Nearly 800,000 Americans get a stent in their heart each year. This shows how common coronary artery disease is. It also shows how important stent placement is in treating it. How serious is stenting? It’s invasive but safe. Get best vital safety facts. It prevents dangerous heart attacks and saves amazing lives daily.
Thinking about getting a cardiac stent can be scary. But stenting is a common treatment. It involves putting a small, mesh-like device in the artery. This keeps the artery open and improves blood flow to the heart.
It’s important for patients to understand the procedure and its effects. We’ll look into what happens during stenting. We’ll also talk about what patients can expect.
Key Takeaways
- Stent placement is a common treatment for coronary artery disease.
- The procedure involves placing a small mesh-like device in the artery.
- Understanding the implications of stenting is important for patients.
- The treatment aims to improve blood flow to the heart.
- Patients should know what to expect during and after the procedure.
Understanding Cardiac Stents
Cardiac stents have changed how we treat heart disease. They are small, mesh-like tubes that keep arteries open. This ensures blood flows well to the heart muscle.
What is a Cardiac Stent?
A cardiac stent is a device for treating blocked arteries. It’s used in angioplasty to keep the artery open. This improves blood flow to the heart.
The stent acts as a scaffold. It prevents the artery from collapsing or getting blocked again.
Types of Stents: Bare Metal vs. Drug-Eluting
There are two main types of stents: bare metal stents and drug-eluting stents. Bare metal stents are made of metal mesh. They physically keep the artery open.
Drug-eluting stents are coated with medication. This medication is slowly released. It helps prevent the artery from getting blocked again by reducing tissue growth around the stent.
- Bare Metal Stents: Simple in design, these stents are less likely to cause allergic reactions and are less expensive.
- Drug-Eluting Stents: These stents release medication to prevent cell proliferation, reducing the risk of restenosis.
Materials Used in Modern Stents
Modern cardiac stents are made from durable, body-compatible materials. These include stainless steel, cobalt-chromium, and platinum-chromium alloys. The material choice depends on the patient’s condition and the blockage’s location.
New materials and technologies are making stents safer and more effective. This leads to better results for patients undergoing angioplasty and stenting.
When is a Stent Necessary?

Deciding to use a stent depends on several things. These include how bad the blockages in the coronary arteries are and if symptoms are present. We will look into these details to see when a stent is needed.
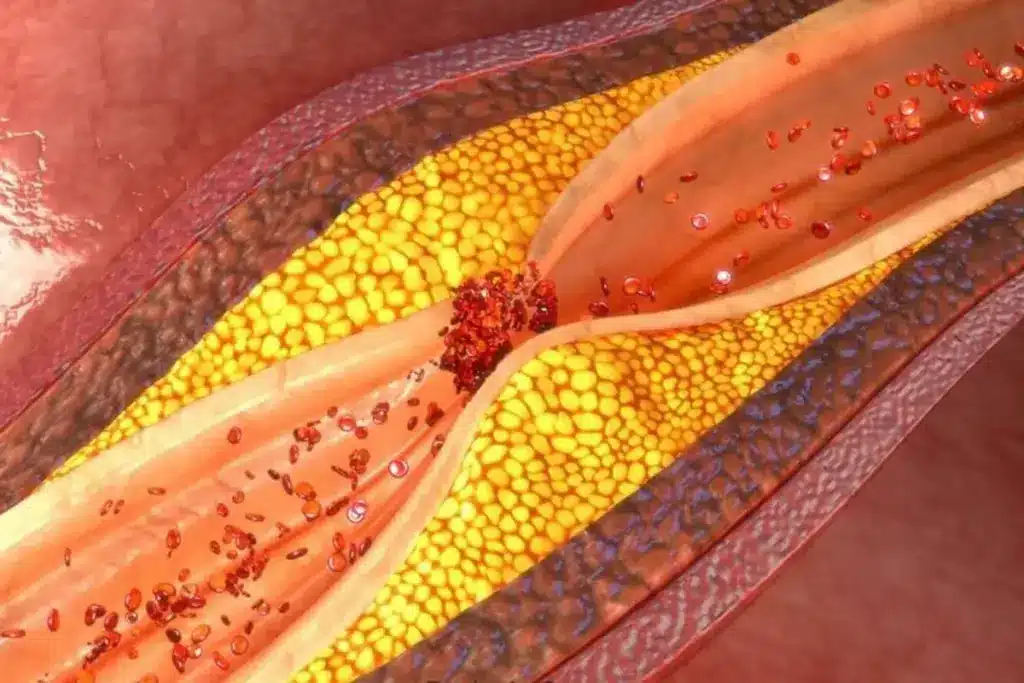
Coronary Artery Disease and Blockages
Coronary artery disease happens when arteries to the heart get narrowed or blocked. This is due to plaque buildup, known as atherosclerosis. It can lead to less blood flow to the heart, causing chest pain, heart attacks, or other serious issues.
Plaque buildup happens over time. It’s affected by diet, lifestyle, and genetics. As plaque grows, it can harden or burst, causing blood clots. These clots can block or completely stop an artery.
Symptoms Indicating Need for Intervention
Certain symptoms mean coronary artery disease might need a stent. These symptoms include:
- Chest pain or discomfort (angina)
- Shortness of breath
- Fatigue
- Pain or discomfort in the arms, back, neck, jaw, or stomach
Having these symptoms doesn’t always mean you need a stent. But, they do mean you should see a doctor for a full check-up.
Diagnostic Tests Before Stent Recommendation
Before suggesting a stent, doctors do several tests. These tests check how bad the coronary artery disease is and the size of blockages. Tests might include:
|
Diagnostic Test |
Purpose |
|---|---|
|
Stress Test |
Evaluates heart function under stress to identify possible blockages |
|
Coronary Angiogram |
Shows detailed images of the coronary arteries to find blockages |
|
Cardiac Catheterization |
Examines the heart’s chambers and coronary arteries |
These tests are key in deciding if a stent is needed. They help plan the best treatment.
In summary, needing a stent depends on several factors. These include the severity of coronary artery disease, symptoms, and test results. Knowing these helps doctors choose the best treatment for patients.
The Stenting Procedure: What to Expect
Stenting is a common and effective way to treat coronary artery disease. Knowing what to expect can make the process less scary.
Pre-Procedure Preparation
We make sure you’re ready for the stenting procedure. This includes a detailed medical check-up, looking at your medical history, and doing tests like blood work and imaging studies. You might need to stop certain medicines beforehand, so it’s important to follow our instructions.
Preparation Steps:
- Fasting for a set time before the procedure
- Getting someone to drive you home after
- Talking about any allergies or concerns with your healthcare team
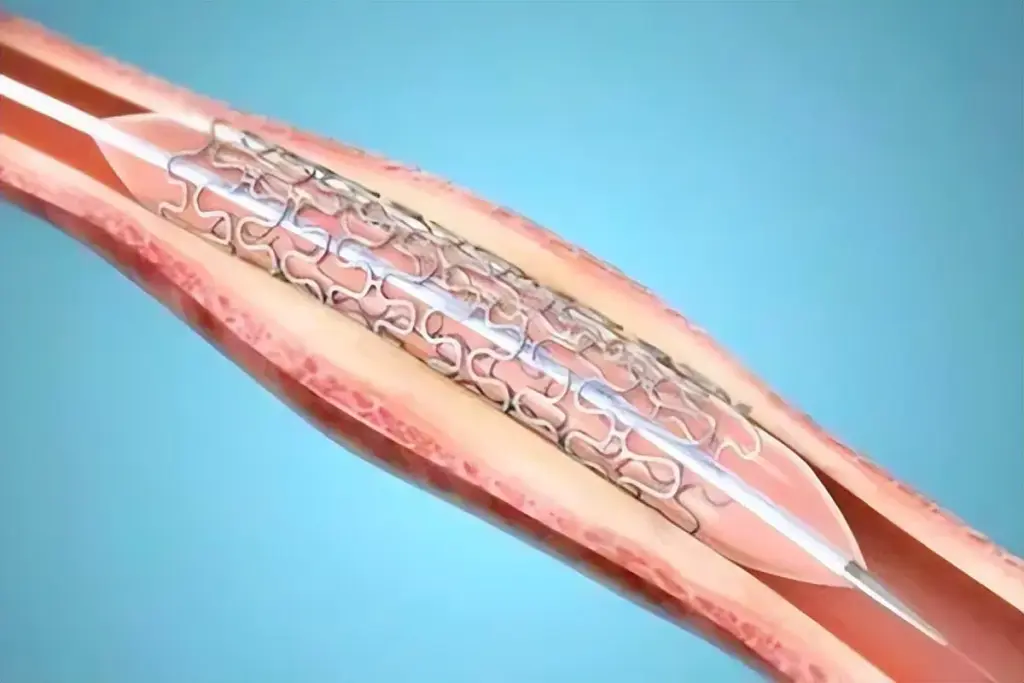
Step-by-Step Process of Stent Placement
The stenting procedure has several steps. First, we numb the area where the catheter will go, usually in the groin or arm. Then, we put a thin, flexible tube called a catheter into the artery and guide it to the blocked area using imaging technology.
Next, we inflate a balloon to open the artery. After that, we place a stent to keep the artery open. The stent is a small, mesh-like device that stays in place forever.
|
Step |
Description |
|---|---|
|
1 |
Insertion of the catheter into the artery |
|
2 |
Guiding the catheter to the blocked area |
|
3 |
Inflating a balloon to open the artery |
|
4 |
Placing the stent to keep the artery open |
Duration and Type of Anesthesia Used
The stenting procedure usually takes about 30 minutes to an hour. It can take longer if the case is more complex. We use local anesthesia to numb the area where the catheter is inserted, so you stay comfortable during the procedure.
In some cases, we might also use conscious sedation to help you relax. This means you’ll be in a relaxed state but can follow instructions.
After the procedure, we watch you for a short time to make sure everything is okay. You might feel some soreness at the catheter site, but it usually goes away quickly.
How Serious is Stent Placement?
It’s important for patients to know how serious stent placement is. This procedure is common for treating heart disease. It’s serious but can be compared to other heart surgeries.
Stent placement is less invasive than some surgeries. This means it has smaller cuts and less body trauma. It usually leads to fewer problems and a quicker recovery.
Comparing Stenting to Other Cardiac Procedures
Stenting is compared to CABG and other heart surgeries. Unlike CABG, stenting is minimally invasive. It uses smaller cuts and causes less body trauma.
This makes stenting less serious. It often leads to fewer complications and a quicker recovery.
Minimally Invasive Nature of Stenting
The benefits of stenting include its minimally invasive nature. A catheter is used to place a stent in a blocked artery. This is guided by imaging technology.
This method lowers the risk of infection and speeds up healing. Patients usually feel less pain and discomfort than with more invasive surgeries.
Typical Recovery Timeline
Recovery from stenting is usually quick. Most patients can go back to normal activities in a few days to a week. The recovery timeline can vary based on health and any complications.
Patients are told to avoid heavy lifting and strenuous activities for a short time. Knowing the recovery process and following post-procedure instructions is key. It helps minimize stent risks and ensures the procedure’s success.
Understanding stent placement’s seriousness helps patients prepare. It empowers them to make informed decisions about their heart care. This knowledge highlights the stent benefits for better heart health and overall well-being.
Potential Risks and Complications of Stenting
Cardiac stenting is very effective, but it comes with risks. It’s important to know these risks. They can affect people differently.
Immediate Procedure-Related Complications
Right after the stenting, some problems can happen. These include:
- Bleeding or hematoma at the catheter site
- Allergic reactions to the contrast dye used
- Damage to the blood vessels or heart
- Arrhythmias or irregular heartbeats
- Stent thrombosis (clot formation within the stent)
Stent thrombosis is very serious. It can cause a heart attack or death. But, modern stents and treatments have made this risk much lower.
Short-Term Risks (First Month)
In the first month, patients face risks like:
- Infection at the catheter site
- Bleeding complications due to antiplatelet therapy
- Restenosis (re-narrowing of the artery)
To lower these risks, doctors often use dual antiplatelet therapy. This includes aspirin and a P2Y12 inhibitor. Taking these medicines as directed is key to avoiding problems.
Long-Term Complications to Be Aware Of
Long-term, patients might face:
|
Complication |
Description |
Management |
|---|---|---|
|
Restenosis |
Re-narrowing of the stented artery |
Monitoring, possible repeat stenting or CABG |
|
Stent Thrombosis |
Clot formation within the stent |
Life-long antiplatelet therapy, monitoring |
|
In-stent Neoatherosclerosis |
Formation of new plaque within the stent |
Monitoring, possible additional stenting |
Knowing about these risks and talking to your doctor can help. It can make your treatment better and safer.
Benefits of Cardiac Stenting
Cardiac stenting is more than a procedure. It’s a step towards better heart health and a better life. It helps those with coronary artery disease in many ways.
Immediate Symptom Relief
Cardiac stenting quickly eases symptoms like chest pain and shortness of breath. It opens up blocked arteries, making the heart work better.
Key benefits of immediate symptom relief include:
- Less frequent and severe angina episodes
- Easier daily activities without pain
- Better overall feeling and less worry about heart issues
Improved Blood Flow and Heart Function
Stenting makes blood flow better to the heart. This not only eases symptoms but also boosts heart function. The heart gets the oxygen and nutrients it needs.
Quality of Life Improvements
Life quality for patients after stenting can really improve. With fewer symptoms and better heart function, they can do more of what they love. This is a big part of the stent benefits patients see.
Some quality of life improvements include:
- More ability to do physical activities and exercise
- Better mental health from fewer symptoms and more physical ability
- Healthier outcomes from better blood flow and lower heart risk
Understanding the benefits of cardiac stenting helps patients make better choices. These benefits include quick symptom relief, better blood flow and heart function, and a better life overall.
Life After Stent Placement
The time after getting a stent is very important. You need to manage your medicines, lifestyle, and activities well. This helps you recover well and lowers the chance of problems.
Essential Medications Following Stent Placement
After getting a stent, doctors usually give you medicines to stop blood clots. You might take aspirin and a P2Y12 inhibitor like clopidogrel. How long you take these medicines depends on the stent type and your health risks.
Common Antiplatelet Medications:
- Aspirin
- Clopidogrel (Plavix)
- Prasugrel (Effient)
- Ticagrelor (Brilinta)
Dietary and Lifestyle Modifications
Living a heart-healthy lifestyle is key after getting a stent. This means changing your diet, being more active, and quitting smoking.
Dietary Recommendations:
- Eat more fruits, veggies, and whole grains
- Drink less saturated fats, cholesterol, and sodium
- Don’t drink too much alcohol
|
Dietary Component |
Recommended Changes |
|---|---|
|
Fats |
Limit saturated and trans fats; choose healthy fats like avocado and nuts |
|
Sodium |
Reduce intake to less than 2,300 mg per day |
|
Fiber |
Increase intake of fruits, vegetables, and whole grains |
Activity Restrictions and Resumption
You can usually go back to normal activities a few days to a week after getting a stent. But, always listen to what your doctor says about how active you can be.
By managing your medicines, making lifestyle changes, and following activity advice, you can do well after getting a stent.
Phase1 of Cardiac Rehabilitation
Cardiac rehabilitation phase1 is key after a stent is placed. It helps patients recover, manage their health, and live healthier. This phase is all about getting better and preparing for a new lifestyle.
In-Hospital Recovery Process
The recovery starts right after the stent is placed. Our team watches over patients for any issues and makes sure they’re okay to go home. We start with gentle movements to avoid problems from staying in bed too long.
“Early mobilization is key to a successful recovery,” says a top cardiologist. “Moving patients gently helps lower risks and boosts results.”
Initial Exercises for Cardiac Rehab Phase1
The first exercises are easy and help keep blood flowing and muscles flexible. Patients might do leg lifts, arm raises, and short walks. Our team adjusts these exercises to fit each patient’s needs and abilities.
- Leg lifts to improve circulation
- Arm raises to maintain range of motion
- Short walks to promote gentle mobilization
Education and Preparation for Discharge
Learning is a big part of phase1. We teach patients about managing their health, including diet, meds, and warning signs. This knowledge makes patients feel ready and confident for going home.
Key areas of education include:
- Understanding and managing medications
- Dietary modifications to support heart health
- Recognizing warning signs that require medical attention
As patients move through phase1, we check if they’re ready to go home. We give them personalized advice for a smooth transition.
Phase2 Cardiac Rehab: Structured Outpatient Program
After the initial recovery, patients move into Phase 2 cardiac rehab. It’s a structured program for those who have had heart procedures or events. It helps improve heart health through exercise and education.
Structure and Duration
Phase 2 lasts several weeks to a few months. The time depends on the patient’s condition and progress. Patients visit a cardiac rehab facility regularly during this time.
Key components of Phase 2 include:
- Supervised exercise sessions tailored to the patient’s needs and abilities
- Continuous monitoring of vital signs and heart function during exercise
- Education on heart-healthy lifestyle choices, including diet and stress management
- Ongoing support from a multidisciplinary team of healthcare professionals
Supervised Exercise Sessions
Exercise is key in Phase 2 cardiac rehab. Patients do activities like walking, cycling, or using resistance machines. These supervised exercise sessions help improve heart fitness and physical function.
A leading cardiologist says, “Exercise training is vital in cardiac rehab. It offers many benefits for those recovering from heart events or procedures.”
Cardiac Rehab Exercises for Phase2
Exercises in Phase 2 are customized for each patient. They may include:
- Aerobic exercises like brisk walking, swimming, or cycling
- Resistance training to build muscle strength
- Flexibility exercises to improve range of motion
These exercises are led by experienced healthcare professionals. They watch how patients do and adjust the program as needed.
By the end of Phase 2, patients have made big strides in their recovery. They have better heart health and know how to keep it healthy.
Phase3 Cardiac Rehab: Maintenance and Independence
As patients move through cardiac rehab, they reach Phase 3. This stage is all about keeping independence and health for the long run. At this point, they’ve made big strides and are ready to take care of themselves.
Transitioning to Self-Managed Care
In Phase 3, patients become more involved in their care. They make health decisions with more confidence. We urge them to keep an eye on their progress, set achievable goals, and ask for help when needed.
Switching to self-care involves several important steps, including:
- Keeping track of vital signs and health metrics
- Following a balanced diet and exercise plan
- Handling stress and staying in touch with healthcare providers
Exercise Progression and Intensity
In Phase 3, exercise plans get more tailored to each person’s fitness and goals. We suggest sticking to a mix of cardio, strength training, and flexibility exercises. This helps keep the heart healthy.
Patients should:
- Slowly increase workout intensity as they feel comfortable and get approval from their doctor
- Try new activities or sports to keep workouts fun
- Rest when needed and avoid pushing too hard
Long-term Lifestyle Management Strategies
Managing lifestyle long-term is key to keeping up with cardiac rehab benefits. We stress the need for:
- Eating a heart-healthy diet full of fruits, veggies, and whole grains
- Drinking plenty of water and cutting down on alcohol
- Quitting smoking and avoiding secondhand smoke
By focusing on these habits, people can greatly lower their risk of heart problems and live better lives.
Phase 3 cardiac rehab is a big step towards lasting health and freedom. By managing their care, exercising wisely, and living a healthy lifestyle, patients can keep up their progress. They can enjoy a healthier, more rewarding life.
When to Contact Your Doctor After Stent Placement
Knowing when to call your doctor after a stent is key. Your health is our main concern. Knowing what to look out for can greatly help your recovery.
Emergency Warning Signs Requiring Immediate Attention
Some symptoms mean you need to see a doctor right away. If you notice any of these, act fast:
- Severe chest pain or discomfort that doesn’t go away
- Shortness of breath or difficulty breathing
- Severe headache or confusion
- Weakness or numbness in your face, arm, or leg
- Severe pain or swelling in your leg
If you see any of these emergency warning signs, call for help or get someone to take you to the hospital.
Non-Emergency Concerns to Discuss
Some symptoms are not urgent but should be talked about at your next visit. These include:
- Mild chest discomfort or pain that resolves on its own
- Fatigue or general feeling of being unwell
- Concerns about your medications or side effects
- Any other unusual symptoms or concerns
If you’re not sure if your symptoms are serious, contact your doctor for advice.
Follow-up Appointment Schedule
After a stent, regular check-ups are important. They help track your progress and adjust your care plan. Your doctor will likely schedule:
- A follow-up visit within a few days to a week after the procedure
- Additional visits as necessary based on your recovery progress
These visits help us check how your heart is doing, adjust your meds, and talk about any worries. Keeping these appointments is key for the best results.
Long-Term Outcomes and Success Rates of Stenting
Stenting’s long-term success depends on the stent type, patient health, and care after the procedure. Knowing these factors helps both patients and doctors make better choices.
Statistical Success Rates by Stent Type
The success of stenting changes with the stent type. Bare metal stents and drug-eluting stents have different success rates and uses.
|
Stent Type |
Success Rate |
Restenosis Rate |
|---|---|---|
|
Bare Metal Stents |
80-90% |
20-30% |
|
Drug-Eluting Stents |
90-95% |
5-10% |
Drug-eluting stents have better success rates and lower restenosis rates than bare metal stents, as shown in the table.
Factors Affecting Long-Term Outcomes
Many things can affect stenting’s long-term success. These include how well the patient follows medication, makes lifestyle changes, and has other health issues.
- Patient Compliance: Following antiplatelet therapy is key to avoiding stent thrombosis.
- Lifestyle Changes: Eating right, quitting smoking, and exercising can help outcomes.
- Comorbid Conditions: Having diabetes, high blood pressure, and other heart diseases can impact stent success.
A study in a top cardiology journal found, “The best results from coronary stenting come from good medicine and lifestyle changes.”
“The mix of stent technology and patient care is essential for good long-term results.”
A Cardiologist
Potential Need for Additional Procedures
Some patients might need more procedures after stenting. This could be because of restenosis or the disease getting worse.
In summary, stenting’s long-term success depends on many things. These include the stent type, patient health, and following care after the procedure. Understanding these helps doctors and patients work together for better results.
Conclusion
Understanding stenting and cardiac rehabilitation is key for heart health. Patients can make better choices about their care by learning about these topics.
Stenting is a big step in fighting coronary artery disease. It works best when paired with cardiac rehab. These programs help patients get better and stay healthy.
Following lifestyle changes, taking medicine, and keeping up with doctor visits are important. We suggest patients work with their doctors to create a plan for heart health after stenting.
Managing heart health is a long-term job. It requires sticking to healthy habits and regular check-ups. With the right strategy, people can see big improvements in their heart health and overall well-being.
FAQ
What is cardiac stenting, and how does it work?
Cardiac stenting is a treatment for coronary artery disease. It involves placing a stent in a narrowed or blocked artery. This keeps the artery open, improving blood flow to the heart.
What are the different types of stents available?
There are two main types of stents. Bare metal stents are made of metal mesh. Drug-eluting stents release medication to prevent cell growth and reduce restenosis risk.
How long does the stenting procedure take?
The procedure itself takes about 30 minutes to an hour. But, preparation and recovery can take several hours overall.
What is the recovery time after stent placement?
Most people can get back to normal in a few days to a week. But, recovery time can vary based on health and the procedure specifics.
What are the possible risks and complications of stenting?
Risks include bleeding, infection, stent thrombosis, and restenosis. These are rare but serious. Following post-procedure care can help minimize risks.
What is cardiac rehabilitation, and what are its phases?
Cardiac rehab helps patients recover from heart conditions and procedures. It has three phases: Phase1 (in-hospital recovery), Phase2 (outpatient program), and Phase3 (maintenance).
What happens during Phase2 cardiac rehab?
Phase2 is an outpatient program with supervised exercise and education. It lasts several weeks to months.
How long do I need to be on medications after stent placement?
Antiplatelet therapy is prescribed to prevent clotting. The duration depends on the stent type and patient factors.
When should I contact my doctor after stent placement?
Seek immediate help for severe chest pain, difficulty breathing, or other emergency signs. For non-emergency concerns, follow your appointment schedule and contact your doctor as needed.
What are the long-term outcomes and success rates of stenting?
Success depends on the stent type, patient care, and overall health. Success rates vary, and some may need more procedures.
How can I manage my lifestyle after stent placement?
After stenting, focus on diet, exercise, stress management, and medication adherence. Cardiac rehab programs offer guidance.
What are the benefits of cardiac stenting?
Stenting offers immediate symptom relief and improved heart function. It also enhances quality of life. Many see a significant reduction in chest pain.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/29242323/





