Plastic surgery restores form and function through reconstructive procedures, cosmetic enhancements, and body contouring.
Send us all your questions or requests, and our expert team will assist you.
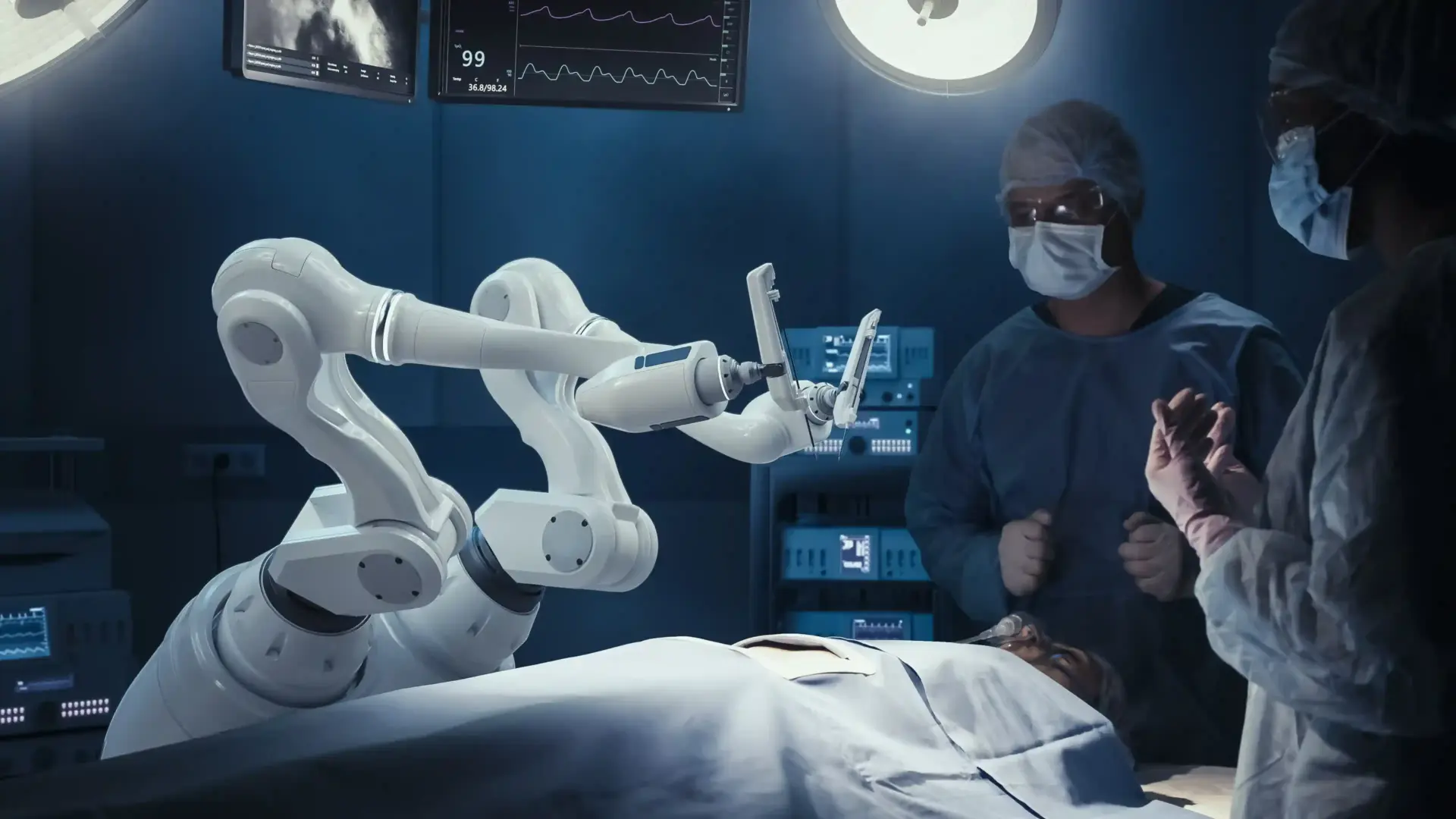
The Mommy Makeover is a complex, multi-procedural operation performed in a fully accredited surgical facility. The environment is optimized for safety, with hospital-grade monitoring equipment and strict sterility protocols. Because of the surgery’s length, maintaining the patient’s body temperature and fluid balance is critical.
The team includes the lead plastic surgeon, a board-certified anesthesiologist, and specialized surgical nurses. The workflow is meticulously choreographed to minimize the time the patient is under anesthesia. Often, two surgeons may work simultaneously to reduce operative time and enhance safety.

General anesthesia is the standard for Mommy Makeovers to ensure the patient is completely unconscious and the abdominal muscles are fully relaxed for repair. The anesthesiologist manages the airway and carefully titrates medications to ensure a smooth emergence.
Safety protocols include the use of antiemetics to prevent postoperative nausea and the administration of prophylactic antibiotics. Local anesthetic blocks (TAP blocks) are often injected into the abdominal wall to provide long-lasting pain relief for the first 24 hours.

The abdominal incision is placed low, typically within the bikini line, to ensure it can be hidden by underwear. The length depends on the amount of skin to be removed. The surgeon dissects down to the fascia, preserving the blood supply to the remaining skin flap.
The umbilicus is circumscribed and preserved on its stalk. After the muscles are tightened and the skin is pulled down, a new opening is made for the navel. The closure is done in multiple layers to reduce tension on the scar and ensure a fine healing line.
Breast incisions vary based on the procedure. For augmentation, the incision is usually in the inframammary fold. For a lift, incisions may be around the areola (donut), vertically down (lollipop), or in an inverted T (anchor) shape, depending on the degree of sagging.
The surgeon carefully designs these incisions to allow for maximum shaping while minimizing visible scarring. The breast tissue is reshaped internally, and the nipple is moved to a higher, more youthful position while preserving its blood and nerve supply.
Muscle repair is the core of abdominal restoration. The surgeon uses heavy, permanent, or long-lasting absorbable sutures to plicate the rectus fascia. This brings the muscles back to the midline and flattens the abdominal protrusion.
Modern techniques often involve a double-layer closure for added strength. This internal corset not only improves the cosmetic appearance but also restores the functional leverage of the abdominal wall.
Traditional abdominoplasty involved suction drains to remove fluid. Modern “drainless” techniques use progressive-tension sutures to tack the skin flap to the muscle, closing the dead space where fluid would otherwise collect.
Tissue glues or fibrin sealants may also be sprayed into the pocket. These biological adhesives help seal the tissues and reduce lymphatic leakage. This approach significantly increases patient comfort and simplifies postoperative care by eliminating the need to manage drains.
Send us all your questions or requests, and our expert team will assist you.

Liposuction is often the first step of the surgery, used to contour the waist and hips. Vaser (ultrasound-assisted) or laser-assisted systems are used to emulsify fat before removal. These technologies allow for smoother fat extraction and stimulate skin retraction.
Using these energy-based tools helps to define the musculature and create a more athletic look. It minimizes trauma to surrounding tissues, resulting in less bruising and a faster recovery than traditional mechanical liposuction.
The closure of all incisions is performed with microsurgical precision. The deep layers are closed first to relieve tension on the skin. This ensures that the blood supply to the skin edges is maintained and that the final scar will be thin and flat.
Surgeons often use barbed sutures that hold tension without knots, distributing the force evenly along the incision. The skin is then sealed with surgical glue or tape, providing a waterproof barrier that protects the wound during the initial healing phase.
Upon waking, the patient is moved to the recovery room. They are placed in a semi-reclined “beach chair” position to keep tension off the abdominal repair. Pain is managed through a multimodal approach involving oral and intravenous medications.
Nurses monitor the blood supply to the abdominal flap and the nipples. Early ambulation is encouraged to promote circulation. Patients are typically discharged once they are stable, alert, and their pain is well-controlled.
Advanced monitoring continues into the recovery. Some surgeons use smartphone apps to track patient progress, allowing patients to upload photos of their incisions for remote monitoring. This provides peace of mind and enables early detection of issues.
Non-invasive monitoring devices may be used to assess tissue oxygenation in the recovery room. These tools ensure that complex tissue rearrangements have not compromised the vascular supply to critical areas, such as the tummy tuck flap or the nipple.
Drainless techniques improve patient comfort by removing the need to manage awkward bulbs and tubes. They also reduce the risk of bacteria entering the wound through the drain site and make showering and dressing easier, often leading to a quicker return to normal activities.
The muscle repair component does cause significant soreness, often described as the feeling after an extreme abdominal workout. However, the use of long-acting local anesthetics (such as Exparel) and muscle relaxants has made recovery much more manageable than in the past.
A standard Mommy Makeover typically takes between 4 and 6 hours, depending on the complexity of the breast and abdominal procedures. Longer surgeries may require an overnight hospital stay for monitoring.
A seroma is a collection of fluid under the skin. While drainless techniques have reduced this risk, it can still occur. The body reabsorbs small seromas, while larger ones may need to be drained with a needle in the office.
Most surgeons allow patients to shower 24 to 48 hours after surgery, once the initial dressings are removed or if waterproof glue was used. If drains are present, specific instructions will be given on how to manage them during showering.



Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)