effect |
Deficiency in tafazzin enzyme |
Clinical Manifestations and Management
People with Barth Syndrome often have a weak heart, muscle issues, and low white blood cells. To manage this, doctors use a mix of heart care, physical therapy, and ways to prevent infections.
We’ll look at how these treatments help improve life for those with Barth Syndrome.
Getting a diagnosis early is key to managing Barth Syndrome. Knowing the genetic and clinical aspects helps doctors create better treatment plans. This way, they can meet the complex needs of these patients.
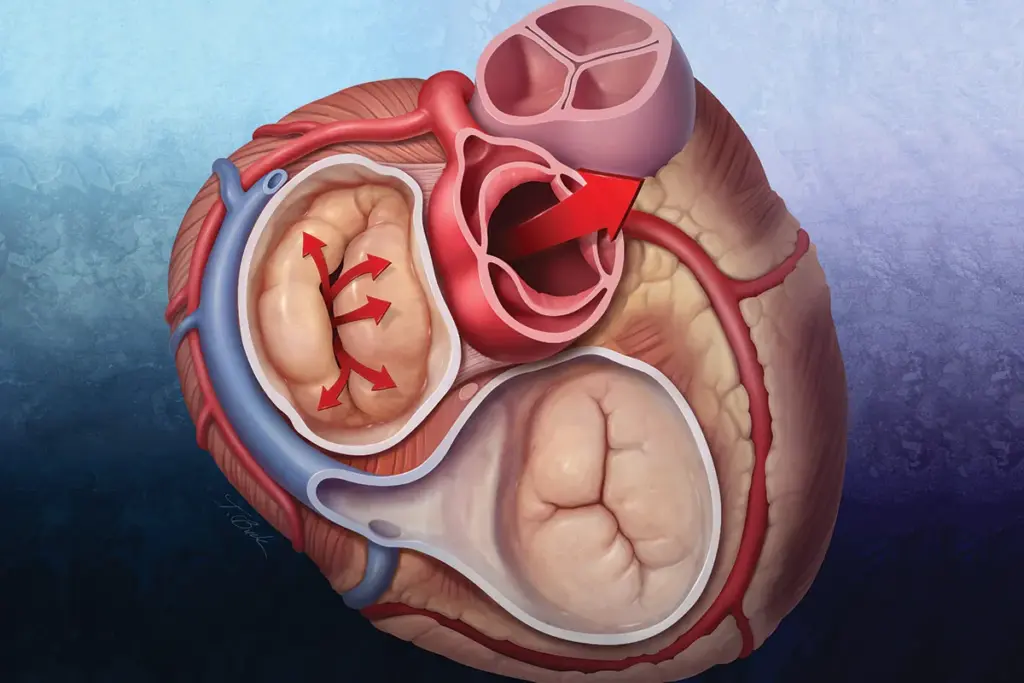
Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC)
ARVC is one of the rarest heart diseases. It mainly affects the right ventricle. This condition causes the right ventricle to change, leading to dangerous heart rhythms.
Genetic Basis and Pathogenesis
ARVC is linked to genes that help hold heart cells together. When these genes mutate, heart cells can’t stick together right. This leads to the changes seen in ARVC.
Genetics and environment play a big role in ARVC. It can start at any age, but usually shows up in teens or young adults.
Diagnosis and Risk Stratification
Finding ARVC can be hard because it shows up differently in everyone. Doctors use a mix of tests, including MRI and genetic tests, to diagnose it.
Doctors look at how likely someone is to have a serious heart problem. They check how well the right ventricle works, if someone has ever fainted, and genetic markers.
|
Diagnostic Criteria |
Major Criteria |
Minor Criteria |
|---|---|---|
|
Structural or Functional Abnormalities |
Severe dilatation or dysfunction of the right ventricle |
Mild dilatation or dysfunction of the right ventricle |
|
Tissue Characterization |
Presence of fibrofatty replacement on biopsy |
Repolarization abnormalities on ECG |
|
Arrhythmias |
History of sustained ventricular tachycardia |
History of non-sustained ventricular tachycardia |
Knowing how to diagnose and manage ARVC is key. It helps doctors take care of patients with this rare heart condition.
Restrictive Cardiomyopathy
Restrictive cardiomyopathy is a rare heart disease that affects the ventricles. It makes the heart work less efficiently. The ventricular walls become stiff, making it hard for the heart to fill with blood during diastole.
Etiology and Classification
This condition can be caused by genetic disorders, diseases like amyloidosis, or storage diseases like hemochromatosis. It’s classified based on its cause, which can be genetic or due to systemic diseases.
There are different types of restrictive cardiomyopathy, depending on the cause. For example, amyloidosis is a common cause. It leads to amyloid fibrils depositing in the heart tissue.
Diagnostic Approach and Management
Diagnosing restrictive cardiomyopathy involves several steps. These include clinical evaluation, imaging studies, and hemodynamic assessment. Echocardiography is key in checking for diastolic dysfunction and ruling out other heart failure causes.
The goal of managing restrictive cardiomyopathy is to improve symptoms and quality of life. Treatment may include diuretics, medications for arrhythmias, and therapies for the underlying disease.
|
Diagnostic Tool |
Key Findings in Restrictive Cardiomyopathy |
|---|---|
|
Echocardiography |
Diastolic dysfunction, restrictive filling pattern |
|
Cardiac MRI |
Late gadolinium enhancement, assessment of myocardial infiltration |
|
Endomyocardial Biopsy |
Histological evidence of myocardial disease (e.g., amyloidosis) |
It’s important for healthcare providers to understand how to diagnose and manage restrictive cardiomyopathy. This ensures the best care for patients with this rare heart condition.
Eisenmenger Syndrome
Eisenmenger syndrome is a serious condition linked to certain heart defects. It causes high blood pressure in the lungs and other health issues. We will look into how it works, its effects over time, and how doctors manage it today.
Pathophysiology and Natural History
Eisenmenger syndrome happens when a heart defect leads to too much blood flow to the lungs. This causes high blood pressure in the lungs. Over time, the defect starts to work in the opposite way, leading to cyanosis and other problems.
As the condition worsens, patients face serious health issues and a high risk of death. It’s important to understand how it works to help manage it better.
Modern Management Strategies
Today, doctors use a team approach to treat Eisenmenger syndrome. They use medicines to lower blood pressure in the lungs and improve life quality. They also suggest lifestyle changes and sometimes surgery. New treatments like pulmonary vasodilators help patients feel better and move more easily.
Dealing with Eisenmenger syndrome requires careful monitoring and a personalized treatment plan. Doctors focus on managing related problems and supporting patients to improve their health.
Cardiac Amyloidosis
Cardiac amyloidosis is a rare condition where amyloid proteins build up in the heart. This leads to a problem called restrictive cardiomyopathy. It makes the heart work poorly, causing serious health issues if not treated.
We see cardiac amyloidosis as a complex issue. It needs a deep understanding of its types and how it works to find good treatments. The amyloid proteins in the heart disrupt its function, causing various symptoms.
Types and Molecular Mechanisms
There are different types of cardiac amyloidosis, like AL and TTR amyloidosis. AL amyloidosis is linked to abnormal light chain proteins. TTR amyloidosis is caused by transthyretin protein, which can be inherited or occur naturally.
The disease happens when proteins misfold and stick together, forming amyloid fibrils. These fibrils harm the heart tissue, disrupting its structure and function.
Emerging Diagnostics and Therapeutics
Diagnosing cardiac amyloidosis uses imaging like echocardiography and MRI, along with biopsy and genetic tests. New tests and biomarkers are being developed for early detection and understanding the disease.
Treatment for cardiac amyloidosis is getting better, focusing on the disease’s cause. For AL amyloidosis, treatments include chemotherapy and stem cell transplants. TTR amyloidosis is managed with TTR stabilizers and gene silencers, showing promise in trials.
We’re moving towards personalized medicine for cardiac amyloidosis. This aims to improve patient outcomes and quality of life. As research continues, we expect better and more targeted treatments for this rare condition.
Hypoplastic Left Heart Syndrome (HLHS)
Hypoplastic Left Heart Syndrome (HLHS) is a rare heart condition. It affects the left side of the heart. This condition is caused by the underdevelopment of key parts of the left ventricle, valves, and aorta.
Embryology and Anatomical Features
HLHS happens when the left side of the heart doesn’t form right during fetal development. This leads to a small left heart. The left heart can’t pump blood to the body, making it very dangerous.
The heart in HLHS is small or missing on the left side. The mitral valve is often blocked or missing. The right ventricle must pump blood to both the lungs and the body.
Staged Surgical Approach
Managing HLHS requires a series of surgeries over time. These surgeries aim to use the right ventricle for blood circulation.
The first surgery, the Norwood procedure, is done soon after birth. It creates a new aorta and connects it to the right ventricle. It also sets up a shunt for lung blood flow.
Later surgeries, like the Glenn and Fontan procedures, are done when the child is older. They help blood flow directly to the lungs without going through the right ventricle.
Even with these surgeries, HLHS patients need ongoing care. They face risks and may need more surgeries later in life.
Brugada Syndrome: A Rare Electrical Heart Disorder
Brugada syndrome is one of the rarest heart conditions. It affects the heart’s electrical activity. This genetic disorder can cause dangerous arrhythmias, making it vital to diagnose and manage well.
Genetic and Molecular Basis
Brugada syndrome is linked to mutations in the SCN5A gene. This gene controls the sodium channel in the heart. Mutations here can disrupt the heart’s electrical flow. Not everyone with the mutation will show symptoms, making diagnosis tricky.
The genetics of Brugada syndrome are complex. It involves many genes and environmental factors. Scientists are working hard to understand it better. They aim to find better ways to diagnose and treat it.
Diagnosis and Risk Stratification
Diagnosing Brugada syndrome requires an electrocardiogram (ECG), clinical checks, and sometimes genetic tests. The Brugada sign on an ECG is key. But, this sign can be fleeting, needing repeated tests.
It’s important to figure out the risk level for Brugada syndrome. Those at high risk might need an implantable cardioverter-defibrillator (ICD). We look at factors like past fainting, family history of sudden death, and specific ECG patterns to decide.
|
Risk Factor |
Description |
Management Strategy |
|---|---|---|
|
History of Syncope |
Fainting spells that may indicate arrhythmias |
Consider ICD implantation |
|
Family History of Sudden Cardiac Death |
Presence of sudden cardiac deaths in close relatives |
Close monitoring and potentially ICD |
|
Characteristic ECG Pattern |
Specific changes on the electrocardiogram |
Monitoring and potentially medication |
It’s key to understand Brugada syndrome to give the right care. By using genetic knowledge, clinical checks, and advanced tests, we can help those with this rare heart disorder.
Ebstein’s Anomaly: A Rare Congenital Tricuspid Valve Defect
Ebstein’s anomaly is one of the rarest heart conditions. It affects the heart’s structure in a unique way. This condition causes problems with the tricuspid valve and the right ventricle.
It leads to different symptoms and outcomes in patients. This makes it a complex condition to manage.
Anatomical Abnormalities and Classification
Ebstein’s anomaly changes the tricuspid valve and the right ventricle. The right ventricle becomes “atrialized.” This can cause issues like tricuspid regurgitation and right-sided heart failure.
Doctors classify Ebstein’s anomaly based on how severe it is and if it’s combined with other heart problems. Knowing the details of each case helps decide the best treatment.
Surgical Techniques and Outcomes
Many patients with Ebstein’s anomaly need surgery. The main surgeries are fixing or replacing the tricuspid valve and reducing the right atrium’s size.
Thanks to advances, surgery for Ebstein’s anomaly has gotten better. Now, doctors focus on personalized care and long-term monitoring. Here’s a look at how surgery is doing:
|
Surgical Technique |
Success Rate |
Complication Rate |
|---|---|---|
|
Tricuspid Valve Repair |
85% |
10% |
|
Tricuspid Valve Replacement |
90% |
15% |
|
Right Atrium Reduction |
80% |
5% |
These results show the need for a customized approach to treating Ebstein’s anomaly. Each patient’s situation is unique.
Pediatric Rare Heart Conditions and Their Management
Pediatric rare heart conditions are a big challenge for doctors. They need special care from start to finish. These uncommon heart conditions need a detailed plan to help young patients the most.
Neonatal Presentation and Diagnosis
Finding rare heart disease types in newborns is hard. Symptoms are subtle, and the heart is complex. Finding it early is key to better survival and life quality.
We use top-notch tests like echocardiography and cardiac MRI to spot these conditions. Genetic tests help find the root cause and guide treatment.
Long-term Care and Transition to Adult Services
Managing rarest cardiovascular diseases in kids is more than just the first treatment. It takes a team of experts to meet the child’s changing needs.
When kids grow up, we focus on smooth care transition. We teach them and their families about their condition and treatment. This helps them get the right care in the adult system.
By focusing on the patient and using new cardiac care, we can help kids with rare heart conditions. We support them as they become adults.
Research Advances in Rare Cardiovascular Diseases
Research is making big strides in rare heart diseases, giving hope to patients. We’re seeing major progress in understanding and treating these conditions. This is thanks to ongoing clinical trials, registries, and new treatments.
Current Clinical Trials and Registries
Clinical trials and registries are key in learning more about rare heart diseases. They help find new treatments, understand how diseases work, and improve patient care. For example, studies on Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC) and Barth Syndrome are giving us important insights.
Some key benefits of current clinical trials and registries include:
- Improved understanding of disease progression and outcomes
- Identification of novel therapeutic targets
- Enhanced patient care through evidence-based medicine
- Facilitation of collaborative research across institutions
Gene Therapy and Precision Medicine
Gene therapy and precision medicine are changing how we treat rare heart diseases. By focusing on the genetic causes, researchers are creating treatments that can stop or reverse disease. For instance, CRISPR/Cas9 gene editing is being looked at for treating genetic heart conditions.
The advantages of gene therapy and precision medicine include:
- Personalized treatment approaches tailored to individual genetic profiles
- Potential for more effective treatment with fewer side effects
- Opportunities for preventive interventions in at-risk individuals
As research keeps moving forward, we’ll see even more innovative treatments for rare heart diseases. This will greatly improve the lives of patients all over the world.
Diagnostic Challenges in Rare Cardiac Conditions
Doctors find it hard to diagnose the rarest heart problems. Finding rare heart abnormalities needs a detailed plan. This plan includes using the latest tools and methods.
Advanced Imaging Techniques
Advanced imaging is key in spotting uncommon cardiac abnormalities. Tools like cardiac MRI and CT scans give clear views of the heart. This helps doctors find rare issues.
These methods help check the heart’s shape, how it works, and its tissues. This is vital for spotting problems like arrhythmogenic right ventricular cardiomyopathy (ARVC) and other rare heart issues.
Genetic Testing and Counseling
Genetic testing is now a must for diagnosing rarest cardiac disorders. It helps find specific genetic changes. This way, doctors can spot conditions like hypertrophic cardiomyopathy and long QT syndrome.
Genetic counseling is also very important. It helps patients and their families understand what genetic tests mean. It also shows the risk of passing these conditions to future generations.
Emerging Biomarkers and Molecular Diagnostics
The field of rare heart conditions is growing thanks to new biomarkers and molecular diagnostics. Biomarkers like troponin and natriuretic peptides show heart damage or stress. Molecular diagnostics find genes that cause diseases.
These new tools make diagnosis more accurate and help start treatment sooner. This is key for better results in patients with rare heart problems.
Living with Rare Heart Conditions: Patient Perspectives
Living with a rare heart condition is complex. It involves medical, emotional, and social aspects. Patients and their families face unique challenges that need support and understanding.
Psychosocial Impact and Quality of Life
Having a rare heart condition deeply affects a person’s mental health and life quality. The condition’s rarity and uncertainty can cause feelings of isolation and frustration. As one patient shared,
“It’s like being in a storm with no clear direction or shelter.”
This shows the importance of strong support systems.
The psychosocial impact isn’t just on the patient. It affects their family and caregivers too. The emotional weight is heavy, requiring counseling and psychological support. By helping with these needs, we can better the lives of those with rare heart conditions.
Support Resources and Patient Advocacy
There are many support resources for those with rare heart conditions. These include advocacy groups, online forums, and specialized healthcare. For example, groups focused on rare heart conditions offer information, emotional support, and a sense of community. As a patient advocate said,
“Support groups have been a lifeline for many of our members, providing a space to share and find solidarity.”
Patient advocacy is key in raising awareness about rare heart diseases. By listening to patients and promoting education, we can improve care and treatment. Advocacy groups are vital in this effort, ensuring the needs of those with rare heart conditions are met.
In summary, caring for someone with a rare heart condition needs a holistic approach. This includes medical care, psychosocial support, and advocacy. By providing all-around resources and awareness, we can improve the lives of patients and their families.
Global Disparities in Rare Heart Disease Care
The world faces big challenges in treating rare heart diseases. Not everyone can get the care they need. This makes life harder for those with rare cardiovascular conditions.
Access to Diagnosis and Specialized Care
Getting a quick and right diagnosis is hard for uncommon cardiovascular diseases. In many places, there’s a lack of advanced tools and experts. This means patients often get late or wrong care.
Dealing with rarest cardiovascular conditions needs a team of doctors. But, not all places have these teams. Many patients struggle to find the right care.
Orphan Drug Availability and Cost Challenges
Orphan drugs are special medicines for rare diseases. But, they’re hard to find and expensive. This makes it tough for patients to get the treatment they need.
The high cost of these drugs is a big problem. It affects how patients get care and strains healthcare budgets. We need to make these drugs more available and affordable.
We must strive for a fair healthcare system. Patients with rare heart diseases should get the care they need, no matter where they are.
Conclusion
Improving care for rare heart disorders needs a team effort. This includes more research, better diagnostic tools, and full support. We’ve looked at many uncommon heart conditions and the rarest heart diseases. We’ve seen how unique they are and the big challenges they bring. Knowing how complex these conditions are helps us see the need for special care. It also shows how important ongoing research is. Better diagnostic tools and treatments are key to improving life for those with these conditions. We must keep supporting patients with rare heart disorders. We need to work together to promote research, education, and care. This way, we can make sure patients with uncommon heart conditions get the care they need.
FAQ
What are rare heart conditions?
Rare heart conditions are diseases that affect the heart but are not common. They often need special care and management.
What is Uhl’s anomaly?
Uhl’s anomaly is a very rare heart condition. It affects the right ventricle in a unique way. This makes diagnosis and management very challenging.
What is Barth syndrome?
Barth syndrome is a rare heart disease that mainly affects males. It has a genetic cause and specific symptoms.
What is Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC)?
ARVC is a rare heart condition that affects the right ventricle. It causes arrhythmias and can be dangerous. It has a genetic cause and specific ways to diagnose it.
What is restrictive cardiomyopathy?
Restrictive cardiomyopathy is a rare heart disease. It affects the ventricles and has a specific cause. There are different types and ways to diagnose it.
What is Eisenmenger syndrome?
Eisenmenger syndrome is a complex heart defect. It arises from uncorrected defects and causes high blood pressure in the lungs. It needs modern treatment strategies.
What is cardiac amyloidosis?
Cardiac amyloidosis is a rare disease that affects the heart. It causes the heart to work poorly. There are different types and new treatments are being developed.
How is Hypoplastic Left Heart Syndrome (HLHS) managed?
HLHS is a complex heart defect. It requires surgery in stages. The surgery involves specific steps and techniques.
What is Brugada syndrome?
Brugada syndrome is a rare heart disorder. It can cause dangerous arrhythmias. It has a genetic cause and specific ways to diagnose and manage it.
What is Ebstein’s anomaly?
Ebstein’s anomaly is a rare heart defect. It affects the tricuspid valve. It requires careful management and specific surgery.
How are pediatric rare heart conditions managed?
Pediatric rare heart conditions are challenging. They require special care from birth to adulthood. There are specific strategies for managing them.
What are the current research advances in rare cardiovascular diseases?
Research is making progress in rare heart diseases. There are clinical trials, registries, and new treatments like gene therapy and precision medicine.
What are the diagnostic challenges in rare cardiac conditions?
Diagnosing rare heart conditions is complex. It involves advanced imaging, genetic testing, and counseling. New biomarkers and diagnostics are emerging.
How do rare heart conditions affect quality of life?
Rare heart conditions can greatly impact quality of life. They affect mental health and daily life. Support and advocacy are important.
What are the global disparities in rare heart disease care?
Access to care for rare heart diseases varies worldwide. There are differences in diagnosis, treatment, and access to drugs. Solutions are needed.
What is the importance of patient advocacy for rare heart conditions?
Patient advocacy is key for those with rare heart conditions. It provides support, raises awareness, and ensures access to care.
What are uncommon cardiac diseases?
Uncommon cardiac diseases are rare heart conditions. They require specialized knowledge and care.
What are the rarest cardiovascular diseases?
The rarest cardiovascular diseases include Uhl’s anomaly, Barth syndrome, and others. They need specific management and care.
Reference
World Health Organization. Evidence-Based Medical Insight. Retrieved from https://www.who.int/news-room/fact-sheets/detail/rare-diseases




































