Geriatrics addresses the health needs of older adults, focusing on frailty, dementia, falls, and chronic disease management.
Send us all your questions or requests, and our expert team will assist you.
Today, Diabetes Mellitus is understood as more than just high blood sugar or not enough insulin. Regenerative medicine and geriatrics now describe it as a complex disorder that involves issues with cell communication, ongoing low-level inflammation, and a reduced ability for the body to repair itself. This new perspective shifts the focus from only managing glucose to also protecting and restoring pancreatic beta-cell function and overall metabolic balance. It also takes into account how aging cells affect metabolism and contribute to disease.
Regenerative medicine explains that our bodies have stem cells and repair systems to keep tissues healthy, but in diabetes, these repair processes fail. In Type 1 diabetes, the immune system attacks cells, while in Type 2, stress on the cells leads to their death. Both types result in the loss of insulin-producing beta cells in the pancreas. Modern treatments now try to prevent this loss and help these cells recover, which is a big change from older methods that accepted decline as unavoidable.
Research into cell-based solutions for diabetes is important, especially as more people develop metabolic problems as they age. High blood sugar often points to larger health issues, showing that the body’s hormones, immune system, and blood vessels are out of balance. In regenerative medicine, diabetes is seen as a cause of faster aging throughout the body. High blood sugar produces harmful byproducts that damage proteins and DNA in organs like the eyes and kidneys.
Key biological characteristics defining the regenerative view of diabetes include:
Regenerative treatments for diabetes are based on the idea of the “pancreatic ecosystem.” This means that beta cells do not work alone but depend on a complex environment made up of blood vessels, immune cells, and supporting tissue. Modern science sees diabetes as a breakdown of this support system. In Type 1 diabetes, the immune system attacks the body’s own tissues, making the environment harmful. In Type 2 diabetes, amyloid deposits and scar tissue build up and block the islets, stopping them from sensing glucose and releasing insulin properly.
Regenerative treatments aim to rebuild the pancreatic environment. This involves more than just adding new cells; it also means calming the immune system and reducing scar tissue so cells can communicate better. Mesenchymal stem cells are used mainly to send helpful signals, not to become new beta cells. They release molecules that fight inflammation and help control the immune response. By viewing diabetes as a problem with the cell environment, doctors can use these tools to reset the immune system and support tissue repair.
This ecosystem idea also applies to the liver and muscles, which are the main places where insulin works. In metabolic syndrome and Type 2 diabetes, these tissues become resistant to insulin. Regenerative medicine sees this resistance as something that can be reversed. By targeting the receptors and cell signals that have stopped working well, treatments aim to restore insulin sensitivity. This helps the body use its own insulin better and eases the burden on the pancreas. The definition of diabetes now includes how the pancreas interacts with muscles, liver, and fat.

Geriatric medicine is important for understanding diabetes, especially as more older adults are affected. The idea of “immunosenescence,” or the gradual weakening of the immune system, is key. As the immune system ages, it becomes less accurate and causes ongoing, low-level inflammation called “inflammaging.” This inflammation disrupts insulin signaling, directly connecting aging to high blood sugar. So, in older people, diabetes is often seen not just as a metabolic disease but also as a sign of faster biological aging.
In older adults, diabetes is closely tied to frailty and muscle loss (sarcopenia). Skeletal muscle uses the most glucose in the body. As people age and lose muscle, the body’s ability to use glucose drops, causing higher blood sugar. This leads to a cycle where high blood sugar causes more muscle loss, making things worse. New care plans for older adults focus on both controlling blood sugar and keeping muscle mass and independence. This approach makes sure treatments support the patient’s overall health.
The aging brain is also very sensitive to changes in metabolism. More research is showing that insulin resistance is linked to memory loss and brain diseases. Some experts even call Alzheimer’s disease “Type 3 Diabetes” to show how important insulin is for brain health. Because of this, a full definition of diabetes in regenerative medicine must include its effects on the brain. Diabetes can threaten a person’s mental sharpness. Treatments are judged not just by how well they lower A1C, but also by how well they protect the brain and keep thinking skills strong.

To understand the regenerative approach, one must delve into the cellular mechanisms that define the disease state. At the heart of the pathology lies oxidative stress. High levels of glucose generate reactive oxygen species (free radicals) that overwhelm the cell’s natural antioxidant defenses. Pancreatic beta cells are uniquely vulnerable to this stress because they lack robust antioxidant enzymes. This oxidative damage triggers pathways of apoptosis (programmed cell death) and senescence (a zombie-like state in which cells stop dividing but continue secreting inflammatory toxins).
Regenerative medicine defines diabetes as a state of “oxidative exhaustion.” Therapeutic interventions often focus on boosting cells’ antioxidant capacity or on introducing stem cells that can transfer healthy mitochondria to damaged cells. This process, known as mitochondrial transfer, revitalizes beta-cell energy production, allowing them to resume normal function. This biological rescue operation is distinct from pharmaceutical management, which typically forces the remaining beta cells to work harder, potentially accelerating their burnout.
Another critical mechanism is the impairment of autophagy. Autophagy is the cellular “housekeeping” process that cleans out damaged proteins and organelles. In diabetes, this cleaning mechanism becomes sluggish, leading to the accumulation of cellular debris that impairs function. Regenerative therapies aim to reactivate autophagy, enabling cells to detoxify and rejuvenate. By viewing diabetes through the lens of these fundamental cellular processes, medical science moves closer to addressing the root causes of the dysfunction rather than simply masking the symptoms.
The traditional classification of diabetes into distinct “Type 1” and “Type 2” categories is becoming increasingly fluid in the era of regenerative medicine. Clinicians now recognize a spectrum of metabolic disorders that often overlap. For instance, “Latent Autoimmune Diabetes in Adults” (LADA) shares features of both types, involving a slow-burning autoimmune attack on the background of insulin resistance. Similarly, “Double Diabetes” occurs when a Type 1 patient develops the insulin resistance typical of Type 2 due to weight gain and aging.
This nuanced understanding allows for more precise definitions and targeted treatments. A patient is not simply categorized by a number but is profiled based on their specific “immunometabolic” phenotype. This profiling considers genetic predispositions, the status of their beta-cell reserve, systemic inflammation levels, and regenerative potential. This high-definition view of the disease is essential for the application of personalized regenerative therapies, which must be tailored to the specific biological hurdles present in each individual.
Finally, the overview of diabetes must situate the condition within the broader context of Metabolic Syndrome. This syndrome is a cluster of conditions—increased blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels—that occur together, increasing the risk of heart disease, stroke, and diabetes. Regenerative medicine views Metabolic Syndrome as a singular, unified physiological breakdown. It is the external manifestation of a system in distress.
Treating diabetes in isolation without addressing the lipid profile, vascular health, or inflammatory status is considered an incomplete approach. The definition of success in regenerative care involves normalizing the entire metabolic profile. This requires a strategy that integrates cellular therapies with lifestyle modifications designed to alter gene expression (epigenetics). By signaling the body to shift from a storage-and-inflammation mode to a repair-and-regeneration mode, clinicians aim to reverse the tide of metabolic syndrome. This comprehensive definition underscores the interconnectedness of all physiological systems and the necessity of a holistic, biologically grounded approach to care.
Send us all your questions or requests, and our expert team will assist you.
The traditional view primarily focuses on managing blood glucose levels through medication and insulin replacement. The regenerative view defines diabetes as a failure of cellular repair and signaling, focusing on restoring the function of pancreatic beta cells, modulating the immune system, and addressing the root causes of insulin resistance to achieve biological restoration.
Inflammaging is the chronic, low-grade inflammation that naturally increases with age. In the context of diabetes, systemic inflammation disrupts insulin signaling pathways in muscle and liver. It creates a toxic environment for pancreatic cells, directly contributing to the development of hyperglycemia and metabolic dysregulation in older people.
The pancreatic ecosystem is the complex microenvironment where insulin-producing beta cells reside, surrounded by immune cells, blood vessels, and supportive tissue. Regenerative medicine recognizes that diabetes damages this entire environment, not just the beta cells. Effective treatment requires repairing this niche to ensure that cells can survive, sense glucose, and function correctly.
Skeletal muscle is the primary site where the body absorbs and uses glucose. In older adults, the age-related loss of muscle mass (sarcopenia) significantly reduces the body’s ability to clear glucose from the bloodstream. Therefore, preserving muscle health is defined as a core component of diabetes management to maintain metabolic balance.
While the underlying causes differ (autoimmune attack vs. metabolic stress), regenerative medicine views both as conditions of beta-cell loss and dysfunction. The therapeutic goals are similar: to protect remaining cells, stop the underlying damage (immune or metabolic), and stimulate the regeneration or restoration of insulin-producing tissue.


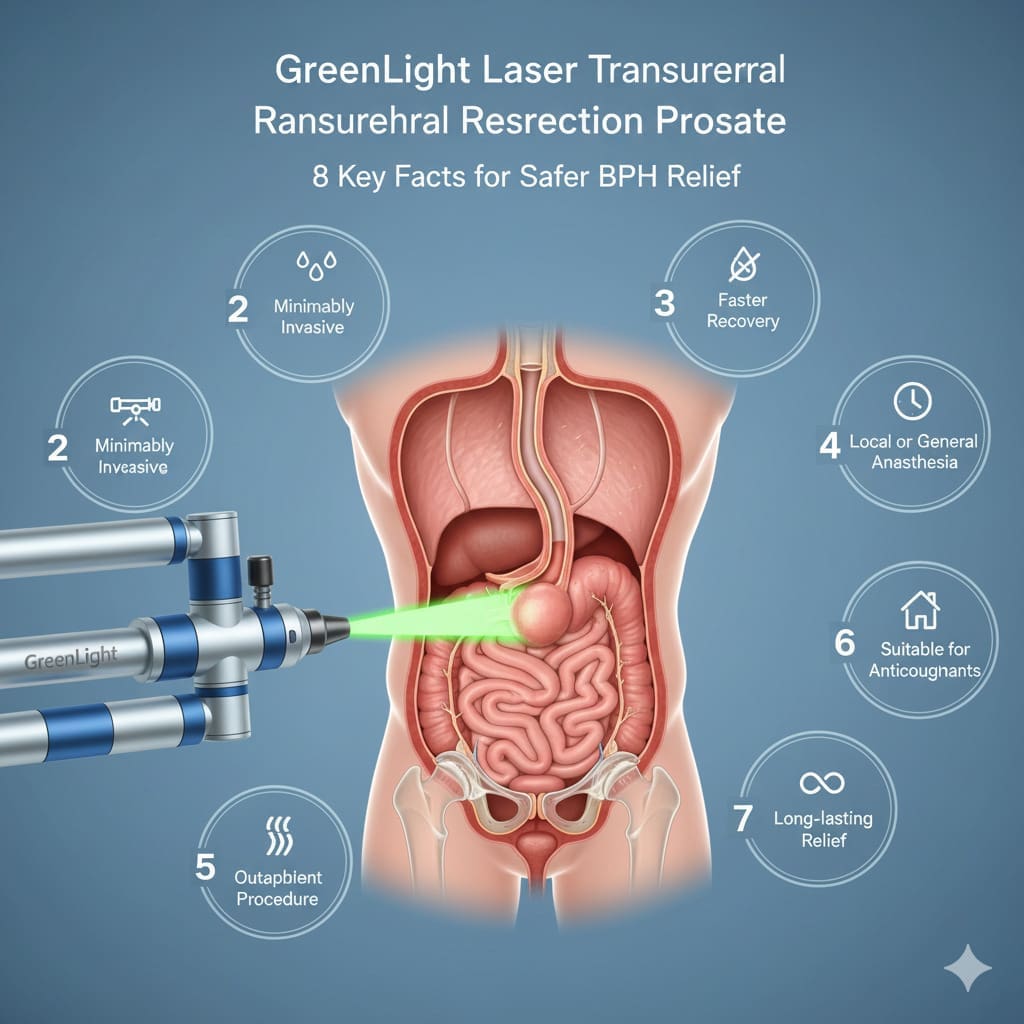
Transurethral resection of the prostate (TURP) is a minimally invasive procedure. It treats benign prostatic hyperplasia by removing excess prostate tissue. This tissue blocks the urinary
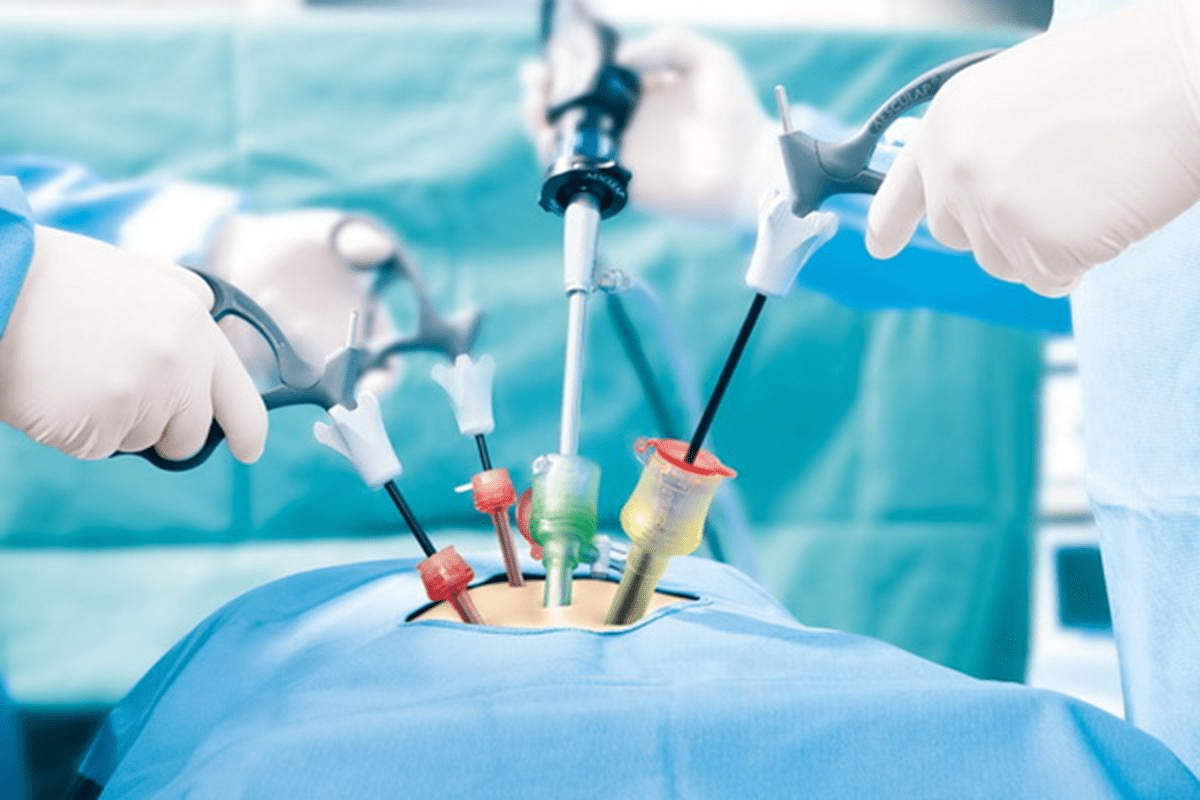
Having TURP surgery is a big step towards better urinary health. But the journey doesn’t stop there. Recovery is key and needs careful planning, patience, and

Recovering from a big surgery is tough. Knowing what to expect helps a lot. What happens after bladder and prostate removal (radical cystoprostatectomy)? Learn about

Transurethral resection of the prostate (TURP) is a common treatment for BPH. This condition makes it hard to urinate because the prostate is too big.

For men with urinary problems due to an enlarged prostate, TURP could change their life. TURP, or Transurethral Resection of the Prostate, is a surgery that

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)