Urethral dilation is a common treatment for a urethral stricture. But the pain level varies a lot among patients. The thought of this procedure can be scary, mainly because of the pain and worry.
Research shows that self-dilation has a median pain score of 3 out of 10. Yet, many men with strictures say they feel pain before treatment. Mostly Clinic says pain can be controlled with over-the-counter pain meds. Sometimes, doctors might give stronger pain meds.
Key Takeaways
- Urethral dilation pain varies among patients.
- Pain can be managed with medication.
- Some discomfort is common during and after the procedure.
- Healthcare providers may prescribe pain relief for severe pain.
- Pain typically improves after several days.
What You Need to Know About Urethral Strictures
We will explore the complexities of urethral strictures. This includes their causes, symptoms, and treatment options. A urethral stricture is when the urethra narrows, causing obstructive urinary symptoms. Knowing about this condition is key to effective management and treatment.
Common causes of urethral narrowing
Urethral strictures can come from injuries, infections, or inflammatory conditions. Trauma to the urethra, from accidents or medical procedures, is a common cause. Infections, like sexually transmitted ones, can also lead to strictures. Conditions like lichen sclerosus can cause narrowing too.
| Cause | Description |
| Trauma | Injury to the urethra from accidents or medical procedures |
| Infections | Sexually transmitted infections or other urethral infections |
| Inflammatory Conditions | Conditions like lichen sclerosus that cause urethral inflammation |
Symptoms that indicate a urethral stricture
The symptoms of urethral stricture vary but often include weak urine flow and straining to urinate. Some may feel like their bladder isn’t emptying fully. UTIs or pain while urinating can also occur. Recognizing these symptoms early is key to timely treatment.
Common symptoms include:
- Weak or interrupted urine flow
- Straining to urinate
- Frequent UTIs
- Pain or discomfort while urinating
How strictures are diagnosed
Diagnosing urethral strictures involves several tests. These include uroflowmetry to check urine flow rate, cystoscopy to see inside the urethra, and retrograde urethrography to image the urethra. These tests help doctors understand the stricture’s location, length, and severity. This information guides the treatment choice.
Understanding the diagnosis and the extent of the stricture is vital for choosing the right treatment. This can include urethral dilation, urethrotomy, or other interventions. We will discuss these treatment options in detail in the following sections.
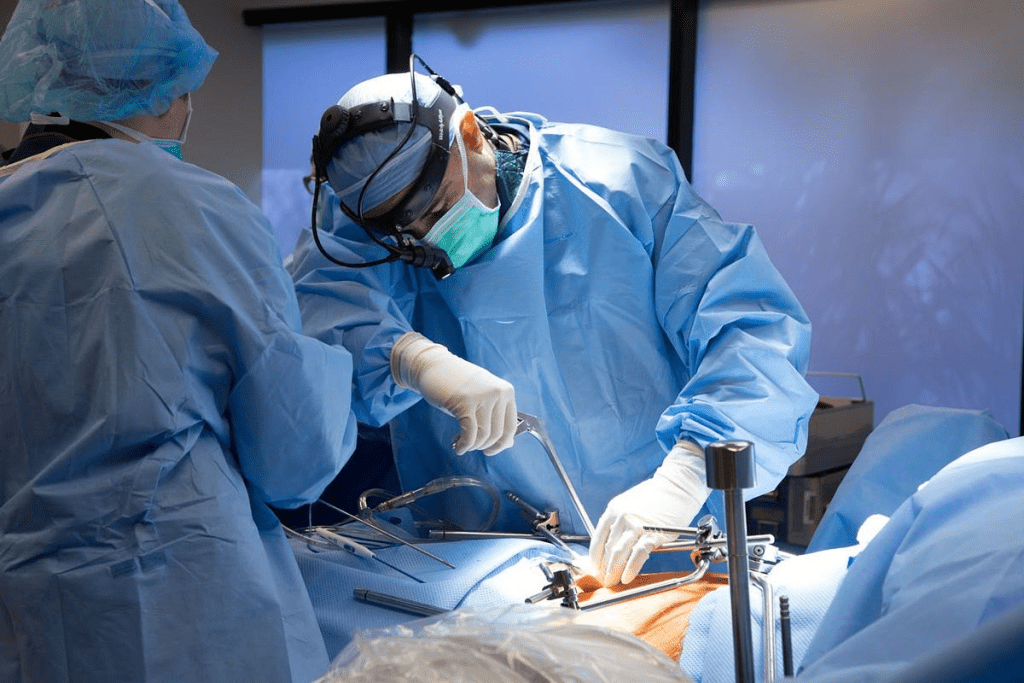
Understanding Urethral Dilation Procedures
Urethral dilation is key in treating urethral narrowing. It aims to widen the urethra for better urine flow. We’ll look at the methods and techniques used, ensuring patients get the right care.
Clinical Dilation Techniques
Healthcare professionals use clinical dilation techniques in a medical setting. These include balloon dilation and catheter-based dilation. Balloon dilation uses a balloon to stretch the urethra. Catheter-based dilation uses larger catheters to widen it.
Both methods are effective, chosen based on the patient’s condition and stricture severity.
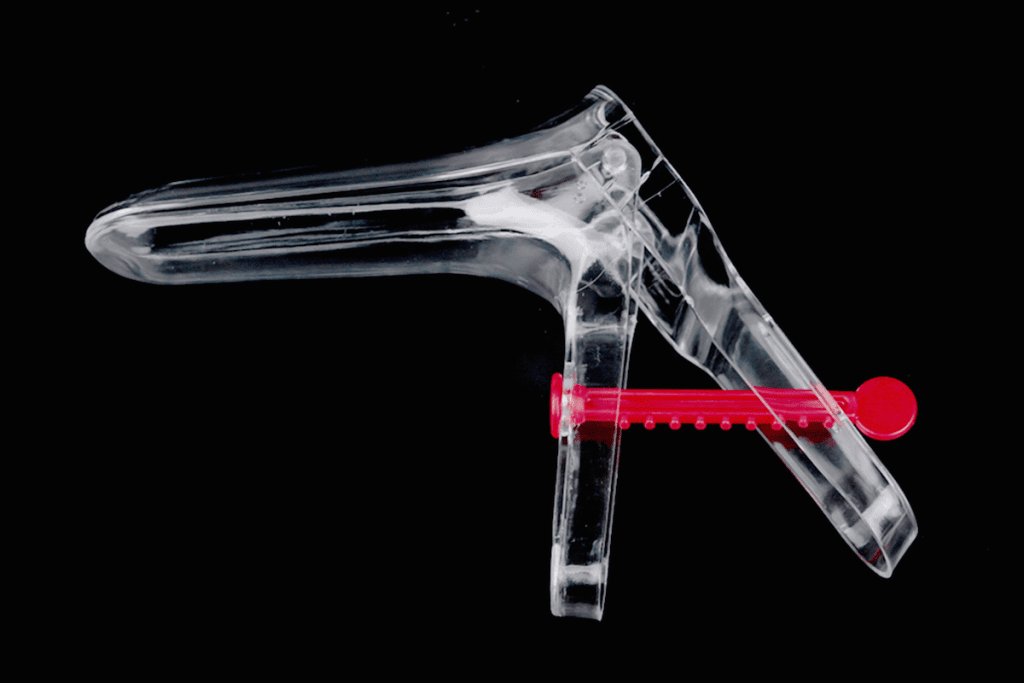
Self-Dilation Methods and Tools
Self-dilation lets patients manage urethral strictures at home. It uses ureteral dilators or tools to widen the urethra. Healthcare professionals teach patients how to do it safely.
The goal is to keep the urethra open and prevent strictures from coming back.
The tools for self-dilation are designed to be easy and comfortable. Regular use can greatly improve life for those with urethral strictures.
Alternatives to Urethral Dilation
Urethral dilation is common, but there are other treatments. These include surgical reconstruction and endoscopic treatments. Surgical reconstruction repairs or replaces the urethra. Endoscopic treatments are minimally invasive.
The choice depends on the stricture’s severity, location, and the patient’s health. Knowing these options helps patients make informed decisions.
We work with patients to find the best treatment plan for them.
Pain Levels During Urethral Dilation
It’s important to know about the pain levels when getting urethral dilation. This treatment helps with urethral strictures, which can cause pain and trouble with urination. We’ll look at the pain levels, using stats and patient stories to help understand it better.
Reported Pain Scores
Research shows that people who undergo urethral dilation experience different levels of pain. For example, self-dilation has a median pain score of 3 out of 10. This means some discomfort is normal, but it’s usually not too bad for most people.
A study found that 71% of men with urethral strictures felt pain before treatment. This shows how strictures can really affect a person’s life, making treatments like dilation very important.
Patient Testimonials and Experiences
What patients say about urethral dilation is very helpful. For instance, one patient said, “The procedure was uncomfortable, but the pain was temporary and manageable.” These stories show how different people can feel and why care should be tailored to each person.
“I was nervous about the procedure, but the healthcare team was very supportive and helped me through it.” -A patient undergoing urethral dilation
Pre-existing Pain from Strictures
Pain from urethral strictures before dilation can affect how a patient feels during the procedure. Those with more severe strictures might feel more pain.
Knowing what causes pain during dilation is key to managing it better. By tackling these issues, doctors can make treatments better and more comfortable for patients.
5 Factors That Influence Pain During Dilation
Understanding what causes pain during urethral dilation is key to managing it. This procedure, often needed for urethral strictures, can be painful for different people. We’ll look at the main factors that lead to this pain, helping both patients and doctors handle it better.
Patient Age and Its Impact on Discomfort
Studies show that younger patients often feel more pain during urethral dilation. This is due to both physical and mental reasons. Younger people might feel pain differently and worry more, making their experience worse.
“The younger the patient, the more likely they are to experience significant discomfort during urethral dilation,” notes a study on urethral stricture treatments. This shows the need for pain management plans that consider the patient’s age.
Technique and Skill of the Practitioner
The skill of the person doing the dilation greatly affects how much pain you feel. A skilled practitioner uses the right urethral dilator and technique, making the process less painful.
Experienced doctors know how to move gently and precisely. This reduces the chance of hurting the urethra and lowers pain. “A gentle touch and thorough understanding of urethral anatomy are key to less pain during dilation,” says a leading urologist.
Type and Size of Dilators Used
The type and size of urethral dilators used can also change how much pain you feel. Different materials and sizes can affect comfort levels, with some being better for certain patients.
- The material of the dilator (e.g., metal, plastic, or inflatable)
- The size of the dilator, which should be chosen based on the stricture’s severity
- The gradualness of dilation, which can affect patient comfort
Choosing the right dilator is a big decision for healthcare providers. It helps ensure the procedure is comfortable and successful.
Patient Anxiety and Psychological Factors
Anxiety and mental factors greatly affect how much pain you feel during dilation. People who are more anxious might feel more pain, making it hard for both the patient and the doctor.
“Addressing patient anxiety through counseling or relaxation techniques can significantly reduce the pain experienced during urethral dilation procedures,” according to a clinical psychologist specializing in medical procedures.
Helping manage anxiety is a big part of caring for patients going through urethrotomy or dilation. It’s important for their overall care.
Conclusion
It’s important for patients to know about the pain that can happen during urethral dilation. We’ve looked at the different parts of urethral dilation. This includes the procedures, the pain patients feel, and what makes the pain worse.
Urethral dilation is a common and effective way to treat a urethral stricture. Knowing about the treatment can make a big difference for patients. By understanding the causes of narrowing, symptoms, and dilation techniques, patients can handle their treatment better.
Talking to healthcare providers about concerns is key to a good urethral dilation experience. By doing this, patients can safely and effectively dilate their urethra. This helps to reduce symptoms of urethral stricture and improve their life quality.
FAQ
What is urethral dilation, and why is it performed?
Urethral dilation is a medical procedure to treat a urethral stricture. This condition narrows the urethra, causing urine flow problems. We perform it to widen the urethra, improving urine flow and reducing symptoms like weak urine flow and painful urination.
Is urethral dilation a painful procedure?
Pain levels vary during urethral dilation. We use local anesthesia to reduce discomfort. Some may feel mild pain after, which can be managed with medication.
What are the risks and complications associated with urethral dilation?
Urethral dilation may have risks like bleeding, infection, and urethral trauma. Stricture can also come back, needing more treatments. We take steps to minimize these risks and ensure a safe procedure.
How is a urethral stricture diagnosed?
We use tests like uroflowmetry, cystoscopy, and retrograde urethrography to diagnose urethral stricture. These tests help us understand the stricture’s severity and location, guiding our treatment.
What are the alternatives to urethral dilation?
Alternatives include urethrotomy, a surgical procedure, or more invasive surgical reconstruction. We choose the best option based on the stricture’s severity and the patient’s medical history.
Can I perform self-dilation at home?
Yes, self-dilation can be recommended as a maintenance treatment. We guide on proper technique and equipment use for safe and effective self-dilation.
How can I manage pain and discomfort after urethral dilation?
We provide pain relief medication and guidance on managing discomfort. Additional measures like applying heat or cold packs may also be recommended.
Will I need to undergo repeated urethral dilations?
The need for repeated dilations depends on the stricture’s cause and initial treatment success. We monitor progress and adjust treatment plans to prevent recurrence.
References
- American Urological Association. (2016). Urethral Stricture: AUA Guideline. Retrieved fromhttps://www.auanet.org/guidelines-and-quality/guidelines/urethral-stricture-guideline


































