Plastic surgery restores form and function through reconstructive procedures, cosmetic enhancements, and body contouring.
Send us all your questions or requests, and our expert team will assist you.
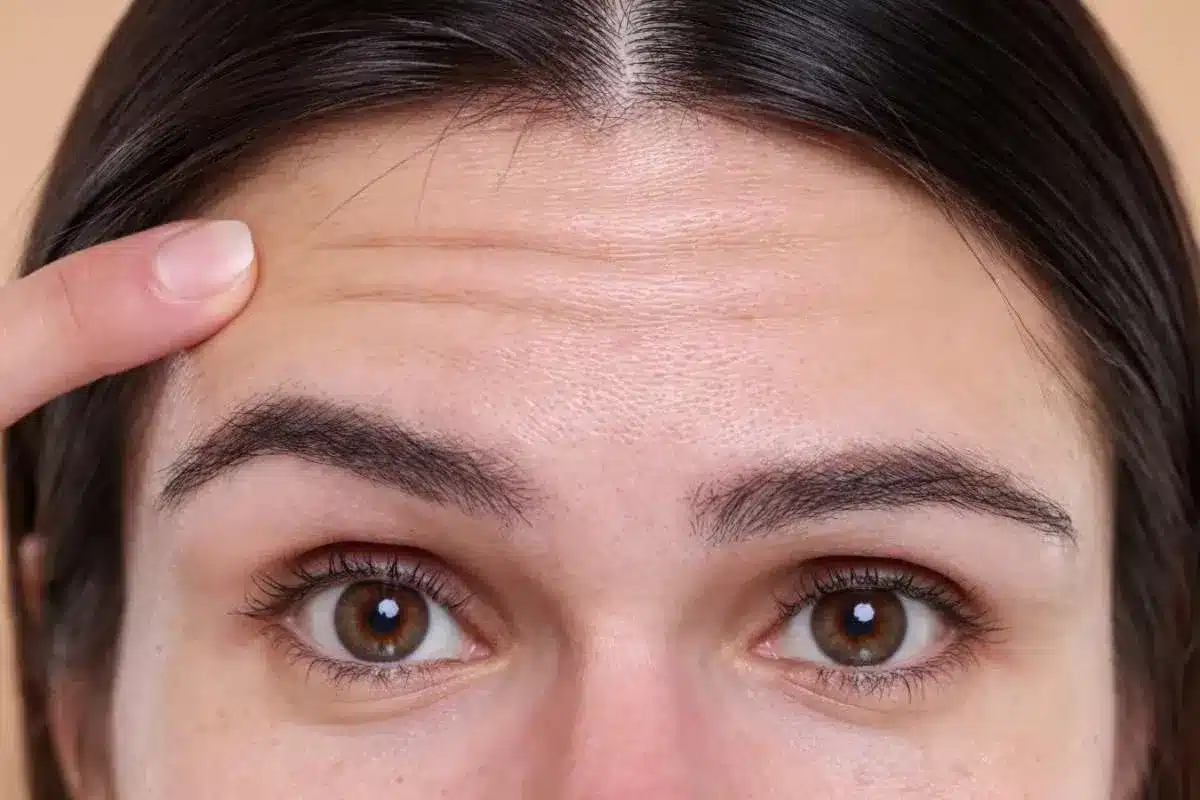
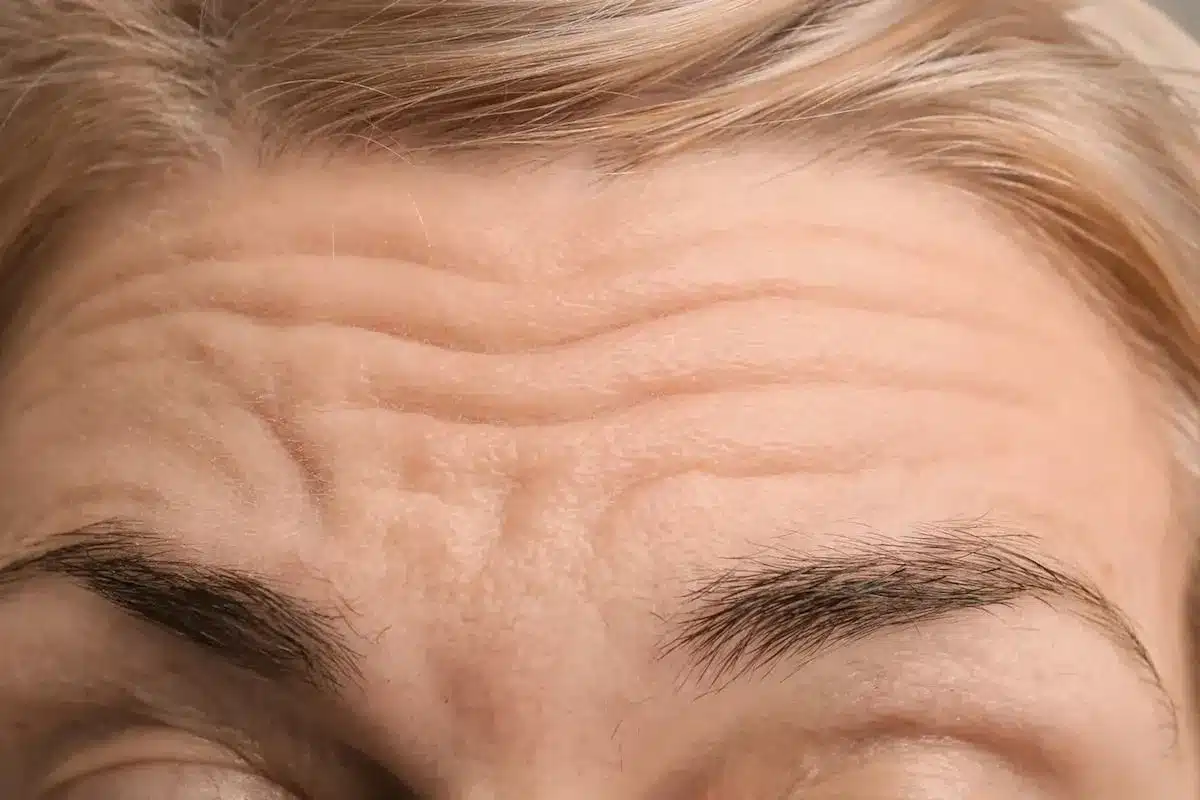
The consultation process is a rigorous diagnostic evaluation, not merely a cosmetic discussion. It involves a detailed analysis of the entire upper facial architecture. The surgeon evaluates the position of the eyebrows relative to the orbital rim, the quality of the forehead skin, and the strength of the underlying muscles.
This phase is critical for determining the specific technique required. The surgeon distinguishes between true eyelid excess and apparent excess due to brow descent. The goal is to formulate a surgical plan that addresses the root cause of the aging changes while respecting the patient’s unique anatomy.
Vector analysis involves determining the optimal direction of pull to achieve a natural lift. The surgeon manually simulates the lift to see how the skin redrapes. This helps determine whether a vertical lift or a lateral-diagonal lift will yield the best aesthetic outcome.
Hairline assessment is paramount. For patients with a high forehead, lifting the brow without careful consideration can further recede the hairline. In these cases, a pretrichial approach might be chosen to lower the hairline. Conversely, patients with low foreheads may benefit from the hairline elevation provided by endoscopic or coronal techniques.
The consultation must include a thorough evaluation of the upper eyelids. The surgeon checks for ptosis (droopy eyelid muscle) versus pseudoptosis (droopy skin). They assess the “glabellar slide” to see how much the brow contributes to the eyelid hooding.
Often, a brow lift is planned in conjunction with a blepharoplasty. However, the surgeon must be careful not to remove too much skin from the eyelid during a brow lift, as this could prevent the eye from closing properly (lagophthalmos). Precise measurements are taken to ensure safety.
Modern clinics utilize advanced 3D imaging technology to scan the patient’s face. This allows the surgeon to create a digital morph of the expected results. Patients can see a simulation of how different degrees of lift will alter their appearance.
This technology is invaluable for managing expectations. It allows the patient and surgeon to align on the desired arch shape and height. It serves as a visual communication tool to ensure that the surgical plan aligns with the patient’s aesthetic goals.

The physical quality of the forehead skin dictates the surgical approach. Thick, sebaceous skin may be more resistant to lifting and require more robust fixation. Thin, crepey skin may require gentler handling but might show irregularities more easily.
The surgeon performs a pinch test to assess turgor and recoil. This helps in predicting how the skin will settle after the procedure. It also influences the choice of fixation devices, such as Endotines or sutures, to ensure the lift holds over time.
The surgeon maps the forehead muscles’ activity by asking the patient to perform various expressions frowning, raising the eyebrows, and squinting. This reveals the strength and location of the depressor muscles (corrugators and procerus).
This mapping guides the surgical release. It tells the surgeon exactly which muscles need to be weakened or removed to stop the frowning and smooth the glabella. It allows for a targeted approach that preserves standard animation while reducing negative expressions.
A comprehensive review of the patient’s medical history is conducted to identify any contraindications. Conditions such as dry eye syndrome, previous facial surgeries, or bleeding disorders are carefully evaluated. Uncontrolled hypertension is a specific risk factor for hematoma.
The surgeon assesses the patient’s healing capacity. A history of keloids or poor scarring may influence incision placement. The goal is to stratify risk and optimize the patient’s physiology before they ever enter the operating room.
Because forehead lifting affects the eye area, ophthalmological health is crucial. Patients with a history of dry eyes, LASIK surgery, or glaucoma may need a clearance exam from an eye specialist.
Lifting the brow can slightly expose the eye more, potentially exacerbating dry eye symptoms. The surgeon performs a Schirmer’s test to measure tear production. Ensuring the eyes have adequate lubrication mechanisms is a mandatory safety step.
A detailed review of all medications and supplements is performed. Blood-thinning medications, including aspirin, NSAIDs, and certain herbal supplements (like fish oil, ginkgo, and vitamin E), must be stopped well in advance of surgery to prevent bleeding and bruising.
The surgeon provides a specific protocol for pausing and restarting medications. This minimizes the risk of hematoma, which is a collection of blood that can complicate recovery and compromise the aesthetic result.
Nicotine is a potent vasoconstrictor that severely impairs blood flow to the skin and healing tissues. In forehead lifts, where skin flaps are elevated, compromised blood flow can lead to skin necrosis (tissue death) and hair loss along the incision.
A strict cessation protocol is enforced. Patients are required to stop all nicotine products (cigarettes, vapes, patches) for at least 4 to 6 weeks before and after surgery. Urine testing may be used to verify compliance and ensure the safety of the surgical flap.
Healing requires energy and building blocks. Patients are advised to optimize their nutrition in the weeks leading up to surgery. A diet high in protein and vitamins supports tissue repair and immune function.
Hydration is also emphasized. Avoiding alcohol and salty foods helps reduce inflammation and swelling. The surgeon may recommend specific supplements, such as Arnica Montana or Bromelain, to help reduce bruising and speed recovery.
Psychological preparation isnecessarysary as physical preparation. The surgeon assesses the patient’s motivation and ensures they have realistic expectations. Patients must understand that the surgery offers improvement, not perfection, and that asymmetry is natural.
Discussion of the emotional aspect of recovery is included. The temporary “tight” feeling and the visible swelling can be distressing. Preparing the patient for the recovery journey helps them cope better with the temporary downtime.
Practical preparation is finalized during the pre-op visit. Patients are instructed to arrange for transportation and a caregiver for the first 24 to 48 hours. They are advised to set up a recovery station at home with pillows for elevation, ice packs, and easy-to-eat foods.
Work and social schedules should be cleared for at least 1 to 2 weeks. Organizing these logistics beforehand significantly reduces stress during the acute recovery phase, allowing the patient to focus entirely on healing.
Send us all your questions or requests, and our expert team will assist you.
No, you generally do not need to shave your head. For incisions within the hairline, the surgeon will part the hair and secure it with rubber bands or clips. The incisions are hidden within the hair
Symptoms include stinging, burning, or a gritty feeling in the eyes. During the consultation, your surgeon can perform a simple test to measure your tear production and determine whether you are at risk.
Yes, it is recommended to dye your hair a few days before surgery if you color it. You will not be able to use hair dye for about 4 to 6 weeks after the procedure while the incisions heal.
Smoking constricts blood vessels and cuts off oxygen to the healing skin. This can cause the skin around the incision to die, leaving a wide scar or bald spot. It is critical to stop completely.
If you have underlying health conditions like high blood pressure or diabetes, or are over a certain age, your surgeon will likely require a clearance note from your primary care doctor to ensure you are safe for anesthesia


Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)