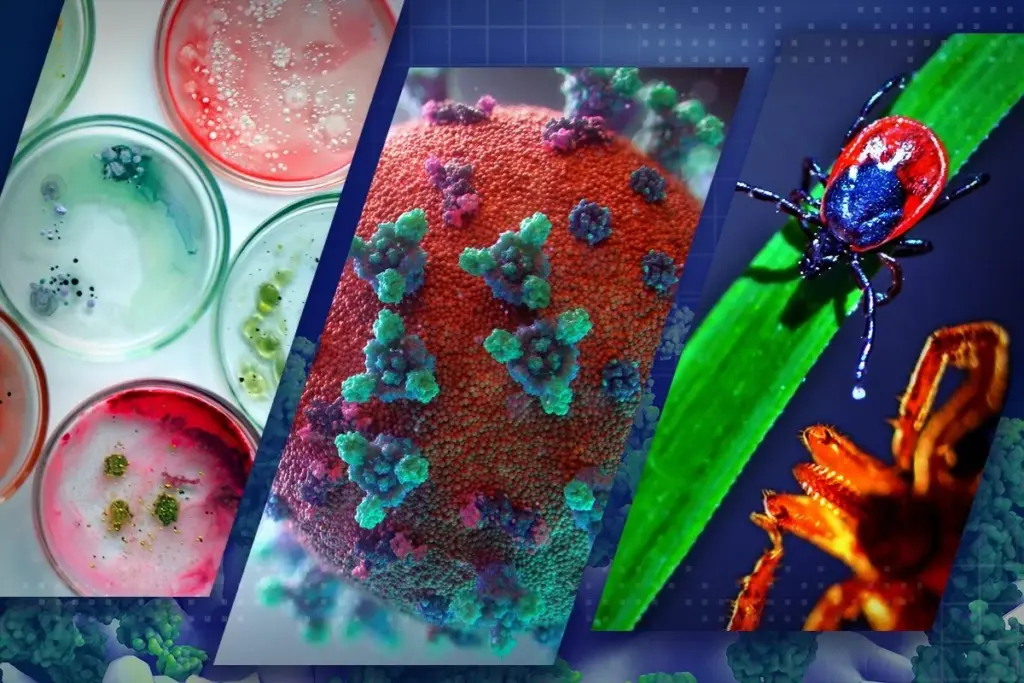
Infectious diseases specialists diagnose and treat infections from bacteria, viruses, fungi, and parasites, focusing on fevers, antibiotics, and vaccines.
Send us all your questions or requests, and our expert team will assist you.

The clinical manifestation of food poisoning is rarely immediate, a fact that often leads to misidentification of the culprit meal. The time between the ingestion of the contaminated item and the onset of the first symptom is known as the incubation period. The pathogen type and the disease mechanism biologically determine this window. For toxins, such as those produced by Staphylococcus aureus in unrefrigerated cream pastries, the onset can be rapid and explosive, occurring within 1 to 6 hours. This is because the biological weapon is pre-formed; the body reacts immediately to the chemical assault.
In contrast, biological pathogens that require colonization take much longer to announce their presence. Bacterial infections such as Salmonella or Campylobacter typically have incubation periods of 12 hours to 5 days. During this time, the bacteria must survive the stomach acid, navigate the small intestine, adhere to the mucosal wall, and multiply to sufficient numbers to trigger an immune response. Parasitic infections may take weeks to manifest. This variability makes it fundamentally flawed to rely on the “last meal hypothesis”—the belief that the last thing eaten caused the illness. The actual source is often a meal consumed days prior.

The hallmark presentation of food poisoning is acute gastroenteritis, an inflammation of the lining of the stomach and intestines. The body’s physiological response to this invasion is to expel it. The mechanisms are defensive, designed to purge the toxin or pathogen from the system.

While the gut is the primary battlefield, the effects of food poisoning often become systemic. The release of pyrogens (fever-inducing substances) by the immune system leads to febrile states, chills, and rigors. Dehydration, a direct consequence of fluid loss, manifests systemically as tachycardia (rapid heart rate), hypotension (low blood pressure), dry mucous membranes, and lethargy.
Specific pathogens have a predilection for tissues beyond the gut. Listeria monocytogenes, for example, can cross the intestinal barrier and enter the bloodstream, causing sepsis, or cross the blood-brain barrier to cause meningitis, presenting with stiff neck, confusion, and photophobia. This invasive capability is particularly dangerous for pregnant women, as the bacteria can target the fetus. Similarly, the neurotoxin of Clostridium botulinum (botulism) causes descending paralysis, starting with blurred vision and drooping eyelids before affecting the muscles of respiration. In these cases, the gastrointestinal symptoms may be mild or absent, masked by the profound neurological compromise.
The transmission of foodborne pathogens is almost exclusively governed by the “fecal-oral route.” This clinical term describes the cycle in which pathogens excreted in the stool of an infected host (human or animal) eventually enter the mouth of a susceptible host. Food serves as the vehicle for this transfer.

The host’s immunological status heavily influences symptom severity and transmission ease. Specific demographics are considered high-risk populations.

While distinct from solid food, water is a critical vector for “food” poisoning. Contaminated water used for drinking, washing produce, or reconstituting powdered foods acts as a direct delivery system for pathogens. Cryptosporidium and Giardia are parasites famously resilient to standard chlorine disinfection and can be transmitted through municipal water supplies or recreational water. In many parts of the world, the distinction between foodborne and waterborne illness is blurred, as water is an ingredient in nearly all food preparation.
Send us all your questions or requests, and our expert team will assist you.
Severe dehydration is a medical emergency. Signs include extreme thirst, dry mouth and skin, little or no urination, dark yellow urine, dizziness, confusion, rapid heartbeat, and sunken eyes. In infants, a sunken soft spot (fontanelle) on the head and crying without tears are critical warning signs.
Bloody diarrhea, or dysentery, is a specific and severe symptom often associated with invasive bacterial infections like E. coli O157:H7, Shigella, or Campylobacter. It indicates that the bacteria are damaging the intestinal lining. It is not common in viral food poisoning and warrants immediate medical attention.
This depends on the pathogen. For Norovirus, a person can remain contagious for two weeks or more after they feel better. For Salmonella, bacteria can be shed in the stool for several weeks to months. This is why strict hand hygiene is essential even after recovery, especially for food handlers.
Yes. If cooked food is left at room temperature for more than two hours, bacteria can multiply to dangerous levels. Reheating may kill bacteria, but it might not destroy heat-stable toxins produced by bacteria like Bacillus cereus (often found in rice) or Staphylococcus aureus, which can cause illness.
No. Fever is a sign of an inflammatory or invasive infection (like Salmonella or Listeria). Many forms of food poisoning, particularly those caused by toxins (such as Staphylococcus) or viruses, may present with vomiting and diarrhea but no significant fever. The absence of fever does not rule out foodborne illness.


Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)