Clinical Immunology focuses on the immune system’s health. Learn about the diagnosis and treatment of allergies, autoimmune diseases, and immunodeficiencies.
Send us all your questions or requests, and our expert team will assist you.

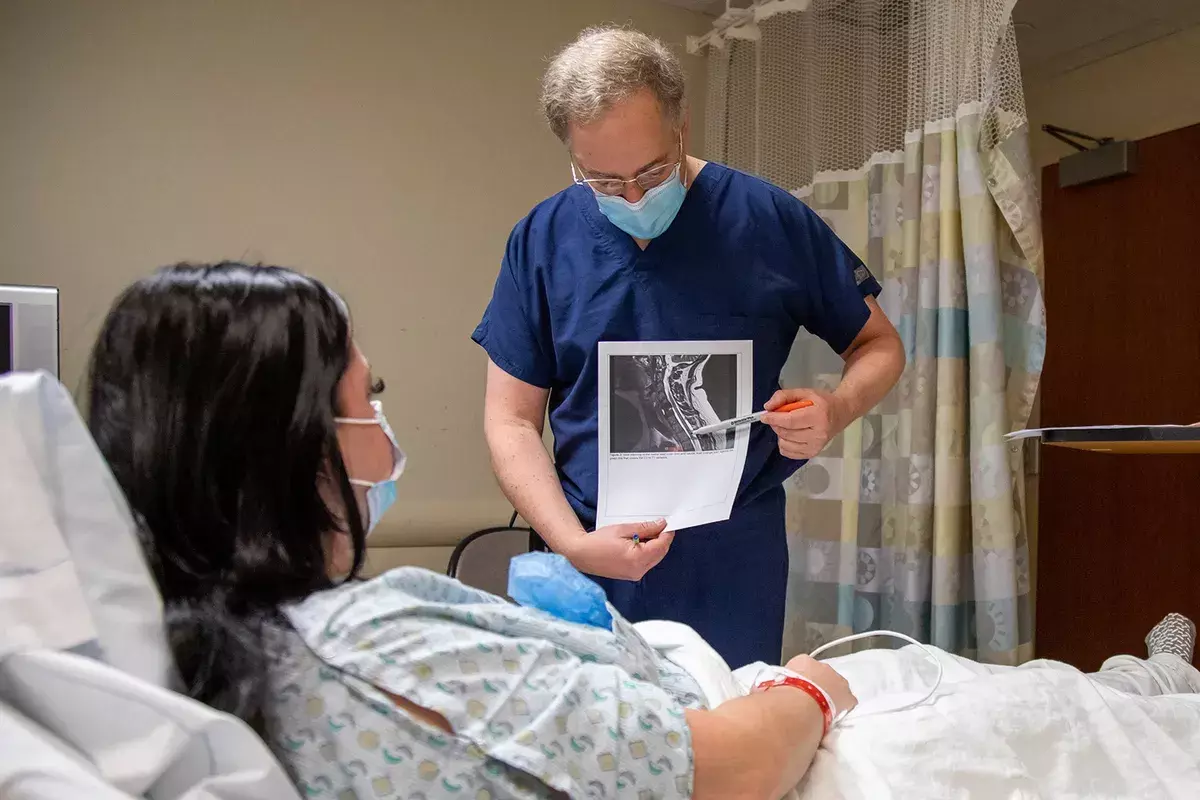
Diagnosing Myasthenia Gravis can be hard because weakness is a common symptom in many illnesses. This often means there is a delay before getting a clear diagnosis. Doctors use a mix of physical exams, blood tests, nerve tests, and scans to confirm MG and rule out other conditions like stroke or thyroid problems.

The neurologist will perform a detailed examination to elicit “fatigability,” the signature of MG.
This is a simple, non-invasive test used when a patient has a drooping eyelid.
Utility: It is susceptible for ocular myasthenia but cannot diagnose generalized weakness.

Blood tests are the first-line confirmatory tests. They look for the specific autoantibodies that cause the disease.
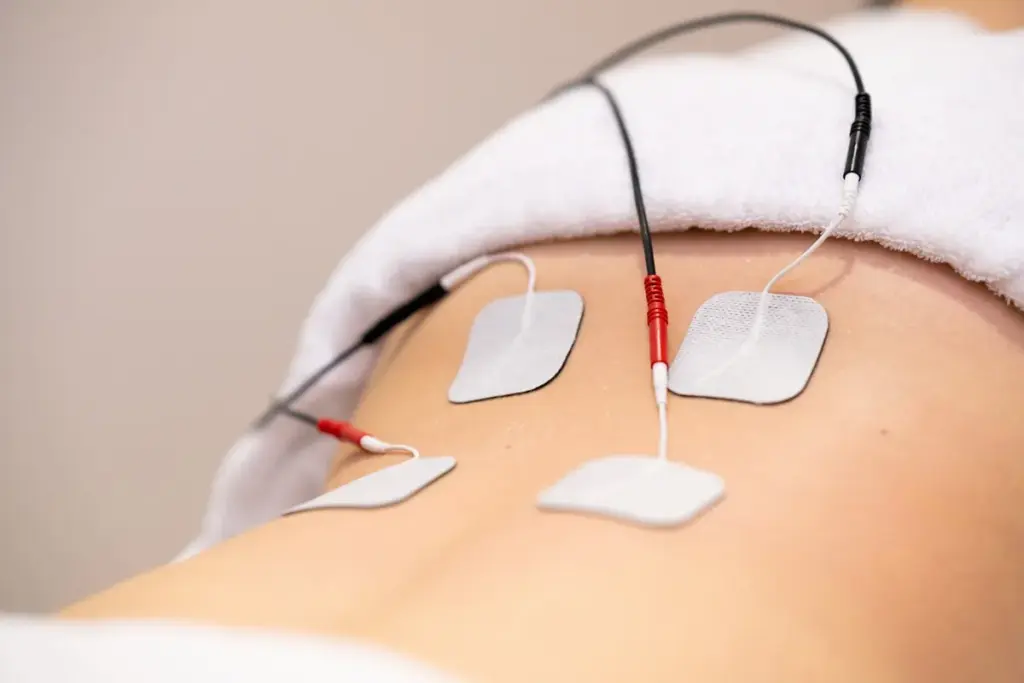
RNS is the most frequently used electrodiagnostic test for MG.
Sensitivity: It is more sensitive in generalized MG than in purely ocular cases.
When other tests are inconclusive, SFEMG is considered the most sensitive diagnostic tool available.
Indication: Usually reserved for complex cases or seronegative patients.
Once the diagnosis is suspected or confirmed, imaging is crucial to evaluate the thymus gland.
Though less common today due to cardiac risks, pharmacological challenge tests were historically the gold standard.
Because respiratory weakness is the most dangerous aspect of MG, evaluating lung function is part of the diagnostic workup.
Sleep Studies: May be used to check for sleep apnea, which is dangerous in MG patients with bulbar weakness.

Send us all your questions or requests, and our expert team will assist you.
It can be slightly uncomfortable because it involves a very thin needle electrode, but it is generally well tolerated and safe.
You may have “seronegative” MG. In this case, diagnosis relies on the clinical exam and electrodiagnostic tests, such as SFEMG.
To check for a thymoma. Even if you don’t have a tumor, the thymus gland might be enlarged, and checking it is standard care.
Generally, yes. However, you should confirm with your doctor, especially if you are having a CT scan with contrast dye.
They feel like small taps or snaps against the skin. They are not harmful, and the sensation stops immediately upon completion of the test.



Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)