
Coronary artery disease affects millions worldwide. Angioplasty with stent placement is a common treatment. But, have you ever wondered how long a stent lasts after it’s inserted? Stents life expectancy? They last a lifetime. Get best vital heart facts. The real danger is new plaque. Learn how to stay safe and healthy.
The lifespan of a coronary stent depends on several factors. These include the type of stent, patient health, and lifestyle choices. Recent advancements in stent technology have made them last longer.
Knowing how long a stent lasts is key for patients and healthcare providers. It helps in making better decisions about heart care. We will look into what affects stent longevity and the latest in stent technology.
Key Takeaways
- The lifespan of a coronary stent varies based on several factors.
- Advancements in stent technology have improved durability.
- Patient health and lifestyle choices play a significant role.
- Understanding stent longevity is key for heart care.
- Different types of stents have different life expectancies.
Understanding Stents and Their Purpose
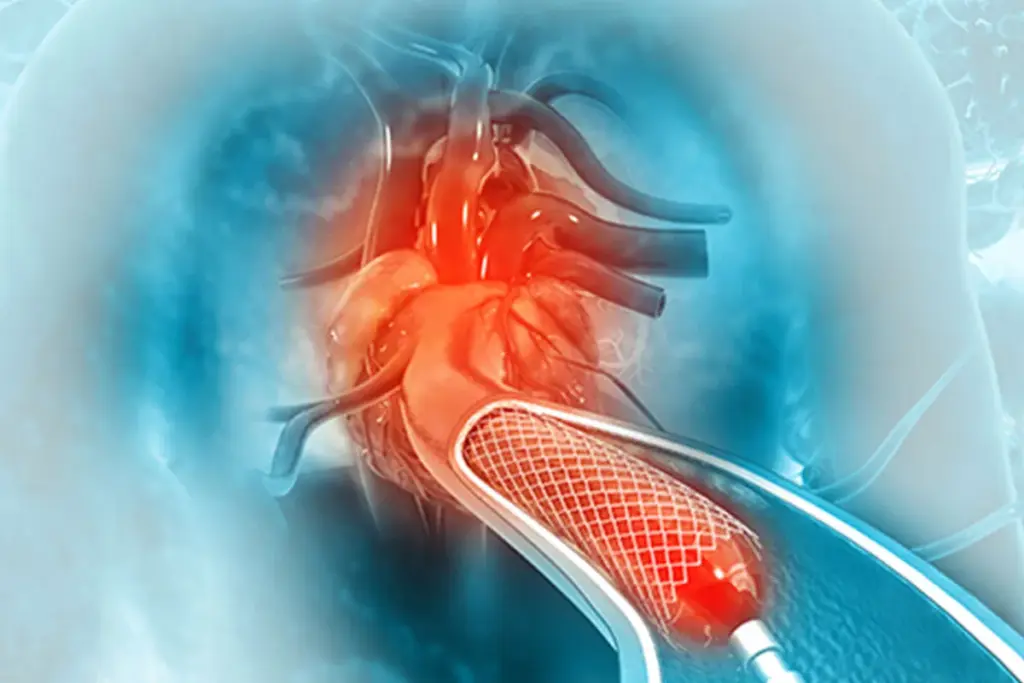
Stents are small, mesh tubes used to support arteries and improve blood flow. They are key in treating many heart and blood vessel problems.
Definition and Types of Stents
Stents are made from metal or polymer. There are bare metal stents, drug-eluting stents, and bioresorbable stents. Each type is made for different heart and blood vessel needs.
“Stents have greatly improved angioplasty results,” say heart doctors. “They keep arteries open, changing how we treat heart disease.”
The Role of Stents in Cardiovascular Treatment
Stents keep arteries open, ensuring blood flows well to important organs. They are often used in heart arteries to treat heart disease. This disease happens when plaque builds up, leading to heart attacks.
Stents help reduce symptoms like chest pain and shortness of breath. This makes life better for people with heart disease.
Common Conditions Requiring Stent Placement
Stents are needed for heart disease, artery disease in the legs, and carotid artery disease. These diseases narrow or block arteries, causing serious health issues if not treated.
- Coronary artery disease: Stents open blocked heart arteries, lowering heart attack risk.
- Peripheral artery disease: Stents boost blood flow to the legs, easing pain when walking.
- Carotid artery disease: Stents prevent strokes by keeping carotid arteries open.
In summary, stents are very important in treating heart and blood vessel diseases. They offer a non-invasive way to keep arteries open and improve patient results.
The Evolution of Stent Technology
Stent technology has seen big changes over the years. It has changed how we treat heart problems. From the first stents to the latest ones, we’ve made big steps forward. These steps have made treatments better and given patients more choices.
Bare Metal Stents: The Foundation
The start of bare metal stents was a big deal for heart disease treatment. These stents helped keep arteries open, improving blood flow. But, they had a problem: they could cause the arteries to narrow again.
The Advent of Drug-Eluting Stents
Drug-eluting stents brought a big leap forward. They release medicine that stops arteries from narrowing. This made stents work better for longer periods.
Latest Innovations in Stent Design
New stents, like bioresorbable stents, are now available. These stents dissolve over time, which could mean fewer long-term problems. There are also stents that are more flexible and easier to use, helping with tricky heart problems.
These new stents have changed how we treat heart issues. They offer better and safer options for patients. With ongoing research, we’ll see even more improvements that will help patients live better lives.
How Long Do Stents Last?
Stent longevity depends on several factors, including the type of stent. Knowing how long a stent lasts is key for patients after angioplasty. It affects their health and quality of life over time.
Average Lifespan of Different Types of Stents
The lifespan of a stent varies by type. Bare metal stents and drug-eluting stents have different lifespans. Bare metal stents might face a higher risk of restenosis in the first year. Drug-eluting stents, on the other hand, reduce this risk significantly.
Drug-eluting stents release medication to prevent new tissue growth. They are popular for their effectiveness in preventing restenosis. Studies show they can last longer than bare metal stents, often several years.
Factors Affecting Stent Durability
Several factors can affect a stent’s durability. Patient-related factors like age, health, and lifestyle choices matter. The procedural technique and the quality of the stent also play a role.
Other factors include health conditions like diabetes, stent size and location, and following post-procedure medication. Knowing these factors helps manage expectations and potentially extend the stent’s lifespan.
Signs of Stent Failure or Deterioration
It’s important for patients to know the signs of stent failure or deterioration. Common signs include recurring chest pain, shortness of breath, or symptoms similar to before the stent placement. If these symptoms happen, getting immediate medical help is critical.
Regular check-ups with healthcare providers are key for monitoring the stent. Being aware of signs and keeping up with check-ups helps ensure the stent lasts longer.
Bare Metal Stents: Durability and Limitations
Bare metal stents play a key role in treating heart conditions. They are used in angioplasty to open blocked arteries. Their simplicity and quick results make them popular.
Expected Lifespan of Bare Metal Stents
Bare metal stents are durable and can last many years. Research shows they can stay effective for up to 15 years. This depends on the patient’s health and lifestyle.
Common Issues with Bare Metal Stents
Despite their long life, bare metal stents have risks. One major issue is restenosis, or the artery narrowing again. This can happen in up to 30% of patients and may need more treatments.
Another problem is stent thrombosis. This is when a blood clot forms in the stent. It can lead to serious heart problems.
When Bare Metal Stents Are Preferred
In some cases, bare metal stents are the best choice. They are good for patients at high risk of bleeding or who can’t take long-term antiplatelet therapy. Their simplicity and lower cost also make them appealing in some situations.
Drug-Eluting Stents: Longevity and Effectiveness
Drug-eluting stents have changed cardiology by giving a better way to fight coronary artery disease. These stents release medicine that stops cells from growing, which lowers the chance of the artery getting blocked again.
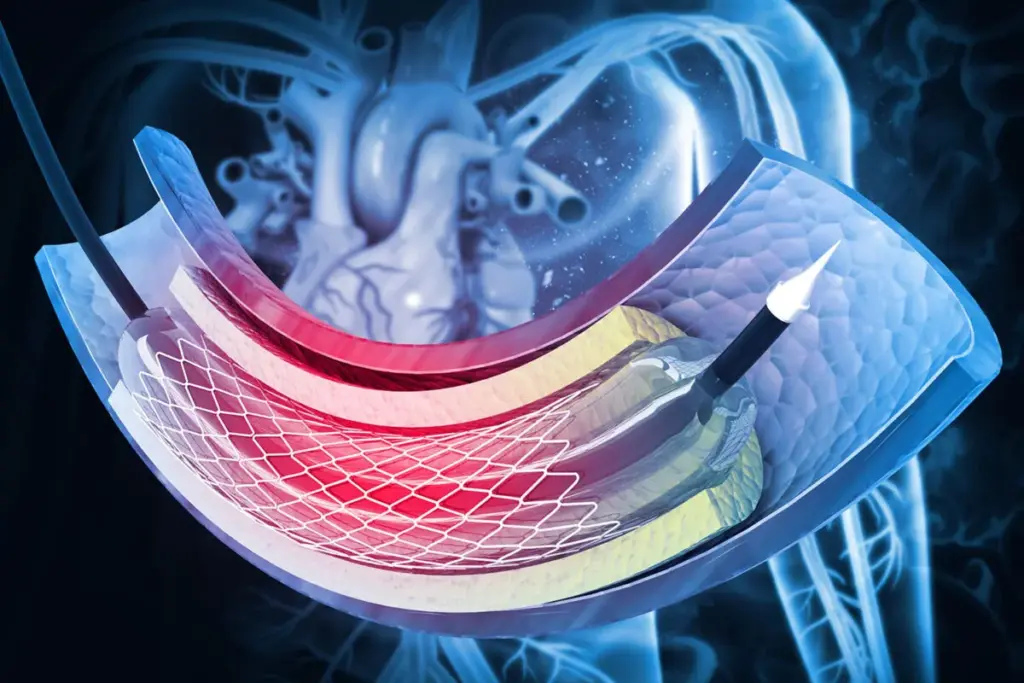
How Drug Coatings Extend Stent Functionality
The drug coating on drug-eluting stents is key to their success. It releases drugs like sirolimus or paclitaxel, which stop tissue from growing around the stent. This keeps the artery open, improving patient outcomes after angioplasty.
“Drug-eluting stents have changed cardiology,” says a top cardiologist. “They prevent blockages, making them essential in fighting heart disease.”
Comparative Longevity to Bare Metal Stents
Drug-eluting stents last longer than bare metal stents. They have fewer blockages and need fewer repeat procedures. This is because the drug coating stops too much tissue from growing.
- Drug-eluting stents reduce the risk of restenosis by releasing medication.
- They have a lower rate of target lesion revascularization compared to bare metal stents.
- Their effectiveness has been proven in numerous clinical trials.
Latest Research on Drug-Eluting Stent Durability
New studies confirm drug-eluting stents are durable and effective. A study in the Journal of the American College of Cardiology showed better results with newer stents. These improvements have made drug-eluting stents even more important in cardiology.
Following new research, it’s clear drug-eluting stents are key in treating heart disease. They meet patient needs, making them essential in heart care.
Bioresorbable Stents: A Temporary Solution
Bioresorbable stents are changing how we treat heart problems. They offer a temporary fix by supporting the artery while it heals. Then, they dissolve, leaving no lasting implant behind.
How Bioresorbable Stents Work
Like traditional stents, bioresorbable stents keep the artery open after a procedure. But they’re made to dissolve, avoiding long-term issues with metal stents.
The process is simple:
- Initial support: The stent holds the artery open.
- Gradual absorption: The body absorbs the stent over time.
- Restoration of natural vessel function: Once gone, the artery works like before, without a foreign object.
Timeline for Absorption
The time it takes for a bioresorbable stent to dissolve varies. Usually, it’s 2 to 3 years after it’s put in. This matches the artery’s healing time, keeping it open when it needs it most.
Benefits and Limitations
Bioresorbable stents have many advantages:
- They lower the risk of problems that metal stents can cause.
- They might help the artery work naturally again.
- They could make future treatments easier, without a permanent implant.
But, there are downsides too:
- They cost more than traditional stents at first.
- We don’t have as much data on their long-term safety and success.
- There’s a chance of complications like blood clots while they dissolve.
More research will help us understand how bioresorbable stents fit into heart care.
Anatomical Placement and Its Impact on Stent Longevity
The place where a stent is put matters a lot for how long it lasts. Different areas of the blood vessels face different stresses and pressures. These can change how well a stent works over time.
Coronary Artery Stents
Coronary artery stents are very common. They go in the arteries that feed the heart. These arteries are always moving with blood and can get clogged.
Drug-eluting stents are great here because they release medicine. This medicine stops the artery from getting too narrow.
Stents for the heart have gotten a lot better. They last longer and cause fewer problems. This is thanks to new materials that are safe for the body.
|
Stent Type |
Average Lifespan |
Common Complications |
|---|---|---|
|
Bare Metal Stents |
5-10 years |
Restenosis |
|
Drug-Eluting Stents |
10+ years |
Stent thrombosis |
Peripheral Vascular Stents
Peripheral vascular stents are for arteries outside the heart, like in the legs. They face high pressures and can get squished. How long they last depends on the patient’s activity and health.
We suggest regular check-ups to keep an eye on these stents. This way, we can catch any problems early.
Carotid and Cerebral Stents
Carotid and cerebral stents are for the brain’s blood vessels. They are key to avoiding strokes. They need to be placed very carefully because of the brain’s delicate blood vessels.
The life of these stents can be affected by the patient’s overall health. Things like high blood pressure or diabetes can play a role.
Factors That Influence Stent Longevity
Many factors affect how long a stent lasts. These include things about the patient and the procedure. Knowing these helps make stents work better and helps patients get the best care.
Patient-Related Factors
Things about the patient can really impact stent life. These include:
- Lifestyle Choices: Smoking, diet, and exercise can all affect how long a stent lasts.
- Health Conditions: Having diabetes, high blood pressure, or high cholesterol can also play a role.
- Genetic Predispositions: Some genetic traits can affect how well a stent works in a patient’s body.
- Adherence to Medication: Taking the right medicine is key to avoiding stent problems.
For example, smoking can make stents more likely to fail. Also, diabetes can shorten stent life because of inflammation and platelet issues.
Procedural Factors
How the stent is put in also matters a lot. These include:
- Stent Type: The type of stent used, like bare metal or drug-eluting, can affect its life.
- Stent Placement Technique: The skill and precision of the placement can impact how well the stent works.
- Vessel Characteristics: The size and health of the blood vessel where the stent is placed can also matter.
Drug-eluting stents, for instance, can help prevent restenosis better than bare metal stents. The way the stent is placed, including making sure it fits right, is also very important.
By understanding and addressing these factors, doctors can help stents last longer and improve patient care.
Complications That May Shorten Stent Life
Stents save many lives, but some problems can shorten their life. It’s important for patients and doctors to know about these issues. This way, they can try to avoid or lessen the risks of stent problems.
Restenosis: Causes and Prevention
Restenosis is when arteries narrow again after a stent is placed. It happens because the body reacts to the stent by growing new tissue inside it.
Many things can lead to restenosis. These include the type of stent, health conditions like diabetes, and inflammation. To stop restenosis, doctors use drug-eluting stents. These stents release medicine to stop new tissue from growing.
|
Causes of Restenosis |
Prevention Strategies |
|---|---|
|
Body’s response to stent injury |
Use of drug-eluting stents |
|
Patient health conditions (e.g., diabetes) |
Management of underlying health conditions |
|
Inflammation |
Anti-inflammatory medications |
Stent Thrombosis
Stent thrombosis is when a blood clot forms in the stent. It’s rare but very dangerous. It can cause a heart attack without warning.
Risk factors for stent thrombosis include stopping antiplatelet drugs too soon, not responding well to them, and health problems. Taking your medicine as directed is key to avoiding this risk.
Stent Fracture
Stent fracture is when the stent breaks. This can cause problems like restenosis or thrombosis. The risk depends on the stent’s design, where it’s placed, and the patient’s health.
To lower the chance of stent fracture, choosing the right stent and placing it carefully is important.
Knowing about these problems and how to prevent them helps patients and doctors. Together, they can make stents last longer and keep hearts healthy.
Post-Procedure Care and Its Impact on Stents
Good post-procedure care can really help a stent last longer and work better. After angioplasty, patients need to follow a detailed care plan. This ensures the stent works right and stays strong.
Immediate Post-Angioplasty Care
Right after angioplasty, it’s all about watching for problems and managing symptoms. Patients are kept under close watch for a few hours to catch any immediate issues like bleeding. It’s key to rest and not do too much during the first few days.
Key aspects of immediate care include:
- Resting the affected limb or area
- Monitoring the puncture site for signs of bleeding or hematoma
- Managing pain with prescribed medications
- Following specific instructions provided by the healthcare team
Medication Regimens
Medicine is a big part of caring for a patient after angioplasty. Patients usually take antiplatelet therapy to stop clots from forming around the stent. It’s very important to stick to the medication plan to avoid problems like stent thrombosis.
Common medications include:
- Aspirin
- P2Y12 inhibitors (e.g., clopidogrel, ticagrelor)
- Other medications as necessary to manage conditions like hypertension or high cholesterol
Follow-up Appointments and Monitoring
Regular check-ups are key to keeping an eye on the stent and heart health. These visits help doctors see how the patient is doing, tweak medications if needed, and catch any problems early.
At follow-up visits, patients can expect their doctor to:
- Watch for signs of stent failure or restenosis
- Adjust medication regimens as necessary
- Give advice on lifestyle changes to help heart health
When Stent Replacement Becomes Necessary
Knowing when to replace a stent is key for good care. A stent needs to be replaced if it’s not working right. This can happen for reasons like the artery getting narrow again or a blood clot forming in the stent.
Indicators for Stent Replacement
There are signs that show a stent might need to be replaced. These include:
- Restenosis: The artery getting narrow again in the stented area.
- Stent Thrombosis: A blood clot forming inside the stent.
- Stent Fracture: The stent breaking down.
Signs like chest pain or trouble breathing might mean the stent is failing. If you have these symptoms, get help right away.
The Replacement Procedure
The steps to replace a stent are similar to putting one in for the first time. It involves:
- Angiography: To see the arteries and check the stent’s condition.
- Balloon Angioplasty: To clear the blockage.
- New Stent Placement: To keep the artery open.
This is done by an interventional cardiologist in a special lab.
Recovery and Expectations
Recovering from a stent replacement is like the first time. Patients are watched for a few hours and might go home the same day. Post-procedure care includes:
- Following the doctor’s advice on medicine.
- Going to check-ups to see how the stent is doing.
- Making healthy lifestyle choices to lower heart risk.
It’s important to listen to your doctor to keep the new stent working well and stay healthy.
Common Patient Questions About Stent Longevity
Patients often wonder about their stent’s lifespan after an angioplasty. We, as medical experts, know how vital it is to answer these questions. This helps us give clear and reassuring answers.
Will I Need Another Stent Procedure?
Whether you’ll need another stent depends on several things. These include the stent type, artery condition, and your health. Drug-eluting stents, for instance, can lower restenosis risk more than bare metal stents.
A study compared different stent types’ long-term results. Here’s a quick summary:
|
Stent Type |
Restenosis Rate |
Average Lifespan |
|---|---|---|
|
Bare Metal Stents |
20-30% |
5-10 years |
|
Drug-Eluting Stents |
5-10% |
10+ years |
|
Bioresorbable Stents |
Varies |
Temporary |
Can I Feel When My Stent Is Failing?
Stent failure or restenosis might not show symptoms until it’s severe. But, some may feel angina-like symptoms or chest pain. It’s key to keep up with your cardiologist’s appointments to check on your stent.
How to Maximize Your Stent’s Lifespan
To extend your stent’s life, live a healthy lifestyle. Eat well, exercise regularly, and don’t smoke. Also, follow your medication plan closely. Aspirin and antiplatelet therapy help prevent clots.
Knowing what affects your stent’s life and taking action can greatly improve it. This, in turn, boosts your heart health.
Living with a Stent: Long-term Outlook
Having a stent is not just a one-time thing. It’s a long-term journey that requires ongoing care and lifestyle changes. Understanding what makes for a healthy and happy life is key.
Quality of Life Considerations
Having a stent can change your life a lot. Sticking to your medication and making lifestyle changes are important. Here’s what we suggest:
- Eat a heart-healthy diet with lots of fruits, veggies, and whole grains
- Do regular physical activities like walking or swimming to keep your heart healthy
- Use stress-reducing activities like meditation or yoga
By adding these habits to your daily routine, you can improve your overall health and lower the risk of problems.
Long-term Monitoring Requirements
Regular check-ups are key to keeping your stent working well and catching any problems early. Going to your follow-up appointments is important for:
- Checking how the stent is doing and your heart health
- Changing your medication if needed to avoid problems
- Talking about any concerns or symptoms you have
We stress the importance of keeping these appointments to get the best care.
Activities to Avoid or Embrace
When you have a stent, some activities might need to be changed or avoided. For example:
- Avoid heavy lifting or bending to protect the stent site
- Choose low-impact exercises like cycling or tai chi to stay active
Talking to your doctor about travel plans is also important, if you’ll be far from medical help.
By knowing what you need and making smart choices, people with stents can live active and happy lives.
Conclusion
Knowing how long stents last and what affects their durability is key. We’ve looked at different stents and how they help keep our hearts healthy. This includes bare metal, drug-eluting, and bioresorbable stents.
How long a stent lasts depends on several things. These include the patient’s health, the procedure, and aftercare. By understanding these, patients can help their stents last longer and stay healthy.
As stent technology and heart care get better, staying updated is important. This helps us give the best care to those with heart conditions. It also improves their life quality and health outcomes related to stents and heart health.
FAQ
What is the average lifespan of a stent?
The lifespan of a stent depends on its type and the patient’s health. Bare metal stents usually last 10-15 years. Drug-eluting stents can last 15 years or more.
How do I know if my stent is failing?
If you have chest pain, shortness of breath, or feel tired, your stent might be failing. Seeing a doctor quickly is important.
Can lifestyle changes affect the longevity of my stent?
Yes, eating well, exercising, and not smoking can help your stent last longer.
What are the common complications associated with stents?
Stents can cause restenosis, stent thrombosis, and stent fracture. Knowing about these and how to prevent them is key.
How often do I need to follow up with my doctor after stent placement?
Regular check-ups with your doctor are vital. How often you need to go depends on your health and the stent type.
Can I feel when my stent is failing?
Sometimes, you might feel chest pain or shortness of breath if your stent is failing. But, you might not always notice symptoms. That’s why regular doctor visits are important.
What is the difference between bare metal stents and drug-eluting stents?
Bare metal stents are just metal and keep the artery open. Drug-eluting stents release medicine to prevent the artery from narrowing.
Are bioresorbable stents a viable option for everyone?
Bioresorbable stents are new and not right for everyone. Your doctor will decide if they’re good for you based on your health and the problem they’re treating.
How does the location of stent placement affect its longevity?
Where the stent is placed can affect how long it lasts. Stents in coronary arteries might not last as long as those in peripheral vessels.
What are the benefits and limitations of bioresorbable stents?
Bioresorbable stents can be absorbed by the body, which might reduce long-term risks. But, they might be more expensive and need more research on their long-term effects.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC6199519/[2





