Geriatrics addresses the health needs of older adults, focusing on frailty, dementia, falls, and chronic disease management.
Send us all your questions or requests, and our expert team will assist you.
Diagnosing diabetes in regenerative medicine and geriatrics goes beyond just checking fasting glucose and HbA1c. While these tests are still necessary, they only show past blood sugar control. Newer approaches use detailed, proactive assessments to understand the patient’s current biology. The aim is to build a complete picture of what is causing the disease, how well the pancreas still works, and how much stress the body’s cells are under. This helps doctors choose treatments that fit each person’s unique needs.
In the geriatric context, evaluation is further nuanced by the need to distinguish between age-related physiological changes and pathological disease progression. A “normal” A1c in a frailer older adult might differ from that of a younger individual, to avoid the risks of hypoglycemia. Therefore, the diagnostic framework is dynamic, prioritizing functional capacity and quality of life alongside glycemic targets. The evaluation is not a single event but a continuous biological audit of the body’s regenerative potential.
Central to the regenerative evaluation is the assessment of beta-cell reserve—the pancreas’s remaining capacity to produce insulin. Standard tests often fail to capture the subtle early decline in beta-cell function. Advanced diagnostics utilize C-peptide testing (a byproduct of insulin production) in both fasting and stimulated states. A “C-peptide response test” provides a dynamic measure of the pancreas’s response to a glucose challenge. This is critical for determining whether a patient requires insulin replacement or if their beta cells can be “rescued” and rejuvenated through regenerative therapies.
Furthermore, testing for islet cell autoantibodies is extensive, not just in Type 1 but in adult-onset cases. Identifying latent autoimmune activity (LADA) in older adults is crucial because it changes the treatment trajectory from insulin sensitization to immune modulation. Understanding the specific nature of beta-cell stress—whether autoimmune, oxidative, or endoplasmic reticulum—guides the selection of targeted biological interventions.

Regenerative medicine places immense value on “glycemic variability”—the swings between high and low blood sugar—rather than just the average (A1c). High variability is known to trigger greater oxidative stress and vascular damage than stable, slightly elevated glucose levels. Continuous Glucose Monitoring (CGM) technology is indispensable in this evaluation. It provides a movie rather than a snapshot of glucose levels, revealing patterns of “dawn phenomenon” (morning spikes) or post-prandial surges that standard labs miss.
Time-in-Range (TIR) has emerged as a superior metric for evaluation. It measures the percentage of time a patient spends within a physiological glucose range. Increasing TIR is directly correlated with better regenerative outcomes and reduced microvascular complications. In geriatric patients, identifying asymptomatic hypoglycemia (low blood sugar) is vital, as these events can trigger arrhythmias, falls, and cognitive confusion. The evaluation prioritizes a “flat and stable” glucose profile to create a safe environment for cellular repair.

Since inflammation is a core driver of diabetic pathology, the diagnostic suite includes a deep dive into the inflammatory cascade. High-sensitivity C-reactive protein (hs-CRP) serves as a baseline marker of systemic inflammation. However, more specific markers such as Interleukin-6 (IL-6), Tumor Necrosis Factor-alpha (TNF-α), and fibrinogen are evaluated to assess the “inflammatory load” on the endothelium. Elevated levels of these cytokines signal an active destruction of the vascular niche and insulin receptors.
Oxidative stress profiling involves measuring markers such as F2-isoprostanes and oxidized LDL. These tests reveal the extent of free radical damage to cell membranes and lipids. Evaluating the body’s antioxidant reserve (e.g., Glutathione levels) helps clinicians understand the patient’s capacity to neutralize toxic metabolic byproducts. If the antioxidant defense is depleted, regenerative therapies must include strategies to replenish this biological shield before cell therapies can be effective.
Given that diabetes is fundamentally a vascular disease, evaluating endothelial health is paramount. Non-invasive tests such as Pulse Wave Velocity (PWV) and Carotid Intima-Media Thickness (CIMT) ultrasound measure arterial stiffness and age. These tests detect “subclinical atherosclerosis” years before a cardiac event occurs. Ankle-Brachial Index (ABI) testing is routine for assessing peripheral blood flow to the legs, critical for preventing ulcers and amputations.
In the microcirculation, advanced retinal imaging serves as a systemic barometer. Additionally, tests for microalbuminuria (small amounts of protein in urine) are conducted with high sensitivity to detect the earliest signs of endothelial leakage in the kidneys. This vascular audit enables the medical team to stage the patient’s vascular age and implement regenerative angiogenesis therapies when blood flow is compromised.
In geriatrics, the scale (weight) is a poor indicator of metabolic health. The evaluation focuses on body composition analysis, specifically looking for “sarcopenic obesity”—the combination of low muscle mass and high visceral fat. This phenotype is highly insulin-resistant and inflammatory. Dual-energy X-ray Absorptiometry (DEXA) scans or bioelectrical impedance analysis are used to quantify muscle mass and fat distribution.
Functional testing, such as grip strength and gait speed, provides insight into the metabolic quality of the muscle. Weakness is a direct clinical sign of mitochondrial dysfunction and poor glucose utilization. By quantifying sarcopenia, clinicians can tailor exercise and nutritional prescriptions to restore the skeletal muscle’s “glucose sink” capacity, which is essential for long-term metabolic control.
Recognizing the link between diabetes and cognitive decline, a baseline neuro-cognitive assessment is standard. Tools such as the Montreal Cognitive Assessment (MoCA) help detect early executive dysfunction that may impair a patient’s ability to manage complex treatment regimens.
Autonomic function testing is also critical but often overlooked. Tests for heart rate variability (HRV) during deep breathing or position changes can diagnose cardiac autonomic neuropathy. This condition puts the patient at risk for sudden cardiac death and silent ischemia. Identifying autonomic dysfunction early allows for interventions that stabilize the nervous system and protect the heart.
Send us all your questions or requests, and our expert team will assist you.
C-peptide is a byproduct of insulin production. Unlike insulin, which is cleared quickly from the blood and can be confounded by injected insulin, C-peptide stays in the bloodstream longer and provides a stable, accurate measure of how much insulin the body is making on its own. It is the gold standard for assessing “beta-cell reserve.”
Glycemic variability refers to the rollercoaster of blood sugar spikes and crashes. These rapid fluctuations cause massive oxidative stress and damage to the lining of blood vessels, much more so than a stable but slightly elevated sugar level. This “shaking” of the metabolic system accelerates complications like retinopathy and heart disease.
Sarcopenic obesity is a condition common in older adults where they have “normal” weight but very low muscle mass and high hidden fat (visceral fat) around the organs. It is diagnosed using body composition scans (like DEXA). This condition is dangerous because the lack of muscle removes the body’s main way to burn sugar, while the fat drives inflammation.
Yes. Standard blood tests (creatinine) often don’t show kidney problems until significant function is lost. The test for “microalbuminuria” detects microscopic amounts of protein leaking into the urine, which is the very first sign that the kidney’s filtration barrier is damaged, allowing for much earlier intervention.
HRV measures the tiny variations in time between heartbeats. A high variation is healthy, indicating a responsive nervous system. In diabetes, nerves controlling the heart get damaged (autonomic neuropathy), leading to low HRV. Measuring this helps predict cardiac risk and “silent” heart issues that otherwise have no symptoms.


Transurethral resection of the prostate (TURP) is a minimally invasive procedure. It treats benign prostatic hyperplasia by removing excess prostate tissue. This tissue blocks the urinary
Transurethral resection of the prostate, or TURP, is a surgery for bladder issues. At Liv Hospital, we focus on your care and follow the best

For men with urinary problems due to an enlarged prostate, TURP could change their life. TURP, or Transurethral Resection of the Prostate, is a surgery that

Robotic prostate surgery is a common choice for treating prostate cancer. It’s important for patients to understand the costs and what their insurance will cover.
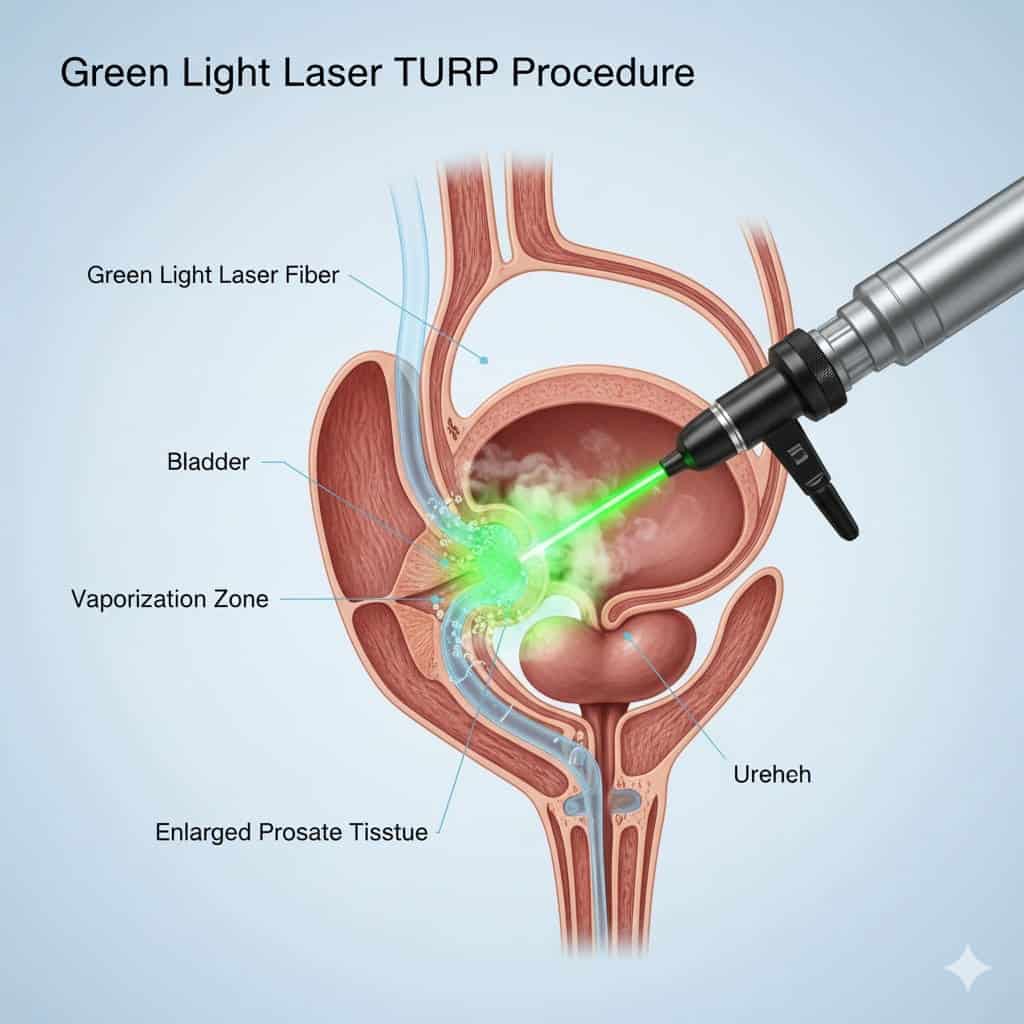
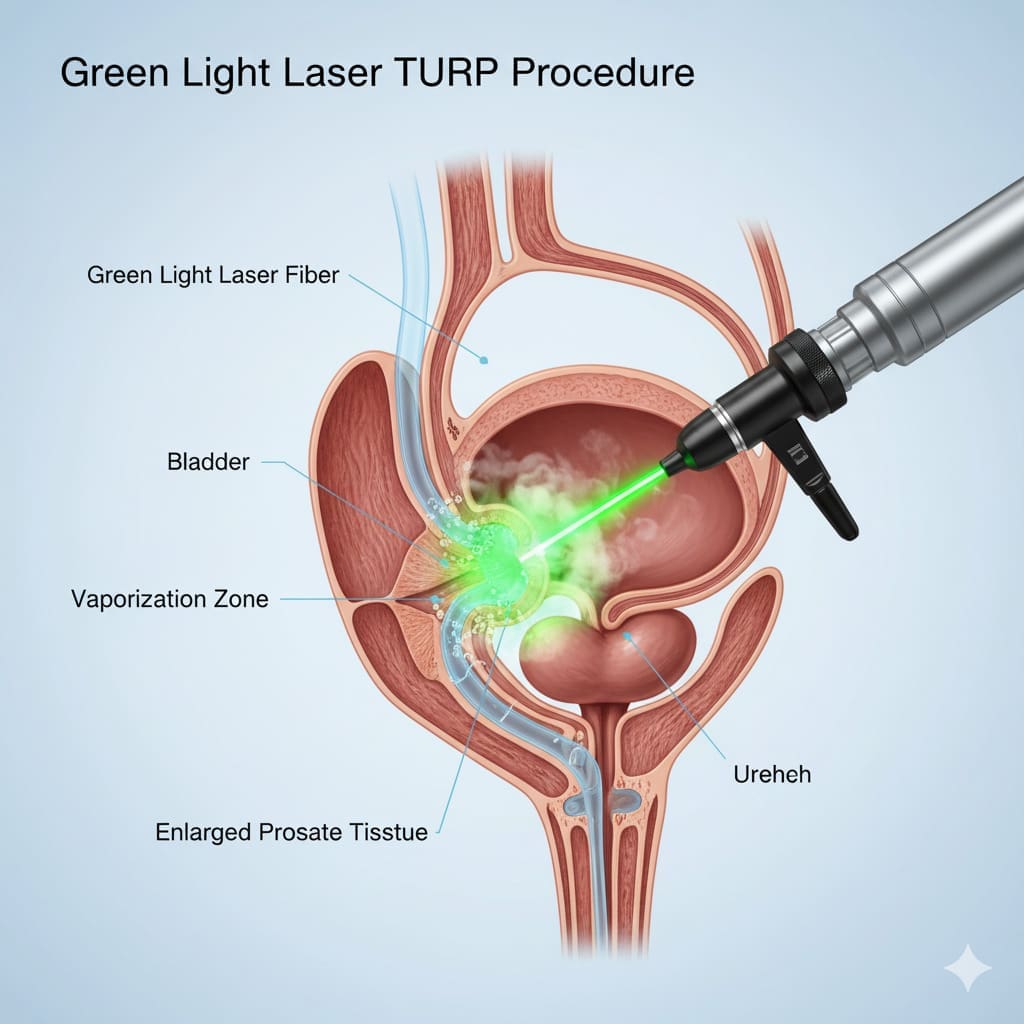
Men with enlarged prostate symptoms need to pick the right treatment. Understanding modern treatments like the Green Light Laser Transurethral Resection of Prostate is key.Studies

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)