Geriatrics addresses the health needs of older adults, focusing on frailty, dementia, falls, and chronic disease management.
Send us all your questions or requests, and our expert team will assist you.
Diagnosing depression in regenerative medicine and geriatrics is very different from standard psychiatric methods. It uses detailed, data-based tests to find the unique biological causes of each patient’s condition. Instead of just using questionnaires, doctors look closely at the patient’s cells, genes, and body systems to find out what is causing brain problems. This careful approach checks every part of the patient’s health and moves diagnosis from just observing symptoms to using real biological evidence. This change is important because it allows for treatments that are tailored to each person’s needs.
Precision is key in this field. The goal is to find out exactly why each person has depression. Is it due to a problem with how their body processes certain chemicals, hidden blood vessel disease, or an imbalance in gut bacteria? Specialists use thorough testing to answer these questions, instead of using a one-size-fits-all approach. This detailed diagnosis helps patients understand their symptoms and see depression as a problem that can be solved, not just a label.
The cornerstone of this modern evaluation is advanced neuroimaging and functional brain mapping. Techniques such as quantitative Electroencephalography are used to visualize the brain’s electrical activity in real time. This technology allows clinicians to identify specific dysregulated networks, such as hypoactivity in the left prefrontal cortex, which is often associated with positive mood and executive control, or hyperactivity in the deep limbic structures, which drives fear and anxiety. Functional Magnetic Resonance Imaging may also be used to observe blood flow and oxygen use, pinpointing areas that are underactive or “offline.”
By observing the connectome—the intricate map of neural connections—specialists can pinpoint the exact areas where neuroplasticity has stalled or where communication between brain regions has degraded. This descriptive visual data provides a concrete baseline against which the success of regenerative therapies can be measured. It offers patients a transparent, tangible view of their neurological status, allowing them to see the physical reality of their condition and track improvements as their brain heals.

Beyond imaging, the evaluation delves into the molecular realm with comprehensive biomarker panels. Blood, urine, and saliva are analyzed to assess a vast array of physiological metrics. Key among these is the evaluation of neurotrophic factors, such as Brain-Derived Neurotrophic Factor and Vascular Endothelial Growth Factor. Low levels of these proteins serve as critical indicators of the brain’s reduced capacity for repair and maintenance. Additionally, inflammatory markers such as C-reactive protein, homocysteine, and various interleukins are measured to determine the inflammatory burden on the brain.
This granular analysis allows the clinical team to diagnose inflammaging as a specific biological driver of the patient’s depressive symptoms. It separates biological depression from purely psychosocial causes and guides anti-inflammatory interventions. Furthermore, metabolic profiling is performed to assess insulin resistance, vitamin deficiencies, and mitochondrial markers. This ensures that any metabolic blockades preventing energy production in the brain are identified and addressed.

Genetic and epigenetic testing form another pillar of the diagnostic architecture. Understanding a patient’s genetic predispositions—such as variations in the MTHFR gene, which affects methylation and neurotransmitter synthesis—provides invaluable context regarding their susceptibility to mood disorders and their ability to metabolize medications. However, modern diagnostics go further, examining epigenetic markers that reveal how lifestyle and environment have influenced gene expression. This includes measuring telomere length to assess cellular biological age versus chronological age.
A patient with depression may exhibit accelerated cellular aging, a finding that immediately directs the care pathway toward aggressive anti-aging and regenerative interventions. This genomic insight transforms the diagnosis from a static label into a dynamic understanding of gene-environment interactions. It allows the clinician to see not just the genes the patient was born with, but also how those genes are behaving in real time, offering targets for intervention that can reverse negative epigenetic expression.
The evaluation of the neuro-endocrine system is exhaustive. The Hypothalamic-Pituitary-Adrenal axis, the body’s central stress response system, is assessed through diurnal cortisol testing. This reveals whether the patient is in a state of high-stress dominance or a state of adrenal exhaustion, both of which can manifest as profound depression. Furthermore, a full thyroid panel, sex hormone evaluation, and cardiovascular assessment are conducted. This is because hormonal imbalances and vascular dysfunctions often masquerade as, or exacerbate, mood disorders. In the geriatric population, distinguishing between a primary depressive disorder and a hormonal deficiency is a critical diagnostic step.
The gut-brain connection is evaluated through advanced microbiome analysis. By sequencing the DNA of gut flora, clinicians can identify dysbiosis—an imbalance of beneficial and pathogenic bacteria—that may be producing neurotoxins or failing to produce essential neurotransmitter precursors, such as serotonin. Additionally, testing for intestinal permeability helps identify potential sources of systemic inflammation that cross the blood-brain barrier. This aspect of the diagnosis highlights the philosophy that a healthy mind is dependent on a healthy gut environment.
Key components of the regenerative diagnostic suite include:
Computerized Cognitive Assessment: Precise measurement of executive function, memory, and processing speed to track functional impact.
Send us all your questions or requests, and our expert team will assist you.
The connectome is the comprehensive map of neural connections in the brain. In diagnosis, analyzing the connectome helps clinicians identify specific circuits that are disrupted or disconnected. This reveals where communication between brain regions has failed, allowing for targeted treatments to repair these pathways.
Epigenetic testing examines how environmental and lifestyle factors have modified gene expression without altering the DNA itself. It can reveal whether a patient’s genes for stress resilience or inflammation are being inappropriately switched on or off, providing a target for interventions to reverse these adverse effects.
The HPA axis controls the body’s stress response and cortisol production. Chronic depression often involves a dysregulated HPA axis, leading to toxic levels of cortisol that damage brain tissue. Assessing this helps determine if the depression is driven by a broken stress-response system, requiring therapies to re-regulate hormonal balance.
Microbiome analysis reveals the balance of gut bacteria. Since gut bacteria produce many neurotransmitters and regulate inflammation, an imbalance can directly cause or worsen depression. This test identifies if the gut is the source of the neurochemical deficit, guiding probiotic and dietary interventions.
Depression can accelerate cellular aging. Measuring biological age through markers such as telomere length reveals the extent of wear and tear the body has sustained. If a patient’s biological age exceeds their chronological age, it indicates a need for aggressive regenerative therapies to slow senescence and restore cellular vitality and mood.


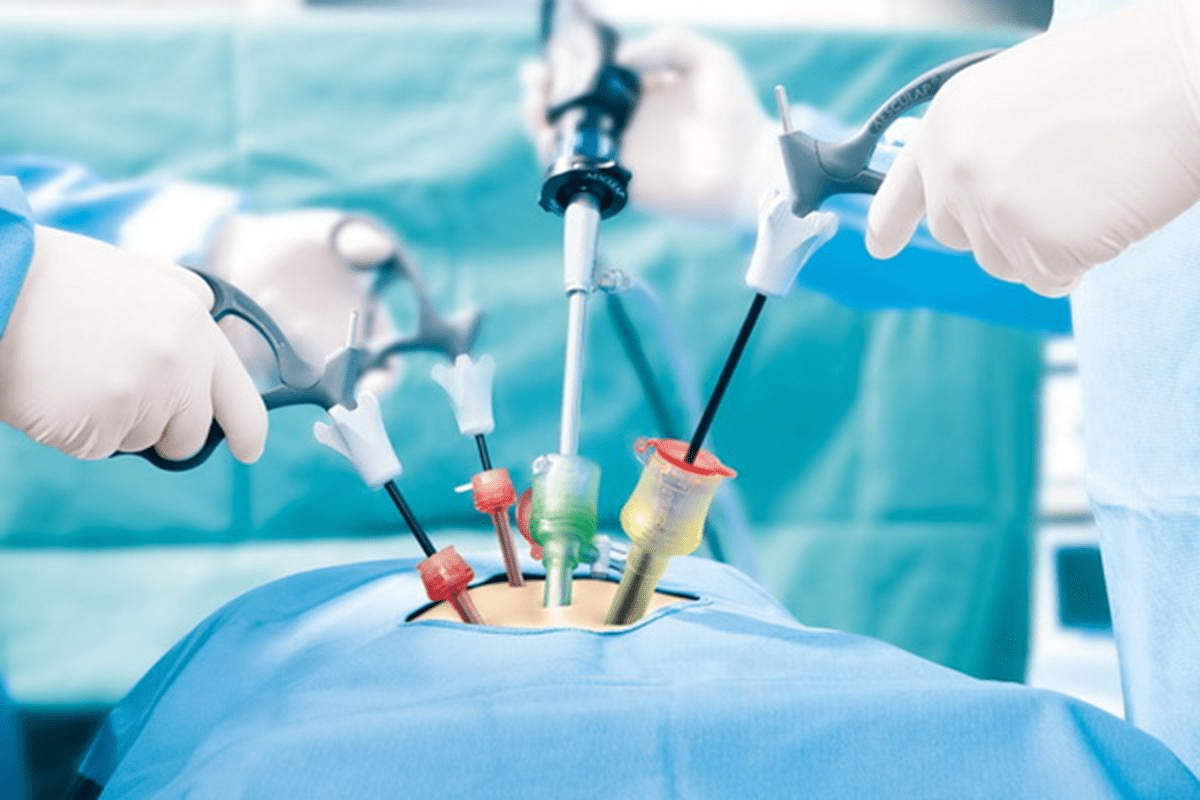
Men often worry that an enlarged prostate means they’re losing their vitality. But, modern TURP surgery brings good news: it’s very safe.At Liv Hospital, we use
Transurethral resection of the prostate, or TURP, is a surgery for bladder issues. At Liv Hospital, we focus on your care and follow the best

Transurethral resection of the prostate (TURP) is a minimally invasive procedure. It treats benign prostatic hyperplasia by removing excess prostate tissue. This tissue blocks the urinary

Recovering from a big surgery is tough. Knowing what to expect helps a lot. What happens after bladder and prostate removal (radical cystoprostatectomy)? Learn about

Robotic prostate surgery is a common choice for treating prostate cancer. It’s important for patients to understand the costs and what their insurance will cover.
Having TURP surgery is a big step towards better urinary health. But the journey doesn’t stop there. Recovery is key and needs careful planning, patience, and

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)