Last Updated on November 26, 2025 by Bilal Hasdemir
Ovarian cancer is often called a “silent killer” because its symptoms are frequently mistaken for other less serious conditions. The American Cancer Society states it’s the fifth leading cause of cancer deaths among women in the United States. A key question is whether a doctor can detect ovarian cancer through a physical examination.
While a doctor may feel abnormalities during a pelvic exam, detecting ovarian cancer by touch alone is challenging. Early detection is critical, as survival rates improve when the disease is caught early. It’s essential to understand the role of physical examination in ovarian cancer screening for women’s health.
Key Takeaways
- Ovarian cancer is often misdiagnosed due to its non-specific symptoms.
- A doctor may be able to feel abnormalities during a pelvic exam.
- Early detection of ovarian cancer significantly improves survival rates.
- Physical examination is one aspect of ovarian cancer screening.
- Understanding the limitations of detection methods is crucial.
The Silent Nature of Ovarian Cancer
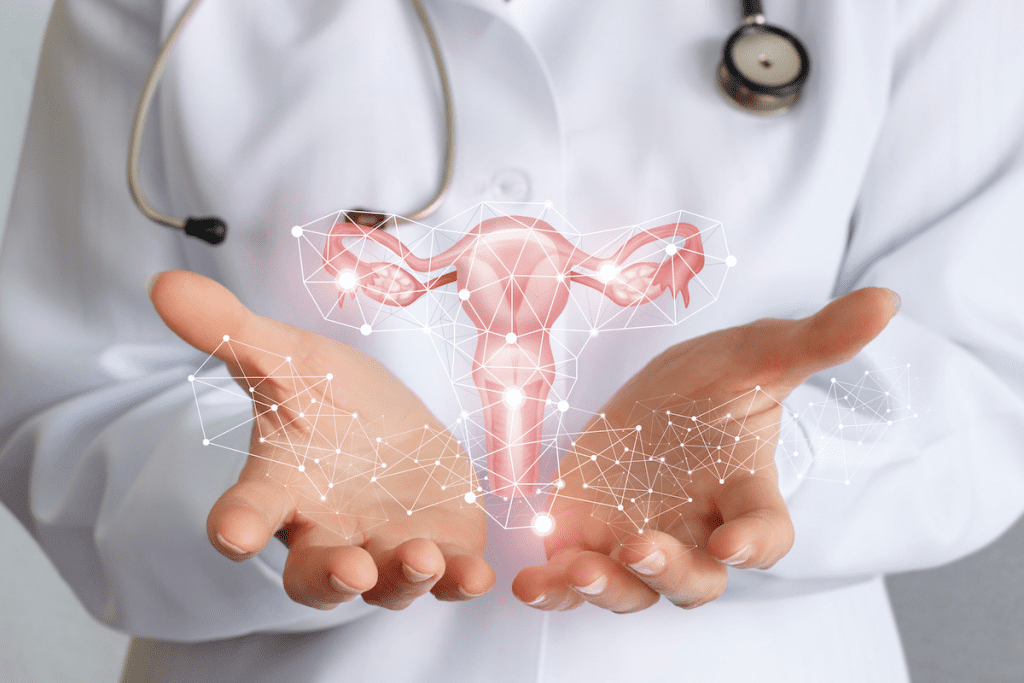
Ovarian cancer poses a significant challenge due to its elusive nature in early detection. It affects the ovaries, vital organs for egg production in females. This cancer type grows uncontrollably, making it a serious concern.
What defines ovarian cancer
Ovarian cancer is marked by the abnormal growth of cells in the ovaries. It encompasses several types, with epithelial ovarian cancer being the most prevalent, accounting for about 90% of cases. This highlights the need for targeted awareness and research.
Current statistics in the United States
In the United States, ovarian cancer is a pressing health issue. The American Cancer Society reports 19,680 new cases in 2022, leading to 12,740 deaths. These numbers underscore the urgency for early detection and prevention.
The challenge of early detection
Early detection is key to treating ovarian cancer effectively. Yet, symptoms are often vague and similar to other common conditions. The absence of a reliable screening test exacerbates this challenge.
| Category | Statistic | Challenge |
| New Cases (2022) | 19,680 | Lack of awareness |
| Deaths (2022) | 12,740 | Late-stage diagnosis |
| Common Type | Epithelial ovarian cancer (90%) | Difficulty in diagnosis |
Grasping the nature, prevalence, and detection hurdles of ovarian cancer is vital. It’s a step towards enhancing patient outcomes and survival rates.
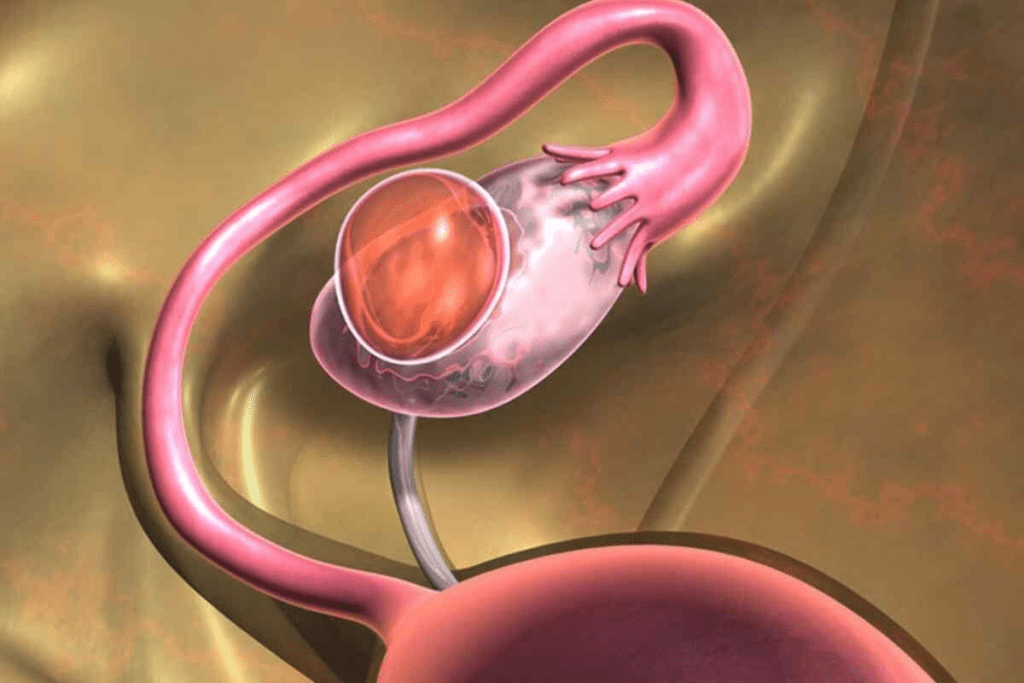
Ovarian Anatomy: Why Location Matters for Detection
The location of the ovaries in the pelvis greatly affects their detectability during a clinical exam. It’s crucial for healthcare providers to grasp the normal anatomy of the ovaries to assess their condition accurately.
Normal Ovarian Position in the Pelvis
The ovaries sit on either side of the uterus, nestled in the pelvic cavity. They are anchored by several ligaments, allowing for some movement. This positioning can sometimes complicate the detection of abnormalities through physical examination alone.
Typically, the ovaries resemble an almond in size. Their small stature, combined with their deep pelvic location, poses challenges for detection through palpation. A deep understanding of pelvic anatomy is essential for gynecologists to overcome these hurdles.
Size and Accessibility Challenges
The size and accessibility of the ovaries during a pelvic exam are key factors in detecting ovarian cancer. Early-stage ovarian cancer may not cause the ovary to enlarge significantly, making detection through touch more difficult.
| Ovarian Size | Detectability | Clinical Implication |
| Normal (almond size) | Difficult to detect abnormalities | Requires skilled examination |
| Enlarged (due to cancer or cysts) | Easier to detect through palpation | May indicate need for further investigation |
A study on ovarian cancer detection underscores the challenge. “The challenge lies not only in the size but also in the location of the ovaries, which can be deep within the pelvis.”
(This anatomical complexity necessitates a skilled and experienced examiner to accurately assess ovarian health.)
In conclusion, grasping ovarian anatomy and the challenges of pelvic exams is crucial for effective detection and diagnosis of ovarian cancer. Healthcare providers must be aware of these factors to deliver the best care possible.
Detecting Ovarian Cancer by Touch: The Clinical Process
The process of detecting ovarian cancer through touch involves a bimanual pelvic examination. This method requires precision and skill. It’s a key part of a routine gynecological check-up, aimed at assessing the health of female reproductive organs.
The Bimanual Pelvic Examination Technique
In a bimanual pelvic exam, the healthcare provider uses one hand to examine the pelvic organs through the vagina. The other hand is placed on the abdomen. This allows for a detailed assessment of the ovaries and surrounding tissues.
The examiner inserts one or two gloved, lubricated fingers into the vagina while pressing on the abdomen. This method enables the doctor to feel the ovaries and detect any abnormalities, such as masses or irregularities.
What Abnormalities Doctors Search For
Gynecologists are trained to identify various abnormalities during a bimanual pelvic examination. When checking for ovarian cancer, they look for signs such as:
- Unusual masses or lumps
- Irregularities in the shape or size of the ovaries
- Abnormal tenderness or pain
- Fixation or immobility of the ovaries
These findings can indicate the presence of ovarian cancer or other conditions that may require further evaluation.
Specialized Training for Gynecologists
Gynecologists undergo extensive training to develop the skills necessary for performing a bimanual pelvic examination effectively. This training includes:
- Anatomical knowledge of the female reproductive system
- Hands-on practice in performing pelvic examinations
- Understanding of various pathological conditions, including ovarian cancer
By combining theoretical knowledge with practical experience, gynecologists can accurately assess the health of their patients’ reproductive organs and detect potential issues early.
What Happens During a Pelvic Examination
The pelvic examination is a key part of gynecological care, aimed at checking the health of reproductive organs. It’s vital for spotting any issues or abnormalities early on.
Step-by-Step Procedure Explanation
The healthcare provider follows a detailed sequence during a pelvic examination. It starts with an external check, then uses a speculum to open the vaginal canal. This allows a visual inspection of the cervix and vagina.
Next, a bimanual examination is performed. This involves using gloved fingers to feel the reproductive organs internally while pressing on the abdomen from the outside. This method helps assess the size, shape, and consistency of the uterus and ovaries, looking for any abnormalities or tenderness.
Patient Positioning and Comfort Measures
Comfort is a top priority during a pelvic examination. Patients lie on an examination table in a supine position, with their feet in stirrups. This setup makes the procedure easier. Healthcare providers often explain each step to reduce anxiety and ensure cooperation.
To make patients more comfortable, they are advised to relax and breathe deeply. Some facilities offer extra comfort measures, like draping or having a chaperone present.
Recommended Frequency for Different Age Groups
The frequency of pelvic examinations varies by age, health status, and risk factors. The American College of Obstetricians and Gynecologists suggests starting regular pelvic exams at age 21. Women under 30 who are not sexually active might have them less often, every 1-3 years, based on their health needs.
For women over 30 or those with certain health issues, more frequent exams are recommended. It’s crucial for women to talk to their healthcare provider to find out the best schedule for their health.
Can a Gynecologist Actually Feel Ovarian Cancer?
The success of ovarian cancer detection through manual examination by gynecologists depends on various factors. Manual examination is a key tool for detecting gynecological conditions. However, its effectiveness in identifying ovarian cancer is influenced by several factors.
Detection Success Rates Through Manual Examination
Research indicates that the success rate of detecting ovarian cancer through manual examination varies. Studies suggest that the sensitivity of pelvic examinations in detecting ovarian cancer can range from 20% to 50% in early-stage disease. This rate improves somewhat in more advanced stages.
| Stage of Ovarian Cancer | Detection Rate |
| Early Stage | 20-50% |
| Advanced Stage | Higher than early stage, exact rates vary |
Factors That Improve Detection Probability
Several factors can enhance the likelihood of detecting ovarian cancer during a manual examination. These include:
- Specialized training: Gynecologists with specialized training in gynecologic oncology are more likely to detect abnormalities.
- Patient factors: Patient characteristics, such as menopausal status and body mass index (BMI), can influence the ease of detection.
- Size and location of the tumor: Larger tumors or those located in more accessible areas are more likely to be detected manually.
Understanding these factors is crucial for both healthcare providers and patients. While manual examination has its limitations, it remains a vital component of gynecological care.
By combining manual examination with other diagnostic tools and being aware of the factors that influence detection, healthcare providers can improve the chances of identifying ovarian cancer at an early stage.
Physical Limitations of Feeling Ovarian Cancer
Detecting ovarian cancer through touch is challenging due to several physical limitations. These can be broadly categorized into size thresholds, anatomical barriers, and patient-specific challenges.
Size Thresholds: Why Early Cancers Remain Undetectable
Early-stage ovarian cancers are often small and difficult to detect through manual examination. The size of the tumor is a key factor in its detectability. Smaller tumors are harder to feel during a pelvic exam. Research shows that tumors less than 3 cm in diameter are particularly challenging to detect manually.
Anatomical Barriers to Effective Palpation
The anatomy of the female pelvis presents several barriers to effective palpation of the ovaries. The ovaries are located deep within the pelvis, surrounded by other organs and structures. This makes it difficult to isolate and examine them thoroughly. Additionally, factors such as obesity or previous abdominal surgery can further complicate the examination.
Patient-Specific Challenges Affecting Examination
Patient-specific factors, such as muscle tension, pain, or discomfort during the examination, can also impact the effectiveness of manual detection. Some patients may have conditions that make a thorough pelvic examination challenging, such as vaginismus or pelvic adhesions.
Understanding these physical limitations is crucial for both healthcare providers and patients. While manual examination has its limitations, it remains a valuable tool in the initial assessment of ovarian cancer. Healthcare providers must be aware of these challenges to interpret findings accurately and decide on the next steps in diagnosis.
When Large Ovarian Tumors Become Palpable
Ovarian tumors that grow significantly can be felt during a clinical exam. Their detectability is tied to size and stage. As large ovarian tumors expand, they become more palpable during a pelvic exam.
Size and Stage Correlation with Physical Detectability
The size of an ovarian tumor is crucial in determining palpability. Tumors over 5 cm in diameter are more likely to be palpable. Yet, the tumor’s stage also impacts detectability.
Advanced-stage tumors, being larger, are more palpable. The tumor’s location, consistency, and mobility also affect manual detection.
Characteristics of Manually Detectable Masses
Manually detectable ovarian masses exhibit distinct characteristics. They may feel like a lump or swelling in the pelvic area. Their firmness, softness, mobility, and tenderness vary.
Ascites, fluid accumulation in the abdomen, can accompany advanced ovarian cancer. This makes the abdomen feel distended.
What Advanced Disease Typically Feels Like
In advanced ovarian disease, tumors may spread to other pelvic or abdominal areas. This makes exams more complex. The masses may feel irregular, with varying consistency, and may cause pelvic pain or discomfort.
Healthcare providers must recognize these characteristics for accurate assessment and diagnosis of ovarian tumors.
Distinguishing Cancerous vs. Benign Ovarian Findings
Gynecologists use their expertise to tell apart benign from potentially cancerous ovarian masses during exams. This is key for deciding the next steps and easing patient worries.
Ovarian cysts: Common and usually benign
Ovarian cysts are fluid-filled sacs on the ovaries, common in women of childbearing age. Most are benign and may go away without treatment. Yet, some cysts can lead to pelvic pain or discomfort during activities.
Doctors can feel ovarian cysts during a pelvic exam. The cyst’s size, tenderness, and how it moves can hint at its type.
Fibroid tumors and other benign conditions
Fibroid tumors, or uterine leiomyomas, are non-cancerous growths in or around the uterus. Though not ovarian, large fibroids can be mistaken for ovarian masses. Other benign conditions, like endometriomas or dermoid cysts, can also mimic ovarian issues.
Doctors must carefully distinguish these benign conditions from possible cancerous ovarian tumors.
Red flags that suggest malignancy
Certain signs during a pelvic exam can hint at ovarian cancer. These red flags include a fixed or irregular mass, tenderness, or ascites (fluid in the abdomen). Finding these signs means more tests, like imaging and possibly biopsy, are needed.
Spotting ovarian cancer early is crucial for better treatment results. This shows how vital skilled pelvic exams are.
Recognizing Ovarian Cancer Warning Signs
Identifying the early signs of ovarian cancer can greatly improve treatment success. Known as a “silent killer,” ovarian cancer’s symptoms are often subtle. They can be mistaken for less serious conditions.
Subtle Symptoms Often Dismissed
Many women overlook the early signs of ovarian cancer, thinking they’re minor or unrelated. Common symptoms include:
- Pelvic or abdominal pain
- Bloating or swelling in the abdomen
- Difficulty eating or feeling full quickly
- Urinary urgency or frequency
- Fatigue
These symptoms are vague and often linked to common ailments. This makes early diagnosis of ovarian cancer difficult.
When Symptoms Warrant Immediate Medical Attention
If you notice any of these symptoms, it’s vital to see a doctor:
- Severe or persistent pelvic or abdominal pain
- Unexplained weight loss or gain
- Significant changes in bowel or urinary habits
Knowing these warning signs can help catch ovarian cancer early. This is when it’s most treatable.
The Symptom Diary Approach
Using a symptom diary can track your symptoms and spot patterns. Documenting when symptoms happen, how severe they are, and what triggers or relieves them helps your doctor. This information is crucial.
It’s essential to be proactive about your health and discuss your concerns with your doctor without hesitation.
Ovarian Cancer Risk Assessment
Understanding the risk of ovarian cancer involves a deep dive into genetic, environmental, and lifestyle factors. This is key to spotting those at higher risk and taking preventive steps.
Genetic Predisposition: BRCA1/2 and Beyond
Genetic mutations are a major factor in ovarian cancer risk. BRCA1 and BRCA2 mutations significantly up the risk of breast and ovarian cancers. Other genes like BRIP1, RAD51C, and RAD51D also raise the risk.
- BRCA1 and BRCA2 mutation carriers face a higher lifetime risk of ovarian cancer.
- Genetic testing can spot these mutations, paving the way for early intervention.
Family History Significance
A family history of ovarian or breast cancer is a major risk factor. Those with a first-degree relative (mother, sister, or daughter) diagnosed with ovarian cancer are at greater risk.
“A woman with a family history of ovarian cancer should discuss her risk with a healthcare provider to determine the best course of action.”
Lifestyle and Environmental Factors
Lifestyle and environmental factors also impact risk, alongside genetics. These include:
- Age: Risk increases with age, especially after 50.
- Reproductive history: Women who’ve never given birth or have struggled with pregnancy may face higher risks.
- Hormone replacement therapy (HRT): Especially estrogen-alone therapy, has been linked to increased risk.
Risk-Reducing Strategies for High-Risk Women
For those at high risk, several strategies can lower ovarian cancer risk:
- Risk-reducing salpingo-oophorectomy (RRSO): Surgical removal of ovaries and fallopian tubes.
- Surveillance: Regular monitoring with transvaginal ultrasound and CA-125 blood tests.
- Chemoprevention: Oral contraceptives have been shown to reduce risk.
Understanding ovarian cancer risk is complex, involving genetics, environment, and lifestyle. Identifying high-risk individuals and using preventive strategies can help reduce this disease’s incidence.
Emerging Technologies for Earlier Detection
Ovarian cancer detection is on the cusp of a revolution, thanks to emerging technologies. The medical community is witnessing significant advancements in diagnostic tools. These advancements promise to improve early detection rates.
Liquid Biopsy Advancements
Liquid biopsy, a non-invasive diagnostic technique, is showing great promise in detecting ovarian cancer. Recent studies have highlighted its potential in identifying specific biomarkers associated with ovarian cancer. This allows for earlier intervention.
The advantages of liquid biopsy include:
- Minimally invasive, reducing patient discomfort
- Potential for early detection before symptoms appear
- Ability to monitor disease progression and treatment response
Artificial Intelligence in Imaging Interpretation
Artificial intelligence (AI) is being increasingly used to enhance imaging interpretation for ovarian cancer detection. AI algorithms can analyze complex imaging data, such as ultrasounds and MRIs. They identify patterns indicative of cancer.
According to a
“study published in a leading medical journal, AI-powered imaging analysis demonstrated a significant improvement in detection accuracy compared to traditional methods.”
Novel Biomarker Research
Researchers are continually discovering new biomarkers that could aid in the early detection of ovarian cancer. Biomarkers are crucial for developing diagnostic tests. These tests can identify the disease at its earliest stages.
The integration of these emerging technologies into clinical practice holds great promise for improving ovarian cancer outcomes. As research continues to advance, we can expect to see more effective and efficient diagnostic tools.
The Diagnostic Pathway After an Abnormal Finding
When an abnormal finding is detected during a pelvic examination, the next steps are crucial in determining the presence of ovarian cancer. The diagnostic pathway that follows is designed to provide a clear understanding of the abnormality and to guide appropriate treatment.
Immediate Next Steps Following Suspicious Exam
Upon identifying an abnormal finding, the healthcare provider will typically discuss the results with the patient and outline the immediate next steps. As noted by the American Cancer Society, “if the pelvic exam reveals an abnormality, further testing is needed to determine the cause” (American Cancer Society). This may involve additional examinations, imaging tests, or laboratory tests to gather more information about the nature of the abnormality.
The initial response to an abnormal finding is critical and may include a detailed medical history to identify any risk factors or symptoms that could be relevant to the diagnosis. The healthcare provider may also perform a physical examination to check for any other signs that could indicate ovarian cancer.
The Diagnostic Workup Process
The diagnostic workup process for ovarian cancer typically involves a combination of imaging tests and laboratory tests.
- Imaging tests such as ultrasound, CT scans, or MRI scans to visualize the ovaries and assess the extent of any abnormalities.
- Laboratory tests, including blood tests to measure tumor markers like CA-125, which can be elevated in ovarian cancer.
A quote from a medical professional highlights the importance of a thorough diagnostic workup: “A comprehensive diagnostic evaluation is essential to accurately diagnose ovarian cancer and develop an effective treatment plan” (
A comprehensive diagnostic evaluation is essential to accurately diagnose ovarian cancer and develop an effective treatment plan.
).
Timeframe Expectations for Diagnosis
The timeframe for diagnosis can vary depending on the complexity of the case and the tests required. Generally, the diagnostic process can take anywhere from a few days to several weeks. Patients should discuss their specific situation with their healthcare provider to understand what to expect.
Understanding the diagnostic pathway and the timeframe for diagnosis can help alleviate some of the anxiety associated with an abnormal finding. By being informed, patients can better navigate the process and make informed decisions about their care.
Conclusion: The Value and Limitations of Physical Examination
Detecting ovarian cancer through physical examination alone is highly challenging. It heavily relies on the gynecologist’s skill and the tumor’s characteristics. While crucial for screening, physical exams have their limits. The ovaries’ deep location in the pelvis makes detecting abnormalities through touch alone challenging.
The success of detection through touch depends on several factors. These include the tumor’s size and the patient’s anatomy. Larger tumors are easier to detect, but early-stage cancers often evade detection. New technologies, like liquid biopsy and AI in imaging, aim to enhance early detection rates.
A comprehensive approach to diagnosis is key. It combines physical exams, imaging, and symptom assessment for early-stage identification. Women, especially those at high risk, should be vigilant about subtle symptoms and regular screening. Understanding the value and limitations of physical exams helps healthcare providers improve ovarian cancer diagnosis and management, leading to better patient outcomes.
FAQ
Can a doctor feel ovarian cancer during a pelvic exam?
A doctor might feel ovarian cancer during a pelvic exam, but it’s not always possible. This depends on the tumor’s size and location. Early stages can be particularly challenging to detect by touch.
How does a bimanual pelvic examination help in detecting ovarian cancer?
A bimanual pelvic exam involves a healthcare provider feeling the abdomen with one hand and the vagina and cervix with the other. This method allows them to check the ovaries for any irregularities, such as masses or tenderness.
What are the limitations of detecting ovarian cancer through a physical exam?
Physical exams have limitations in detecting ovarian cancer. These include the tumor’s size, location, and the patient’s body type. Small tumors or those deep in the pelvis can be hard or impossible to find manually.
Can ovarian cysts be felt by a doctor during a pelvic exam?
Yes, doctors can often feel ovarian cysts during a pelvic exam. Yet, it’s hard to tell if a cyst is benign or cancerous just by feeling it.
How accurate is a pelvic exam in detecting ovarian cancer?
The accuracy of a pelvic exam in finding ovarian cancer varies. A skilled healthcare provider can spot some cancers, but many early cases are not detectable by physical exam alone.
What are the next steps if a doctor suspects ovarian cancer during a pelvic exam?
If a doctor suspects ovarian cancer, they’ll suggest more tests. This includes imaging studies like ultrasound and CT scans, and possibly a biopsy to confirm the tumor’s nature.
Can ovarian cancer be missed on a pelvic exam?
Yes, ovarian cancer can be missed on a pelvic exam, especially if the tumor is small or hard to feel. Regular check-ups and knowing your risk factors are key to early detection.
How often should women have a pelvic exam to screen for ovarian cancer?
The frequency of pelvic exams for ovarian cancer screening varies. It depends on age, risk factors, and what your healthcare provider advises. Women should talk to their doctor about their individual screening needs.
Are there any risk-reducing strategies for ovarian cancer?
Yes, there are ways to reduce ovarian cancer risk. These include genetic testing for BRCA1 and BRCA2, prophylactic surgery for high-risk individuals, and possibly certain birth control methods.
What emerging technologies are being developed for earlier ovarian cancer detection?
New technologies aim to detect ovarian cancer earlier. These include liquid biopsy, AI in imaging, and biomarker research. They aim to improve detection and catch cancer at an earlier stage.
References
- National Cancer Institute. (2023). Ovarian, fallopian tube, and primary peritoneal cancer screening (PDQ ®)“Health professional version. https://www.cancer.gov/types/ovarian/hp/ovarian-screening-pdq