Last Updated on November 26, 2025 by Bilal Hasdemir
Nearly 20% of women diagnosed with ovarian cancer are over 65. This shows the need for effective treatments for all ages. We look into if removing the ovary can cure ovarian cancer treatment.
Ovarian cancer is a complex condition needing a detailed treatment plan. Understanding the available options is key for patients and their families. We will talk about the role of surgery in treating this condition.
Exploring ovarian cancer treatment, it’s important to know the benefits and limits of surgery. This includes removing the ovary.
Key Takeaways
- Ovarian cancer treatment often involves a combination of therapies.
- Surgery plays a critical role in treating ovarian cancer.
- The decision to remove the ovary depends on various factors, including the stage of cancer.
- Understanding the treatment options is vital for making informed decisions.
- Patients should discuss their individual circumstances with their healthcare provider.
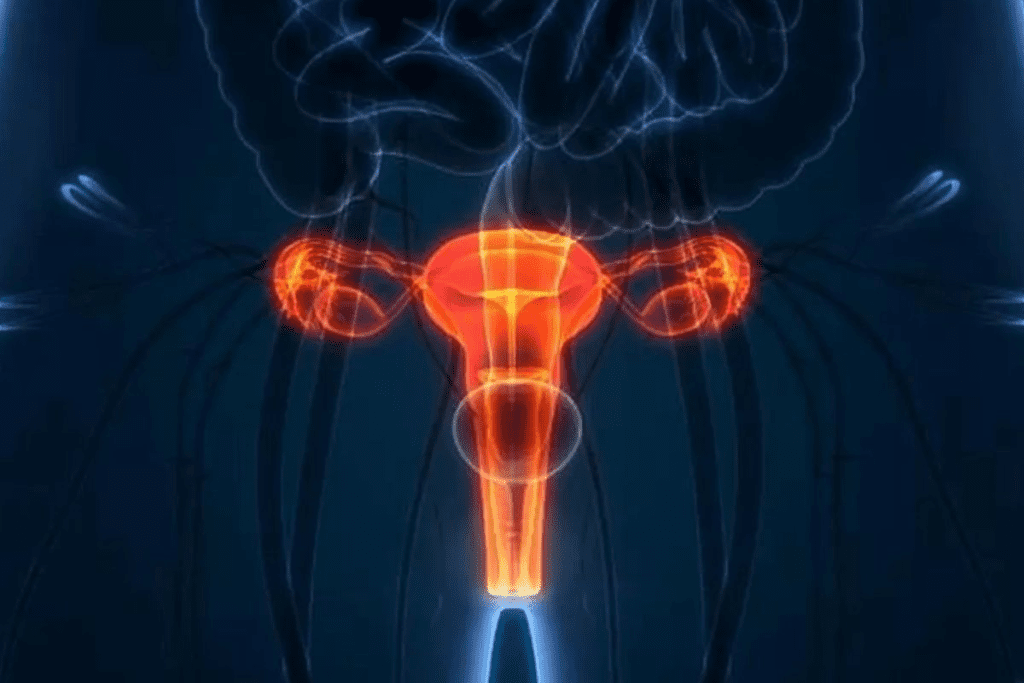
Understanding Ovarian Cancer: Types, Stages, and Risk Factors
Learning about ovarian cancer starts with knowing its types, stages, and risk factors. It’s a disease that affects women all over the world. Understanding it well is key to managing and treating it effectively.
Common Types of Ovarian Cancer
Ovarian cancer is not just one disease; it’s several types. Each type comes from different cells in the ovary. The most common types are:
- Epithelial tumors: These make up about 90% of ovarian cancers. They start in the outer layer of the ovary.
- Germ cell tumors: These are less common. They affect younger women and start in the egg-producing cells.
- Stromal tumors: These are rare. They start in the ovary’s connective tissue.
Knowing the type of ovarian cancer is important for choosing the right treatment.
Staging System Explained
The stage of ovarian cancer is very important. It helps doctors know how to treat it and what to expect. The FIGO system is the most used. It divides ovarian cancer into four stages:
- Stage I: Cancer is only in one or both ovaries.
- Stage II: Cancer has spread to other parts of the pelvis.
- Stage III: Cancer has spread to nearby parts of the abdomen or lymph nodes.
- Stage IV: Cancer has spread to distant places like the liver or lungs.
Key Risk Factors and Warning Signs
There are several risk factors for ovarian cancer. These include genetic mutations, family history, age, and reproductive history. It’s also important to know the warning signs. Common symptoms include:
- Pelvic or abdominal pain
- Bloating or swelling in the abdomen
- Difficulty eating or feeling full quickly
- Urinary urgency or frequency
While these symptoms can be vague, seeing a doctor if they’re persistent or severe is important.
By knowing about ovarian cancer types, stages, and risk factors, women can take better care of their health. This knowledge helps them make informed choices about their well-being.
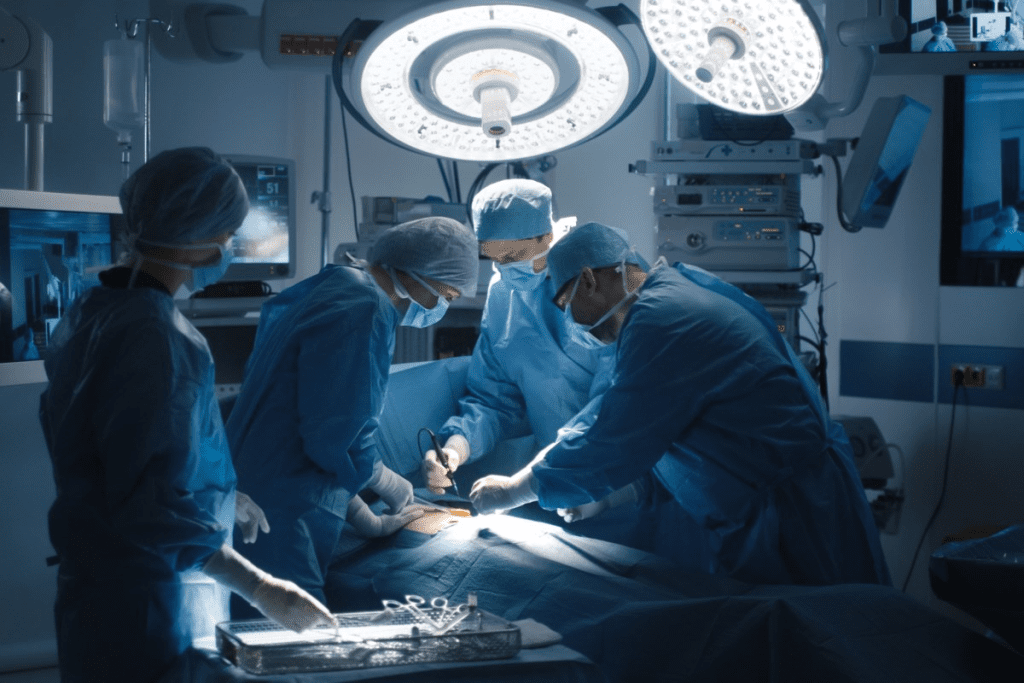
The Role of Surgery in Ovarian Cancer Treatment
Surgery is a key part of treating ovarian cancer. It depends on the patient’s condition and cancer stage. Surgery helps in diagnosing, removing tumors, or as part of a treatment plan.
Surgery as a Primary Treatment Approach
Surgery is often the first step in treating ovarian cancer, mainly in early stages. The goal is to remove as much tumor as possible. This makes other treatments like chemotherapy more effective. Oophorectomy, or the removal of one or both ovaries, is a common surgical procedure for ovarian cancer.
The type and extent of surgery depend on several factors. These include the cancer stage, the patient’s health, and if they want to keep their fertility. The decision-making process involves a careful evaluation of these factors to determine the most appropriate surgical approach.
Diagnostic vs. Therapeutic Surgical Procedures
Surgical procedures for ovarian cancer can be either diagnostic or therapeutic. Diagnostic surgery takes a sample of tissue or fluid for examination. Therapeutic surgery aims to remove the cancerous tissue or tumor.
“Surgery is a critical component of ovarian cancer treatment, often leading to cure, when diagnosed early.”
An Oncologist
Therapeutic surgeries can range from removing the affected ovary to more extensive surgeries. This depends on the disease extent.
When Surgery Is Recommended
Surgery is recommended for early-stage ovarian cancer or advanced cancer to alleviate symptoms. The decision to have surgery is made based on the patient’s health and preferences.
| Surgical Procedure | Description | Indications |
| Unilateral Oophorectomy | Removal of one ovary | Early-stage cancer, desire to preserve fertility |
| Bilateral Oophorectomy | Removal of both ovaries | Advanced cancer or post-menopause |
| Total Hysterectomy with Bilateral Salpingo-Oophorectomy | Removal of uterus, ovaries, and fallopian tubes | Advanced cancer, completion of childbearing |
In conclusion, surgery is vital in treating ovarian cancer. It offers various options tailored to each patient’s needs. Understanding the different surgical approaches helps patients make informed decisions about their care.
Ovary Removal Ovarian Cancer Cure: Examining the Evidence
Patients with ovarian cancer often wonder if removing the ovary can cure the disease. The answer depends on the cancer’s stage, type, and the patient’s overall health.
We’ll look at how effective ovary removal is in treating ovarian cancer. We’ll focus on success rates by cancer stage, the limits of oophorectomy alone, and research on its cure.
Success Rates by Cancer Stage
The success of ovary removal in curing ovarian cancer depends on the cancer’s stage. Early-stage ovarian cancer has a better prognosis than advanced stages.
- Stage I: Cancer is limited to one or both ovaries. Surgery alone can cure many cases, if caught early.
- Stage II and beyond: Cancer has spread beyond the ovaries. Surgery is key, but chemotherapy is often needed too.
Limitations of Oophorectomy Alone
Oophorectomy (ovary removal) is a key surgery for ovarian cancer. But, it’s not enough to cure the disease, mainly if the cancer has spread.
Research shows that removing the ovary can be very effective if the cancer is only in the ovary. But, for more advanced cases, a mix of treatments is needed.
Research Findings on Curative Potentials
Studies have looked into how well oophorectomy works in treating ovarian cancer. For example, research on toxins like PFOS has shown risks for ovarian cancer and its treatment.
Our understanding of ovarian cancer and its treatment is growing. Oophorectomy is a key part of this research, showing its value when used with other treatments.
By looking at the evidence, we can see when ovary removal is likely to cure the disease. We also know when more treatments are needed.
Types of Surgical Procedures for Ovarian Cancer
Surgery is key in treating ovarian cancer. Different procedures are used based on the cancer’s stage and the patient’s health. The right surgery depends on the disease’s extent and if the patient wants to keep their fertility.
Unilateral Oophorectomy
A unilateral oophorectomy removes one ovary. It’s an option for women with early-stage ovarian cancer who want to keep their fertility. This is often chosen by younger patients who haven’t finished having children. The goal is to remove the cancerous ovary while leaving the other reproductive organs intact, keeping hormonal balance and pregnancy possibilities.
Bilateral Oophorectomy
In a bilateral oophorectomy, both ovaries are removed. This is more common, often for advanced cancer or high risk in both ovaries. Removing both ovaries stops estrogen production, which can help some ovarian cancers grow. But, it causes immediate menopause, affecting the patient physically and emotionally.
Total Hysterectomy with Bilateral Salpingo-Oophorectomy
This surgery removes the uterus, both ovaries, and both fallopian tubes. It’s for women who are postmenopausal or have finished having children. This approach removes all cancer sources, lowering recurrence risk. But, it’s a more invasive surgery with a longer recovery.
Debulking Surgery
Debulking surgery aims to remove as much tumor as possible. It’s used for advanced ovarian cancer that has spread.
“The goal of debulking surgery is to leave behind only minimal residual disease, as this has been shown to improve survival outcomes and quality of life for patients.”
Though not always curative, debulking surgery makes other treatments like chemotherapy more effective.
Is Removing One Ovary Enough for Ovarian Cancer?
Ovarian cancer surgery might remove one ovary. But is this enough to get rid of the cancer? We’ll look at what decides this choice and what it means for patients.
Factors That Determine Surgical Approach
Choosing to remove one or both ovaries depends on several things. These include the cancer’s stage and type, the patient’s health, and if they want to keep their fertility.
Key considerations include:
- The extent of cancer spread
- The patient’s age and reproductive plans
- The presence of genetic mutations that may increase cancer risk
Risks of Cancer in the Remaining Ovary
Removing just one ovary means there’s a chance cancer could grow in the other. We’ll talk about how likely this is and how to watch for it.
This risk is higher for those with a family history of ovarian cancer or certain genetic mutations like BRCA1 and BRCA2.
Fertility Considerations
Many women with ovarian cancer worry about keeping their fertility. We’ll look at how removing one ovary might affect this.
Fertility options after oophorectomy may include:
- Embryo or egg freezing
- Ovarian tissue preservation
- Consideration of alternative treatments that may preserve ovarian function
We know every patient is different. We’re dedicated to caring for both the cancer and the patient’s quality of life.
Stage 1 Ovarian Cancer: Can Surgery Alone Be Curative?
Women with early-stage ovarian cancer often wonder if surgery can cure them. The journey through diagnosis and treatment is tough. It’s important to know if surgery can treat stage 1 ovarian cancer effectively.
Success Rates for Early-Stage Cancer
Surgery for stage 1 ovarian cancer looks promising. Early diagnosis is key. If the cancer is well-differentiated and only in the ovary, surgery can often cure it.
Recent studies show that women with stage 1 ovarian cancer who had surgery have a high five-year survival rate. This rate is often over 90%. It shows surgery can be a strong treatment for early-stage ovarian cancer.
When Additional Treatments May Be Needed
While surgery can cure many, some cases need more treatment. The cancer’s type, grade, and if it has spread are important. These factors decide if more treatment is needed.
If the cancer is high-grade or at high risk of coming back, chemotherapy may be suggested. We help patients choose the best treatment for them.
Monitoring After Surgery
Monitoring after surgery is vital for ovarian cancer treatment. Regular check-ups help us see how the patient is doing. They also help catch any signs of cancer coming back early.
“Regular surveillance is key to managing ovarian cancer effectively, even after successful surgery,” says a leading oncologist. “Through a combination of physical exams, imaging tests, and tumor marker assessments, we can monitor for any changes that may indicate a recurrence.”
Following the recommended follow-up schedule is very important. It helps ensure the best results for our patients.
Advanced Ovarian Cancer: The Role of Debulking Surgery
Debulking surgery plays a key role in treating advanced ovarian cancer. It involves removing as much of the tumor as possible. This surgery is also known as cytoreductive surgery.
Goals of Cytoreductive Surgery
The main goal of cytoreductive surgery is to leave no tumor larger than 1 cm. This is important because it affects how well treatments like chemotherapy work.
The surgery aims to:
- Remove as much tumor as possible to reduce the tumor burden.
- Relieve symptoms like pain or bowel obstruction caused by the tumor.
- Improve the patient’s quality of life by reducing the need for other treatments.
Optimal vs. Suboptimal Debulking
Debulking surgery success is measured as either optimal or suboptimal. Optimal debulking means leaving behind tumors less than 1 cm. Suboptimal debulking means larger tumors are left.
Patients who achieve optimal debulking tend to have better survival rates and quality of life. This is compared to those with suboptimal debulking.
“The extent of surgical cytoreduction is a significant predictor of survival in patients with advanced ovarian cancer.”
Impact on Survival and Quality of Life
Debulking surgery greatly impacts survival and quality of life for patients with advanced ovarian cancer. It reduces the tumor burden, making treatments more effective.
Research shows that successful debulking surgery leads to:
- Improved overall survival rates.
- Enhanced quality of life due to reduced symptoms.
- Better response to chemotherapy.
Every patient’s situation is different. Deciding on debulking surgery should be done with a healthcare provider. Understanding the goals and benefits helps patients make informed decisions about their care.
Minimally Invasive Surgical Options for Ovarian Cancer
Ovarian cancer surgery is changing with new, less invasive methods. These advances offer patients fewer complications and quicker healing. We’ll look at the different minimally invasive surgeries for ovarian cancer and their benefits.
Laparoscopic Procedures
Laparoscopic surgery, or keyhole surgery, uses small cuts in the belly to insert tools. It’s used for both checking and treating ovarian cancer. This method can cut down on hospital time, scarring, and pain after surgery.
Some benefits of laparoscopic surgery are:
- Smaller cuts mean less scarring
- Less pain after surgery
- Shorter time in the hospital
- Quicker recovery
Robotic-Assisted Surgery
Robotic-assisted surgery uses a robotic system to help the surgeon. It offers clear 3D views, precise tools, and better control. This tech is great for complex surgeries, making them more precise.
The benefits of robotic-assisted surgery are:
- More precise and accurate
- Better views
- More control and flexibility
- Potential for fewer complications
Patient Selection Criteria
Not every patient with ovarian cancer can have minimally invasive surgery. The choice depends on the cancer stage, tumor size, and the patient’s health. We carefully pick the best surgery for each patient.
The table below shows what we consider when choosing minimally invasive surgery:
| Factor | Description | Consideration |
| Cancer Stage | Early-stage cancer may be more suitable for minimally invasive surgery | Advanced stages may require more extensive surgery |
| Tumor Size | Smaller tumors are generally more amenable to minimally invasive surgery | Large tumors may necessitate open surgery |
| Patient Health | Patients with significant comorbidities may benefit from minimally invasive surgery | Overall health status influences surgical risk |
By choosing the right patients and using the best minimally invasive techniques, we can improve outcomes. This helps women with ovarian cancer live better lives.
Recovery After Ovary Removal Surgery
Knowing what to expect after oophorectomy surgery can make recovery easier. We’ll help you understand the hospital stay, recovery time, and how to manage pain and physical limits.
Typical Hospital Stay and Recovery Timeline
The time you spend in the hospital after ovarian cancer surgery varies. It depends on the surgery’s complexity and your health. Usually, patients stay 2-4 days.
Recovery time can be weeks to months. It’s key to follow your doctor’s post-op instructions for a smooth recovery.
| Recovery Stage | Timeline | Key Activities |
| Immediate Recovery | 1-3 days | Rest, pain management, monitoring for complications |
| Early Recovery | 1-2 weeks | Gradual increase in activity, follow-up appointments |
| Late Recovery | 4-6 weeks | Return to normal activities, follow-up care |
Physical Limitations and Activity Restrictions
After oophorectomy, avoid heavy lifting, bending, and hard activities for weeks. This prevents complications and aids healing.
- Avoid lifting objects heavier than 10 pounds for 4-6 weeks.
- Limit bending and twisting motions.
- Gradually increase walking and other low-impact activities.
Managing Post-Surgical Pain
Managing pain well is key for a comfortable recovery. Follow your doctor’s advice on pain meds and other methods.
Pain Management Strategies:
- Use prescribed pain medications as directed.
- Apply heat or cold packs to the affected area (as advised by your doctor).
- Practice relaxation techniques, such as deep breathing or meditation.
Side Effects and Long-Term Implications of Ovary Removal
Ovary removal surgery, also known as oophorectomy, can lead to various side effects. This surgery is sometimes needed for treating ovarian cancer or other conditions. It’s important to know its long-term effects.
Hormonal Changes and Surgical Menopause
One major effect of ovary removal is a sudden drop in hormone levels, causing surgical menopause. This condition can lead to symptoms like:
- Hot flashes
- Night sweats
- Mood swings
- Vaginal dryness
These symptoms can be more intense than those in natural menopause. This is because the hormonal change happens suddenly, not gradually.
Psychological and Emotional Impact
The hormonal changes after ovary removal can also affect a woman’s psychological and emotional state. Some women may feel:
- Depression
- Anxiety
- Mood disorders
Healthcare providers should offer support. They might also refer patients to mental health professionals if needed.
Hormone Replacement Therapy Considerations
To help with symptoms, hormone replacement therapy (HRT) might be suggested. HRT can manage:
- Menopausal symptoms
- Osteoporosis risk
- Cardiovascular health
But, starting HRT should be a careful decision. It’s best to talk to a healthcare provider about its risks and benefits.
Choosing to have ovary removal surgery is a big decision. Knowing the possible side effects and long-term effects helps women make better health choices.
Survival Rates and Prognosis After Ovarian Cancer Surgery
Survival rates for ovarian cancer depend on the stage and surgery success. Knowing these stats helps patients and families make better care choices.
Five-Year Survival Statistics by Stage
The five-year survival rate is a key indicator for ovarian cancer patients. The overall rate is about 48%. But, it changes a lot based on the stage.
- Stage I has a 90% five-year survival rate.
- Stage II drops to around 70%.
- Stage III has a 39% rate.
- Stage IV’s rate is about 17%.
These numbers show how important early detection and good treatment are.
Factors That Influence Prognosis
Many things affect ovarian cancer prognosis after surgery. These include:
- The tumor’s stage and grade.
- How well the surgery removes cancer.
- The patient’s health and age.
- Genetic mutations like BRCA1 and BRCA2.
Knowing these can help tailor treatments for better results.
Quality of Life Considerations
Quality of life after treatment is key. Surgery can cure cancer but also has long-term effects. We support patients through these challenges.
Our teams help manage symptoms and address fertility and sexuality concerns. We also guide on hormone therapy when needed. This approach improves life quality for survivors.
Understanding survival rates, prognostic factors, and treatment effects helps patients navigate their journey.
Complementary Treatments: When Surgery Isn’t Enough
There are many treatments beyond surgery for ovarian cancer. Surgery is a key part of treatment, but more is often needed. These extra treatments help ensure the best care.
Chemotherapy After Surgery
Chemotherapy is a common treatment after surgery. It helps get rid of any cancer cells left behind. This treatment lowers the chance of cancer coming back.
The type and length of chemotherapy depend on the cancer’s stage and type. Chemotherapy regimens use drugs given through an IV or by mouth. Common drugs include carboplatin and paclitaxel.
Radiation Therapy Options
Radiation therapy is another treatment for ovarian cancer. It uses high-energy rays to kill cancer cells. We might suggest it for advanced cancer or when cancer has spread.
- External beam radiation therapy (EBRT) is the most common type, delivering radiation from outside the body.
- Internal radiation therapy, also known as brachytherapy, involves placing radioactive material inside the body.
Targeted Therapies and Immunotherapy
Targeted therapies and immunotherapy are new ways to fight ovarian cancer. Targeted therapies aim at specific molecules that help cancer grow. They help stop cancer cells from growing and spreading while protecting healthy cells.
Immunotherapy boosts the body’s immune system to fight cancer better. We’re looking into different immunotherapy methods, like checkpoint inhibitors and cancer vaccines, to improve treatment results.
By adding these treatments to surgery, we create a detailed treatment plan for each patient. This approach aims to improve outcomes and quality of life.
Making Treatment Decisions: Working With Your Healthcare Team
Dealing with ovarian cancer treatment needs teamwork between patients and their healthcare team. This partnership is key for making choices that fit the patient’s needs and wishes.
Questions to Ask Your Oncologist
Talking to your oncologist about treatment options is important. Understanding your diagnosis, treatment goals, and possible outcomes helps you make smart choices. Here are some questions to ask:
- What stage is my ovarian cancer, and what does it mean for treatment?
- What treatments are best for my case?
- What are the good and bad sides of each treatment?
- How will treatment change my quality of life?
Seeking Second Opinions
Getting a second opinion is a common and wise move in cancer treatment. It can give you more information and confidence in your treatment plan. Look for a specialist with ovarian cancer experience for your second opinion.
Balancing Quality of Life and Treatment Goals
Treatment for ovarian cancer aims to control the disease while keeping quality of life good. Patients and their healthcare team must work together to balance treatment benefits and side effects. This balance is key for effective and lasting treatment.
By working closely with your healthcare team and asking the right questions, you can make choices that support your well-being and treatment goals.
Conclusion: The Future of Ovarian Cancer Treatment
Looking ahead, ovarian cancer treatment is on the rise. Ongoing research and new care methods are bringing hope for better patient results. Studies have made big strides in understanding the disease, leading to more effective treatments.
Now, we’re moving towards treatments that are more tailored to each patient. This focus aims to boost survival rates and improve life quality. The future looks bright, with new trends and care advancements on the horizon.
Supporting research and innovation is key to better healthcare. We aim to deliver top-notch care with full support for patients. As ovarian cancer care keeps improving, we’re dedicated to providing the best care for those affected.
FAQ
Can removing the ovary cure ovarian cancer?
Removing the ovary is a key part of treating ovarian cancer. But, whether it cures the cancer depends on several things. These include the cancer’s stage and the patient’s overall health.
What is the role of surgery in ovarian cancer treatment?
Surgery is very important in treating ovarian cancer. It’s often the first step. Surgery helps remove the tumor and makes other treatments more effective.
Is removing one ovary enough for ovarian cancer treatment?
Taking out one ovary might be an option for early-stage cancer or for those wanting to keep their fertility. But, it depends on many factors. These include the cancer’s stage, the tumor’s characteristics, and the patient’s health.
What are the different types of surgical procedures for ovarian cancer?
There are several surgeries for ovarian cancer. These include removing one or both ovaries, and removing the uterus and ovaries. The choice depends on how far the cancer has spread and the patient’s needs.
Can stage1 ovarian cancer be cured with surgery alone?
Sometimes, surgery alone can treat stage1 ovarian cancer. But, other treatments like chemotherapy might also be needed. This depends on the tumor and other risk factors.
What is debulking surgery, and what is its role in advanced ovarian cancer?
Debulking surgery tries to remove as much tumor as possible. It’s used for advanced cancer to improve survival and quality of life. It reduces the tumor burden.
What are the benefits and challenges of minimally invasive surgical options for ovarian cancer?
Minimally invasive surgeries, like laparoscopic and robotic-assisted, offer less pain and quicker recovery. But, they might not be right for everyone. It depends on the patient’s condition and the cancer’s extent.
What can I expect during recovery after ovary removal surgery?
After ovary removal surgery, you’ll likely stay in the hospital. Then, you’ll need to rest and avoid strenuous activities. Managing pain is also important during recovery.
What are the side effects and long-term implications of removing the ovaries?
Removing the ovaries can cause hormonal changes and menopause. It can also affect your mood. Hormone replacement therapy might help manage these effects.
How do survival rates and prognosis vary after ovarian cancer surgery?
Survival rates after surgery for ovarian cancer vary a lot. They depend on the cancer’s stage and the patient’s overall health. Other treatments’ effectiveness also plays a role.
What complementary treatments are used when surgery isn’t enough?
When surgery isn’t enough, treatments like chemotherapy and radiation are used. Targeted therapies and immunotherapy are also options. These treatments work together with surgery to manage the disease.
How can I make informed treatment decisions for ovarian cancer?
To make informed decisions, work closely with your healthcare team. Ask questions and consider getting a second opinion. Think about how treatment will affect your quality of life.
What is the future of ovarian cancer treatment?
Ovarian cancer treatment is getting better with new research and advancements. These changes aim to improve outcomes and quality of life for patients.
Can ovary removal prevent ovarian cancer recurrence?
Ovary removal can lower the risk of cancer coming back. But, it depends on the cancer’s stage and how well the treatment works.
What are the risks associated with oophorectomy surgery?
Oophorectomy surgery has risks like infection and bleeding. It can also cause hormonal changes and lead to menopause.
References
- National Cancer Institute. (2023). Ovarian Epithelial, Fallopian Tube, and Primary Peritoneal Cancer Treatment (PDQ ®)“Health Professional Version. https://www.cancer.gov/types/ovarian/hp/ovarian-epithelial-treatment-pdq