Plastic surgery restores form and function through reconstructive procedures, cosmetic enhancements, and body contouring.
Send us all your questions or requests, and our expert team will assist you.
The consultation serves as the foundational diagnostic phase of the surgical journey. It is a rigorous medical appointment where the feasibility of the combined procedures is assessed against the patient’s physiological reality. The surgeon evaluates the interplay of anatomy, tissue quality, and general health.
During this session, the dialogue moves beyond aesthetic desires to clinical possibilities. The surgeon must identify any anatomical asymmetries or underlying hernias that could complicate the surgery. It is time to set realistic parameters based on the patient’s unique body structure.
comprehensive review of medical and surgical history
assessment of current medications and supplements
evaluation of scarring from previous surgeries, such as C-sections
discussion of lifestyle habits, including smoking and exercise
identification of specific aesthetic goals and concerns

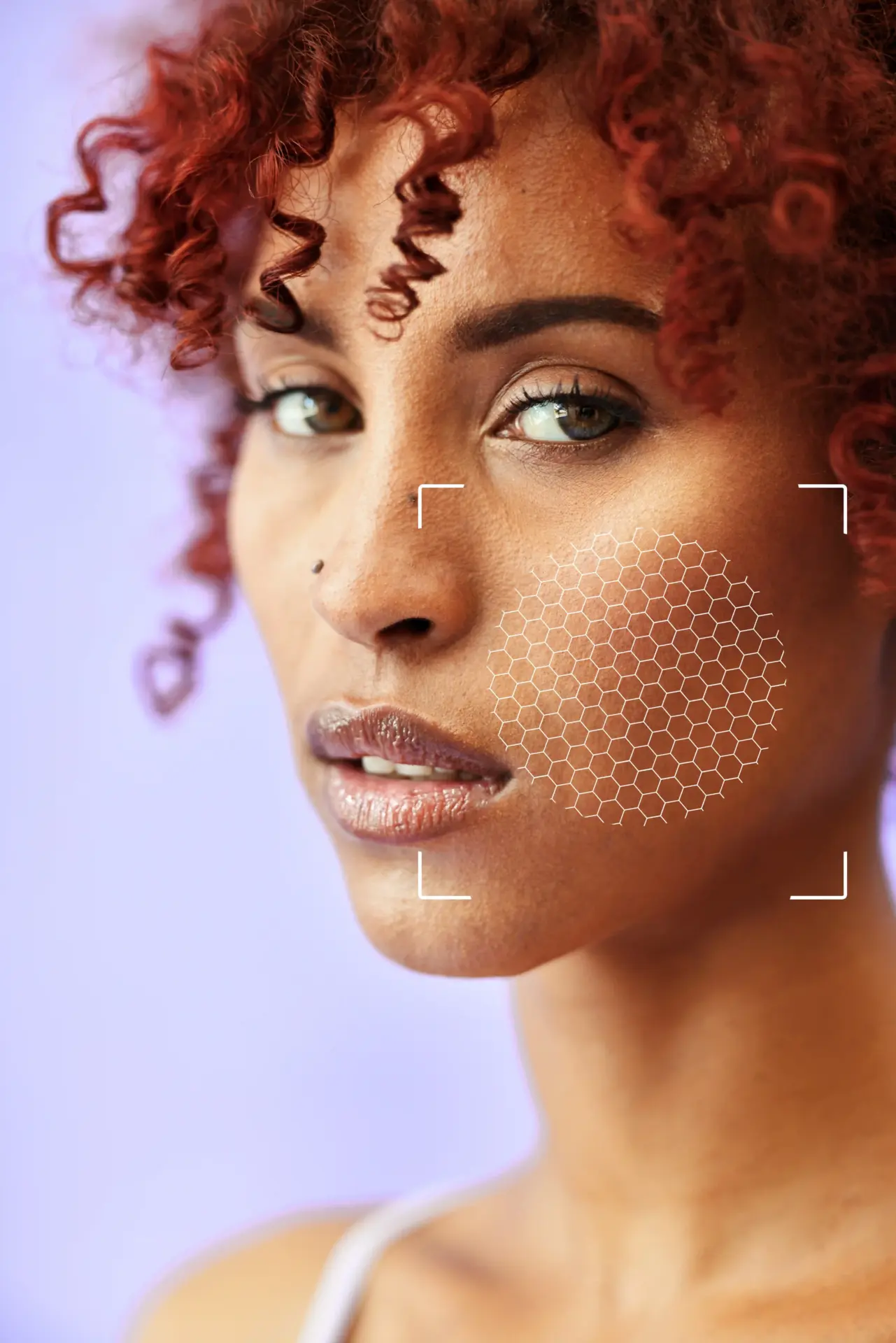
Modern consultations frequently utilize advanced imaging technology to bridge the gap between imagination and reality. 3D simulation tools enable surgeons to scan the patient’s body and generate a digital avatar. This avatar can be manipulated to show potential surgical outcomes for both breasts and the body.
Digital mapping allows for precise measurements of surface area and volume. This helps in planning the exact amount of skin excision, the size of breast implants, and the new nipple position. It serves as a visual communication tool that aligns the patient’s expectations with the surgeon’s technical plan.

Skin elasticity is a critical factor in determining the type of procedure for both the abdomen and breasts. Patients with poor elasticity are at higher risk of stretch marks or delayed wound healing when the skin is placed under excessive tension. The surgeon assesses the skin’s mobility to ensure it can be safely re-draped.
This assessment helps in deciding between a mini and a full abdominoplasty, and whether a breast lift is needed alongside augmentation. If the skin is loose and inelastic, simply filling it with an implant will lead to recurrent sagging; the skin envelope must be tightened.
Staging the integrity of the abdominal muscles involves determining the severity of the separation and the strength of the fascial tissue. A wide separation with thin, weak fascia requires a more aggressive plication technique. This step ensures the core repair is durable.
The surgeon also checks for the tone of the oblique muscles and the presence of any ventral hernias. Identifying these weaknesses preoperatively prevents intraoperative surprises and allows for a comprehensive repair plan that restores functional core strength.

Evaluating breast tissue involves assessing the volume of glandular tissue relative to fat and the degree of ptosis. The surgeon measures the distance from the sternal notch to the nipple to determine the extent of the lift required.
The quality of the breast parenchyma is also assessed. Women with dense, glandular breasts may require different surgical techniques than those with fatty, involuted breasts. This evaluation dictates whether implants, fat transfer, or auto augmentation (using the patient’s own tissue) is the best approach.
To ensure safety and optimal healing, patients must meet strict health criteria before scheduling surgery. This involves a battery of laboratory tests to check for anemia, clotting disorders, and nutritional deficiencies. The body must be in a metabolic state that supports rapid tissue repair.
Chronic conditions such as diabetes or hypertension must be perfectly managed. The surgeon will often coordinate with the patient’s primary care physician to obtain medical clearance. This rigor minimizes the risk of intraoperative and postoperative complications, especially given the length of combined surgeries.
Send us all your questions or requests, and our expert team will assist you.

Weight stability is non-negotiable for an optimal outcome. Patients are advised to reach their goal weight and maintain it for at least six months before the consultation. Fluctuating weight indicates that the body’s metabolic baseline is not yet established.
Operating on a patient who is actively losing weight can result in the recurrence of loose skin shortly after surgery. Conversely, operating on a patient with a high BMI increases the risk of wound healing problems and infection. The “ideal” candidate is weight stable and nutritionally sound.
Nicotine is a potent vasoconstrictor that significantly impairs blood flow to the skin. In a Mommy Makeover, where large flaps of skin are elevated on the tummy and breasts, proper blood flow is essential for survival of the tissue. Patients are strictly required to cease all nicotine products weeks before and after surgery.
Certain supplements and medications can also increase bleeding risk. The consultation includes a detailed review of all intake, including herbal remedies. Patients are given a “stop list” of substances to avoid to ensure the coagulation system functions normally during surgery.
For patients undergoing breast surgery, ensuring breast health is a priority. Women over a certain age, or those with a family history of breast cancer, are required to have a recent mammogram or ultrasound.
This screening ensures that there are no suspicious lesions or calcifications that need to be addressed before cosmetic surgery. It establishes a healthy baseline for future monitoring and ensures that the cosmetic procedure does not interfere with oncological safety.
A Mommy Makeover is a major life event with a significant recovery period. The consultation includes an assessment of the patient’s support system. Patients need to arrange for help with childcare and daily activities for the first few weeks.
Managing expectations is also crucial. The surgeon discusses the emotional rollercoaster of recovery, from the initial excitement to post-op fatigue. Preparing mentally for downtime ensures a smoother, less stressful recovery journey.
A high BMI is statistically linked to higher rates of complications such as seroma, infection, and poor wound healing. Most surgeons have a cutoff (often around 30-32) to ensure patient safety and the quality of the aesthetic result.
No, you must stop breastfeeding for at least 3 to 6 months before surgery. This allows the milk ducts to dry up and the breasts to return to their stable size, reducing the risk of infection (mastitis) and ensuring accurate sizing for the procedure.
If a patient tests positive for nicotine on the day of surgery or during the preoperative window, the surgery is typically cancelled or postponed. The risk of skin necrosis (tissue death) and nipple loss is too high to proceed safely.
3D simulations are sophisticated estimation tools, not guarantees. They provide an excellent approximation of volume changes and contour improvements, but they cannot perfectly predict how individual tissues will heal, settle, or react to gravity.
While not always mandatory, surgeons assess the patient’s emotional maturity and expectations during the consultation. If a patient displays signs of body dysmorphic disorder or unrealistic expectations, a formal psychological clearance may be requested.



Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)