Last Updated on November 26, 2025 by Bilal Hasdemir
Ovarian cancer is a complex disease with many risk factors. Nearly 80% of ovarian cancer cases are diagnosed in women over the age of 50. This makes age a big risk factor.
There isn’t a single known cause, but knowing the risk factors is important. Factors like family history, genetic mutations, and lifestyle choices can affect a woman’s risk.
Key Takeaways
- Age is a significant risk factor for ovarian cancer.
- Family history and genetic mutations can increase the risk.
- Lifestyle choices may also impact ovarian cancer risk.
- Understanding risk factors is key to prevention.
- Ovarian cancer risk factors are multifaceted.
Understanding Ovarian Cancer

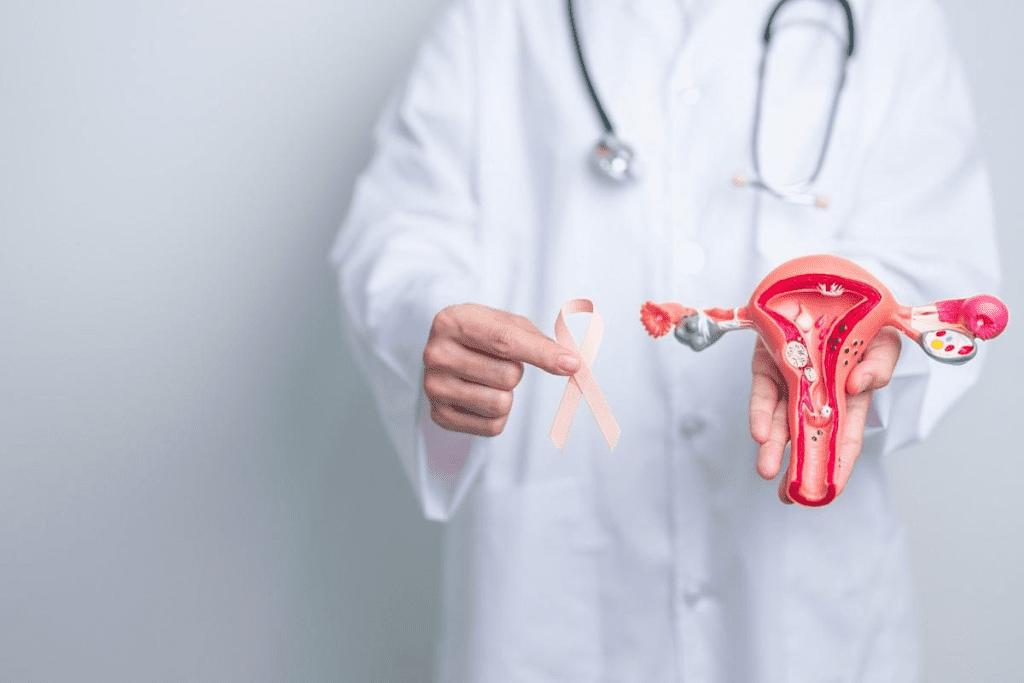
It’s important to know about ovarian cancer to catch it early and treat it well. Ovarian cancer starts in the ovaries. These organs make eggs and hormones.
What is Ovarian Cancer?
Ovarian cancer starts in the ovaries. This is where eggs are made and hormones like estrogen and progesterone are produced. It can take different forms based on the cells involved.
Definition and Basic Pathology
Ovarian cancer is when abnormal cells grow out of control in the ovaries. This can cause tumors, some of which are harmless, while others are dangerous.
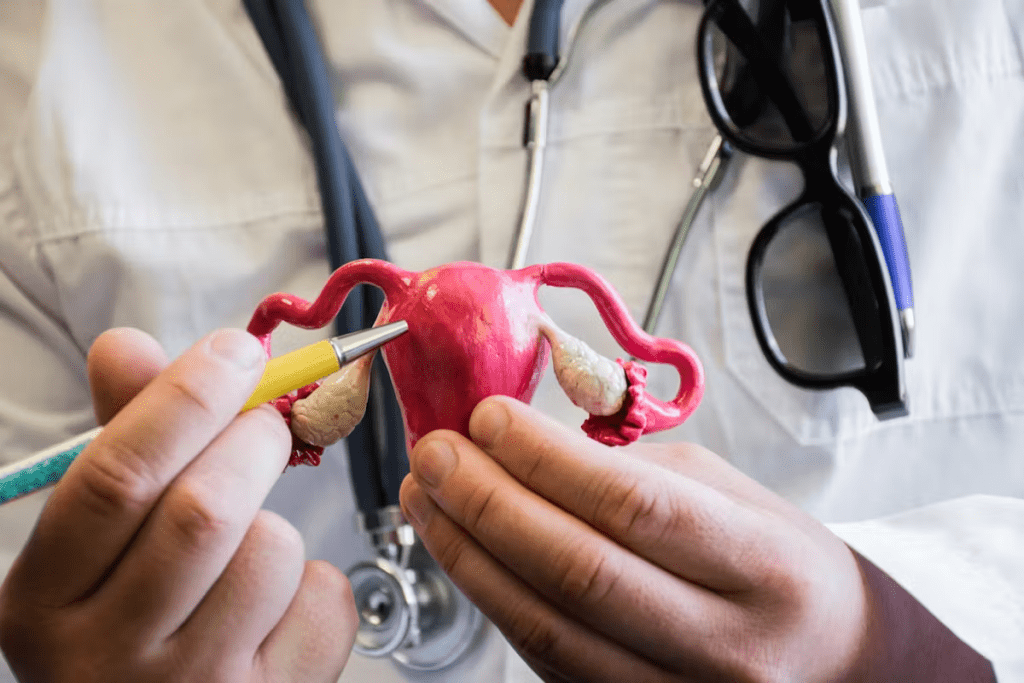
How Cancer Develops in the Ovaries
Cancer in the ovaries starts with a genetic mutation in the cells. This mutation makes cells divide without stopping. Many things can cause this, like genes and hormones.
Types of Ovarian Cancer
Ovarian cancer comes in several types, based on the cells affected. The most common is epithelial ovarian cancer. It starts in the outer layer of the ovary.
Prevalence and Statistics in the United States
Ovarian cancer is a significant health concern in the United States. Every year, thousands of new cases are found. It’s often found late, so knowing the risks and causes is key to catching it early.
Genetic changes, like in the BRCA1 and BRCA2 genes, raise the risk of ovarian cancer. Knowing about these genetic factors helps find people at high risk.
Recognizing Ovarian Cancer Symptoms
It’s important to know the symptoms of ovarian cancer early. This can help in getting the right treatment. Ovarian cancer often shows symptoms that can be mistaken for other, less serious issues.
Early Warning Signs
Look out for these early signs of ovarian cancer:
- Abdominal bloating or swelling
- Quickly feeling full when eating
- Weight loss
- Discomfort in the pelvic area
These symptoms are often mild. They can be caused by many things, so it’s key to notice any changes in your body.
Advanced Symptoms
When ovarian cancer gets worse, symptoms can get more serious. They might include:
- Fatigue
- Back pain
- Changes in bowel habits
- A frequent need to urinate
Remember, these symptoms can also mean other health problems. But if they keep happening, seeing a doctor is a must.
When to See a Doctor
If you notice any symptoms, like those mentioned, it’s time to see a doctor. Early detection is key to treating ovarian cancer effectively.
Being proactive about your health and talking to your doctor about any worries can really help.
Genetic Mutations: The Primary Cause of Ovarian Cancer
Certain genetic mutations, like BRCA1 and BRCA2, are key causes of ovarian cancer. They affect DNA repair. This makes it harder for the body to fix DNA damage, raising cancer risk.
BRCA1 and BRCA2 Mutations
The BRCA1 and BRCA2 genes help fix damaged DNA. Mutations in these genes can increase the risk of breast and ovarian cancers.
How These Mutations Increase Risk
With BRCA1 or BRCA2 mutations, DNA damage isn’t fixed. This leads to more genetic changes that can cause cancer. Women with these mutations face a higher risk of ovarian cancer.
Prevalence in the Population
About 1 in 400 to 1 in 800 people have a BRCA1 or BRCA2 mutation. The number varies by ethnic background.
Lynch Syndrome and Other Hereditary Conditions
Lynch syndrome, or hereditary nonpolyposis colorectal cancer (HNPCC), raises ovarian cancer risk. It also increases the risk of colorectal and other cancers. Other hereditary conditions may also play a role, though less commonly.
Genetic Testing for Ovarian Cancer Risk
Genetic testing can find mutations that raise ovarian cancer risk. It’s vital for women with a family history of breast or ovarian cancer.
Who Should Consider Testing
Women with a strong family history of breast or ovarian cancer should think about genetic testing. This includes those with multiple relatives affected at a young age. Testing is also suggested for those with known genetic syndromes.
Understanding Test Results
Test results can be complex. A positive result means a mutation is found. A negative result doesn’t mean no risk. Genetic counseling is key for understanding results and making choices.
Knowing about genetic mutations is vital for understanding personal risk. It helps make choices about preventive measures and surveillance.
Family History and Hereditary Factors
Knowing how family history affects ovarian cancer risk is key to early detection and prevention. Research shows that women with a family history of ovarian or breast cancer face a higher risk. This is because they might carry genes that increase their risk.
First-Degree Relatives with Ovarian Cancer
Having a mother, sister, or daughter with ovarian cancer raises a woman’s risk. Studies reveal that the risk is even higher if many first-degree relatives have been diagnosed. It’s also higher if they were diagnosed young.
Breast Cancer in the Family
The connection between breast and ovarian cancer is strong, thanks to BRCA1 and BRCA2 genes. Families with a history of early breast cancer may also face a higher risk of ovarian cancer.
Genetic Counseling for High-Risk Families
Genetic counseling is vital for families with ovarian or breast cancer history. Counselors review family medical history, discuss genetic testing, and explain the risks. This helps individuals understand their risk and make informed health choices.
What to Expect from Genetic Counseling
Genetic counseling involves reviewing family medical history and discussing genetic risks. Counselors explain the implications of genetic testing. This helps individuals grasp their risk and decide on preventive measures.
Making Informed Decisions Based on Family History
Genetic counseling provides the information needed to make health decisions. This might include more frequent screenings, preventive surgeries, or other strategies to reduce risk.
| Family History | Risk Level | Recommended Action |
| No family history of ovarian or breast cancer | Average risk | Follow standard screening guidelines |
| One first-degree relative with ovarian or breast cancer | Moderate risk | Consider genetic counseling and earlier screening |
| Multiple first-degree relatives with ovarian or breast cancer | High risk | Genetic counseling and consider preventive measures |
Genetic counseling is essential for those with a significant family history of ovarian or breast cancer. Understanding their risk allows women to take proactive steps to safeguard their health.
Age as a Risk Factor
As women get older, their chance of getting ovarian cancer goes up. This risk jumps after the fifth decade of life. Most ovarian cancer cases happen in women over 50, showing how important age is.
Ovarian Cancer Risk by Age Group
The risk of ovarian cancer changes with age. Women under 40 face a lower risk, but it grows as they get older. The highest risk is between 60 and 70 years old, based on data.
| Age Group | Ovarian Cancer Risk |
| Under 40 | Low |
| 40-49 | Moderate |
| 50-59 | High |
| 60-70 | Very High |
| Over 70 | Highest |
Post-Menopausal Risk Increase
After menopause, the risk of ovarian cancer goes up a lot. The drop in estrogen levels during menopause can cause changes that may lead to cancer. Women should talk to their doctors about these risks.
Age-Related Cellular Changes
As we age, our cells change in ways that can lead to cancer, including ovarian cancer. Telomere shortening and genetic mutations are key factors. Knowing about these changes helps women understand their risk and take steps to prevent it.
By understanding how age affects ovarian cancer risk, women can better manage their risk. They can take steps to prevent it with the help of healthcare professionals.
Causes of Ovarian Cancer: Hormonal Factors
Estrogen exposure, pregnancy, and the timing of menstruation and menopause affect ovarian cancer risk. Knowing these factors helps understand individual risk. It also helps in reducing the chance of getting ovarian cancer.
Estrogen Exposure and Ovarian Cancer
Estrogen exposure over a woman’s life is a big risk factor for ovarian cancer. The more estrogen a woman’s ovaries are exposed to, the higher her risk. This idea is called the “incessant ovulation” hypothesis.
Prolonged estrogen exposure happens for many reasons. Early menstruation and late menopause are two of them. “Women who start menstruating before age 12 and enter menopause after age 55 have a higher cumulative estrogen exposure,” studies say. This can increase their risk of ovarian cancer.
Impact of Pregnancy and Breastfeeding
Pregnancy and breastfeeding reduce the risk of ovarian cancer. During pregnancy, the ovaries stop releasing eggs. This break from ovulation is thought to lower the risk of genetic errors that can lead to cancer.
How Pregnancy Reduces Risk
Each full-term pregnancy lowers a woman’s risk of ovarian cancer. The biggest risk reduction comes from the first pregnancy. The exact reasons are not fully understood. But, hormonal changes during pregnancy, like the decrease in estrogen and progesterone after childbirth, may play a role.
Number of Pregnancies and Risk Correlation
Women with multiple pregnancies have a lower risk of ovarian cancer. “The risk of ovarian cancer decreases with increasing number of pregnancies,” studies show. This highlights the protective effect of pregnancy.
Early Menstruation and Late Menopause
Women with early menstruation and late menopause are exposed to more estrogen. This can increase their risk of ovarian cancer. Prolonged estrogen exposure is thought to stimulate the growth of ovarian cells. This can lead to cancerous changes.
“Factors such as early menstruation, late menopause, and never having been pregnant may increase ovarian cancer risk due to increased estrogen exposure.”
Understanding these hormonal factors is key. It helps women and their healthcare providers assess risk. It also helps in considering preventive measures or closer monitoring.
Medical Conditions Linked to Ovarian Cancer
Certain medical conditions have been linked to an increased risk of ovarian cancer. This shows how important it is to understand these connections. Research has found several conditions that may raise the risk.
Endometriosis and Ovarian Cancer Risk
Endometriosis is a condition where tissue like the uterus lining grows outside it. It has been linked to a higher risk of ovarian cancer. Studies show women with endometriosis are more likely to get ovarian cancer.
Mechanisms Behind the Connection
The exact reasons for the link between endometriosis and ovarian cancer are not clear. But, chronic inflammation and hormonal factors are thought to play a part.
Monitoring for High-Risk Patients
Women with endometriosis should know their increased risk. They should talk to their healthcare provider about monitoring. Regular check-ups and screenings can help find issues early.
Polycystic Ovary Syndrome (PCOS)
Polycystic ovary syndrome (PCOS) is a hormonal disorder in women of reproductive age. Some studies suggest PCOS may be linked to a higher risk of ovarian cancer. But, more research is needed to confirm this.
Pelvic Inflammatory Disease
Pelvic inflammatory disease (PID) is an infection of the female reproductive organs. Research suggests PID may be linked to a higher risk of ovarian cancer. This could be due to chronic inflammation.
“Understanding the relationship between these medical conditions and ovarian cancer risk is key for early detection and prevention.” By knowing these links, women can take steps to monitor their health and lower their risk.
Lifestyle and Environmental Risk Factors
Ovarian cancer risk is influenced by lifestyle choices and environmental exposures. Research is uncovering the complex factors behind this disease. Understanding lifestyle and environment is key.
Obesity and Ovarian Cancer
Being overweight or obese raises ovarian cancer risk. Obesity is linked to higher inflammation and hormonal changes, which may lead to cancer.
BMI Correlation with Risk
Studies link Body Mass Index (BMI) to ovarian cancer risk. A higher BMI is associated with increased risk, mainly in postmenopausal women.
Fat Tissue and Hormone Production
Fat tissue is not just for storing fat; it’s active in hormone production. Excess body fat can increase estrogen production, which may stimulate ovarian cancer cells.
Diet and Nutrition Impact
Diet and nutrition are key in ovarian cancer risk. A diet rich in fruits, vegetables, and whole grains may lower risk. A diet high in processed foods and saturated fats may increase it.
Environmental Toxins and Exposures
Exposure to certain environmental toxins raises ovarian cancer risk. Understanding these risks is important for prevention.
Talcum Powder Controversy
The use of talcum powder in the genital area is controversial. Some studies suggest a link to ovarian cancer. While not all studies agree, the risk is a concern for many women.
Industrial Chemicals and Pollutants
Exposure to industrial chemicals and pollutants is another risk factor. Reducing exposure to these substances can lower ovarian cancer risk.
By understanding and addressing these risk factors, women can take steps to lower their ovarian cancer risk.
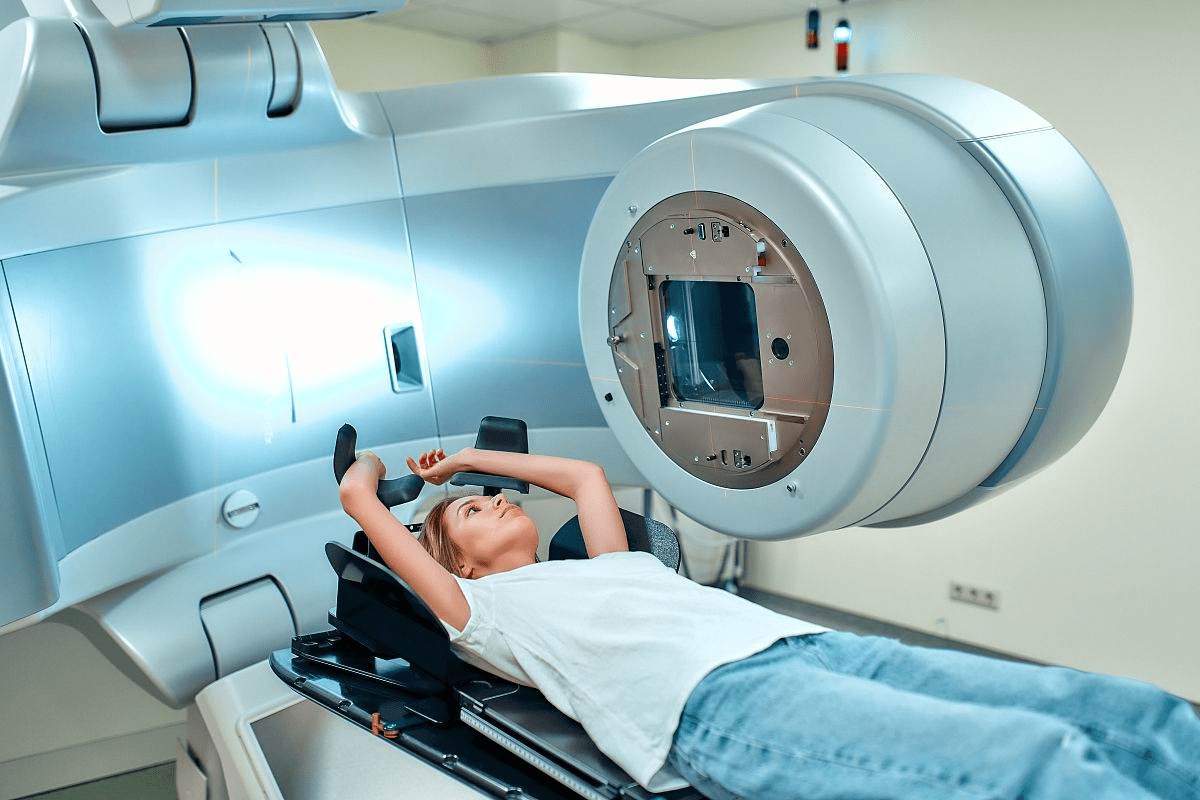
Medical Treatments and Interventions
Medical treatments, like fertility treatments and hormone replacement therapy, have been studied for their link to ovarian cancer. Some treatments can change a woman’s risk of getting ovarian cancer.
Fertility Treatments and Ovarian Cancer Risk
Fertility treatments are getting more common. Researchers are looking into how they might affect ovarian cancer risk. Some studies hint at a possible link, but the findings are not solid yet.
“The relationship between fertility treatments and ovarian cancer risk remains a topic of ongoing research and debate.”
Nature Reviews Cancer
A study in the Journal of Clinical Oncology found a slight link between fertility drugs and ovarian cancer. This was true for women who had never given birth or had a family history of cancer.
| Fertility Treatment Type | Ovarian Cancer Risk |
| Clomiphene Citrate | Moderate Increase |
| Gonadotropins | Potential Increase |
| In Vitro Fertilization (IVF) | Limited Evidence |
Hormone Replacement Therapy Considerations
Hormone replacement therapy (HRT) helps with menopause symptoms. Some studies suggest HRT might raise ovarian cancer risk, mainly with estrogen-only therapy.
Key Considerations for HRT:
- How long you use HRT
- What kind of HRT you take (estrogen-only vs. estrogen-progestin)
- Your personal risk for ovarian cancer
Gynecological Surgeries and Their Impact
Surgeries like tubal ligation and hysterectomy might lower ovarian cancer risk. This is because they change the ovaries or fallopian tubes.
It’s important to know how these treatments affect ovarian cancer risk. Women should talk to their doctors about their risks and treatment options.
Protective Factors and Risk Reduction Strategies
Understanding protective factors and risk reduction strategies is key to preventing ovarian cancer. This knowledge empowers women to take steps to lower their risk.
Oral Contraceptives as Protection
Using oral contraceptives can greatly reduce ovarian cancer risk. Studies show women who use them have a lower risk than those who don’t.
Duration of Use and Risk Reduction
The longer a woman uses oral contraceptives, the more her risk drops. This shows a clear link between use time and risk reduction.
Considerations for High-Risk Women
Women at high risk, like those with BRCA1 or BRCA2 mutations, may benefit from oral contraceptives. But, they should talk to their doctor first. This is to consider their health and risk level.
Tubal Ligation and Hysterectomy
Surgeries like tubal ligation and hysterectomy may lower ovarian cancer risk. Though the exact reasons are unclear, these surgeries offer some protection.
Lifestyle Changes for Risk Reduction
Changing your lifestyle can also help lower ovarian cancer risk. Staying at a healthy weight, exercising regularly, and eating well are good steps.
Screening Options for High-Risk Women
High-risk women can benefit from special screenings to catch ovarian cancer early. These include:
CA-125 Blood Test
The CA-125 blood test checks for a protein that can signal ovarian cancer.
Transvaginal Ultrasound
Transvaginal ultrasound helps spot any oddities in the ovaries.
| Screening Method | Description | Benefit for High-Risk Women |
| CA-125 Blood Test | Measures CA-125 protein levels in the blood | Early detection of ovarian cancer |
| Transvaginal Ultrasound | Imaging test to identify ovarian abnormalities | Early detection and monitoring |
Conclusion: Understanding Your Personal Risk
Knowing your personal risk factors is key to preventing and catching ovarian cancer early. By understanding what increases your risk, you can take steps to lower it. This helps protect you from this serious disease.
This article has explained the main risk factors for ovarian cancer. These include genetic mutations, family history, age, hormonal factors, and lifestyle choices. Knowing these can help you figure out your own risk and make smart health choices.
To prevent ovarian cancer, awareness, genetic testing, and lifestyle changes are important. If you’re at high risk, regular check-ups and talking to your doctor can help. This way, you can lower your risk.
By learning about your risk and taking steps to reduce it, you can take control of your health. This empowers you to make choices that are good for your reproductive health and overall well-being.
FAQ
What is the main risk factor for developing ovarian cancer?
The main risk factor is a family history of ovarian cancer, mainly in first-degree relatives. Genetic mutations like BRCA1 and BRCA2 also play a big role.
How do genetic mutations like BRCA1 and BRCA2 affect ovarian cancer risk?
BRCA1 and BRCA2 mutations raise the risk of ovarian cancer. They make it hard for the body to fix DNA damage, leading to cancer cells.
Can hormonal factors influence ovarian cancer risk?
Yes, hormonal factors like estrogen exposure can affect risk. Early menstruation and late menopause also play a part. Pregnancy and breastfeeding may lower the risk.
How does age impact ovarian cancer risk?
Risk increases with age, more so after menopause. This is due to cellular changes and exposure to harmful substances over time.
Is there a link between endometriosis and ovarian cancer?
There might be a link between endometriosis and certain types of ovarian cancer. But the exact reasons are not fully understood.
Can lifestyle factors such as obesity and diet affect ovarian cancer risk?
Yes, obesity and a diet high in certain fats can increase risk. Eating well and staying healthy can help lower it.
Do fertility treatments increase the risk of ovarian cancer?
The link between fertility treatments and ovarian cancer is complex. Some studies suggest a higher risk, mainly with certain medications.
How can oral contraceptives impact ovarian cancer risk?
Oral contraceptives can lower ovarian cancer risk. The more you use them, the greater the protection.
What screening options are available for high-risk women?
High-risk women might get regular screenings with ultrasound and CA-125 blood tests. But, these methods’ effectiveness for early detection is being studied.
Can certain surgeries reduce ovarian cancer risk?
Yes, surgeries like tubal ligation and hysterectomy can lower risk. But, the decision to have these surgeries should be personal.
How does hormone replacement therapy (HRT) affect ovarian cancer risk?
HRT might slightly increase ovarian cancer risk, mainly with long-term use. But, the overall risk is low.
Are there any environmental toxins that can increase ovarian cancer risk?
Exposure to toxins like talc and pesticides might raise risk. But, more research is needed to confirm this.
References
- National Cancer Institute. (2023). Ovarian, fallopian tube, and primary peritoneal cancer”Patient version. https://www.cancer.gov/types/ovarian