Plastic surgery restores form and function through reconstructive procedures, cosmetic enhancements, and body contouring.
Send us all your questions or requests, and our expert team will assist you.
Advancements in surgical technique have introduced drainless abdominoplasty options. Traditional methods rely on suction drains to remove fluid accumulation between the skin and muscle. Drainless techniques use progressive-tension sutures to close the dead space internally.
By quilting the skin flap down to the underlying muscle fascia, the surgeon eliminates the space where fluid could collect. This technique reduces the patient’s postoperative physical burden and eliminates discomfort and scarring at drain sites.
Tissue glues and sealants are increasingly used to reinforce the closure and reduce complications. Fibrin sealants can be sprayed into the surgical pocket to promote adhesion and hemostasis. This biological glue mimics the body’s natural clotting process.
External skin glues provide a waterproof barrier over the incision line. This allows patients to shower earlier and protects the wound from bacteria. These modern adhesives contribute to a cleaner, more streamlined recovery process.
Microsurgical principles are applied to the dissection and closure phases. Surgeons use electrocautery with fine tips to dissect tissue with minimal thermal damage. This precision preserves the vascular network and lymphatic channels, which are essential for healing.
The incision is closed in multiple layers with fine, absorbable sutures. This distributes tension deep within the tissue, relieving pressure on the skin surface. The result is a finer, less visible scar that heals more reliably.
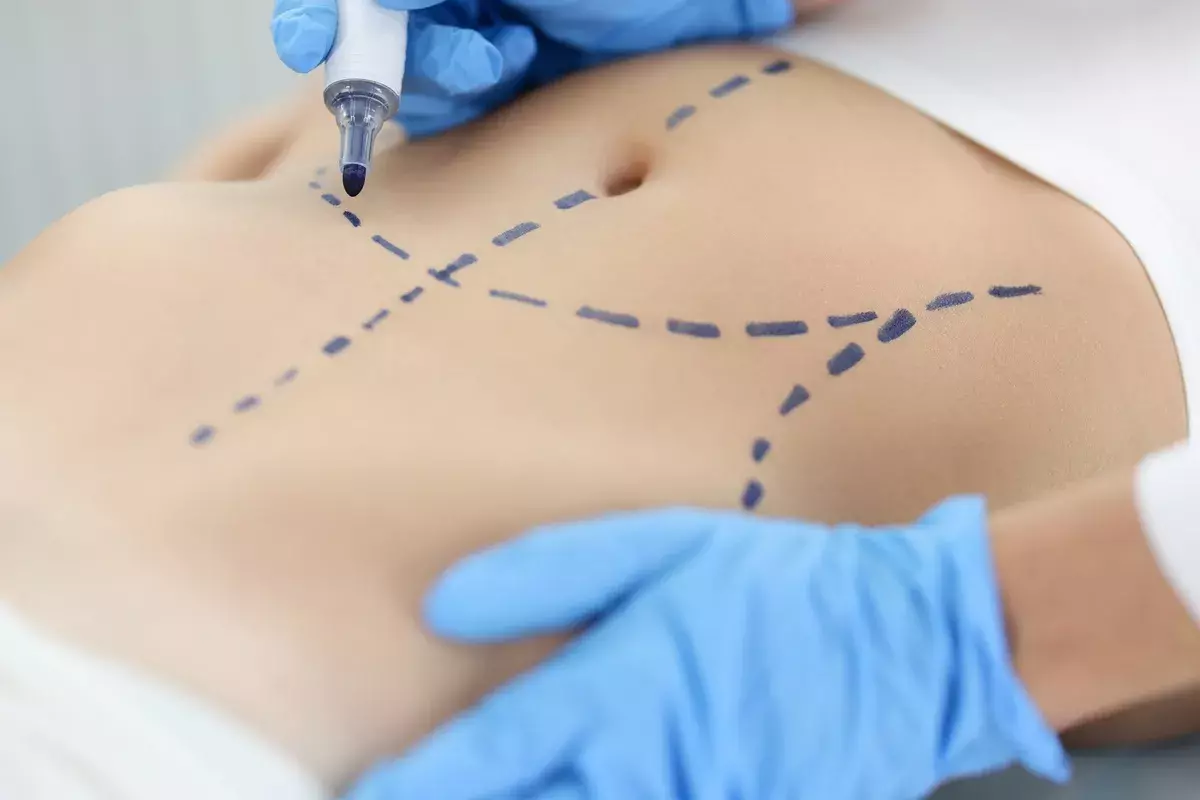
The surgical journey begins with meticulous preoperative preparation on the day of surgery. The surgical site is marked while the patient is standing to ensure symmetry and proper scar placement. The patient is prepped with antiseptic solutions to create a sterile field.
Compression devices are placed on the legs to prevent blood clots during the procedure. The anesthesia team administers medications to ensure the patient is comfortable and safe. This phase establishes a controlled, sterile surgical environment.

The surgery is typically performed under general anesthesia to ensure complete muscle relaxation. The surgeon makes the incision low on the pubis, extending towards the hips. The length is determined by the amount of skin to be removed.
The skin and fat are elevated off the abdominal wall up to the ribcage. The umbilicus is carefully detached from the surrounding skin but left attached to the muscle wall. This exposure allows for the repair of the diastasis recti.
The rectus muscles are plicated using heavy, permanent sutures. This tightens the abdominal wall and narrows the waist. Once the muscle repair is complete, the operating table is flexed to relieve tension on the skin.
The excess skin is pulled down and excised. A new opening is created for the belly button, and it is sutured into place. The incisions are then closed in layers, and dressings are applied.
Vaser Vibration Amplification of Sound Energy at Resonance technology is often integrated into the procedure. This ultrasound-assisted liposuction emulsifies fat cells before removal. It allows for precise sculpting of the flanks and upper abdomen.
Vaser is gentler on surrounding tissues than traditional liposuction. It preserves the connective tissue and blood vessels, leading to less bruising and better skin retraction. This tool refines the contours surrounding the tightened abdomen.
Laser-assisted systems may be used to treat the skin surface or to aid in coagulation. These devices deliver thermal energy to the dermis, stimulating collagen production and improving skin texture.
In some cases, laser therapy is used postoperatively to treat the incision line. This promotes faster fading of the scar and reduces redness. The integration of laser technology enhances the overall aesthetic finish of the surgery.
Advanced monitoring systems are utilized throughout the surgery to ensure patient safety. This includes continuous tracking of vital signs, oxygenation, and depth of anesthesia.
Postoperatively, bioimpedance or other monitoring tools may be used to assess fluid status and tissue health. These technologies provide real-time data that allows the medical team to intervene early if any irregularities arise.
Modern recovery protocols emphasize multimodal pain management. Surgeons often inject a long-acting local anesthetic called Exparel into the fascia of the muscle during surgery. This provides numbing relief for the first few days, reducing the need for narcotic pain medication.
This approach allows patients to mobilize sooner and experience less grogginess. Combining this with anti-inflammatories and muscle relaxants ensures a more comfortable recovery period.
Preventing blood clots is a significant focus during and after surgery. In addition to leg compression devices, patients are encouraged to walk shortly after waking from anesthesia.
Early ambulation stimulates blood flow and significantly reduces the risk of Deep Vein Thrombosis DVT. For high-risk patients, blood-thinning medication may be prescribed for a short period post-surgery.
Send us all your questions or requests, and our expert team will assist you.
You will likely feel tightness and soreness in your core, similar to doing too many sit-ups. This is the muscle repair healing. The sensation of tightness is normal and will gradually relax over the first few weeks.
The belly button stalk is preserved, and a new opening is made in the skin that is pulled down. The skin is then sutured to the stalk, often with a technique that hides the scar inside to create a natural-looking hood.
You will need to sleep and rest in a flexed position, with your head elevated and pillows under your knees. This “beach chair” position relieves tension on the incision and the repaired muscle.
Yes, if your surgeon uses waterproof skin glue, you can typically shower within 24 to 48 hours. You should let the water run gently over the area, but avoid scrubbing the incision or soaking in a bath.
Most patients walk slightly hunched over for the first week to protect the repair. You will gradually be able to stand straighter as the skin relaxes, typically achieving a whole upright posture by the end of the second week.



Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)