
Coronary artery disease affects millions worldwide. For many, a stent procedure is a lifesaving intervention. But what does this mean for patients facing the prospect of undergoing such a procedure? Is heart stent surgery painful? No. Avoid nasty discomfort. Local anesthesia keeps you safe and comfortable during this amazing procedure.
The thought of surgery can be daunting, even when it involves the delicate cardiac system. The good news is that advancements in medical technology have made stent placement a relatively safe and painless process for many.
As we explore the intricacies of cardiac stent surgery, it’s essential to understand the nature of the procedure and the level of discomfort patients may experience. Our goal is to provide a clear and compassionate guide to help you navigate this complex topic.
Key Takeaways
- Understanding the stent procedure and its implications.
- What to expect during and after stent placement.
- The role of a coronary stent in treating coronary artery disease.
- Advancements in cardiac stent technology.
- Patient experiences and pain management during recovery.
Understanding Heart Stents and Their Purpose
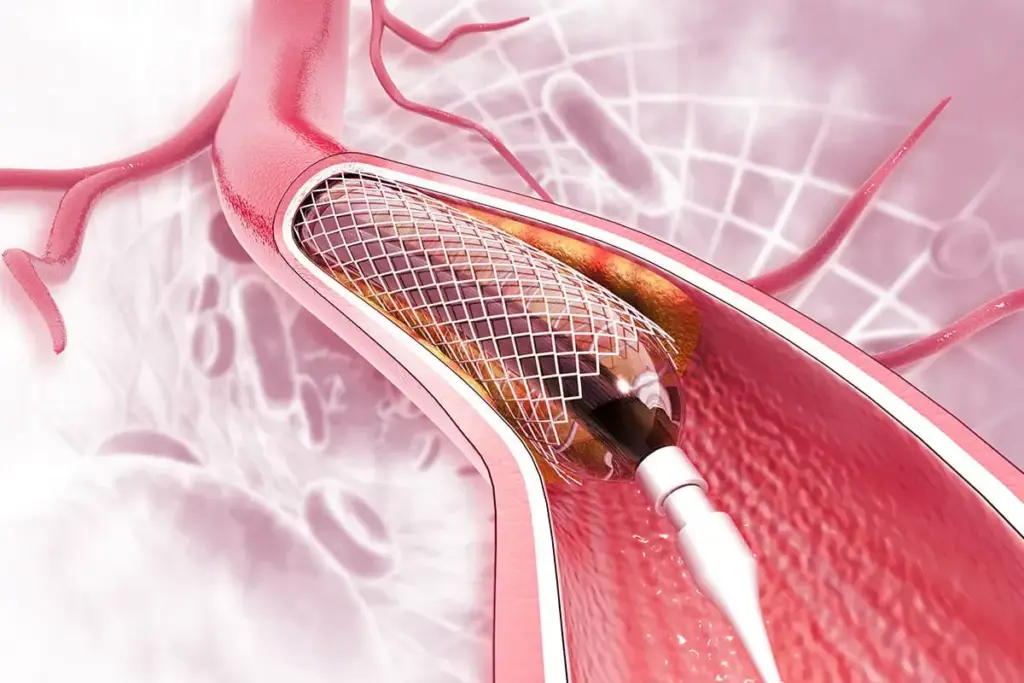
Heart stents are small, mesh tubes used to treat narrowed or blocked arteries. They play a key role in keeping the heart’s blood flow healthy. This ensures that blood reaches the heart without issues.
Plaque buildup in arteries, known as atherosclerosis, can cause serious problems like coronary artery disease. Heart stents are used to keep arteries open. This helps prevent heart attacks and other heart problems.
What is a Heart Stent?
A heart stent is a tiny, expandable tube made of metal mesh. It’s designed to be inserted into a narrowed or blocked artery. This helps restore blood flow. The stent is placed during a minimally invasive procedure called angioplasty.
Why Heart Stents Are Needed
Heart stents are needed to treat conditions like coronary artery disease and atherosclerosis. They keep arteries open, which helps in several ways:
- Improves blood flow to the heart muscle
- Reduces symptoms of angina and shortness of breath
- Lowers the risk of heart attacks
Types of Coronary Stents Available
There are several types of coronary stents available, each with its own unique characteristics:
- Bare-metal stents: These are the original type of stent and are made of metal mesh.
- Drug-eluting stents: These stents are coated with medication that helps prevent the artery from narrowing again.
- Bioresorbable stents: These stents are made of materials that dissolve over time, reducing the risk of long-term complications.
Understanding the different types of stents can help patients make informed decisions about their treatment options.
Conditions That Require Heart Stent Placement

Doctors decide to use heart stents for certain heart problems, like coronary artery disease. This procedure is key to getting blood to the heart again. It helps ease symptoms and can save lives.
Coronary Artery Disease
Coronary artery disease (CAD) is a main reason for heart stent use. It happens when the heart’s blood supply arteries get narrowed or blocked. This can cause chest pain, shortness of breath, or even a heart attack.
Medicines like rosuvastatin calcium and atorvastatin calcium help manage CAD. They lower cholesterol and slow plaque buildup.
Atherosclerosis and Plaque Buildup
Atherosclerosis is what causes CAD. It’s when plaque, made of fat, cholesterol, and more, builds up in arteries. This can harden or rupture, causing a blockage and heart attack risk.
Plaque buildup happens over time. High cholesterol, smoking, and high blood pressure are key factors.
Acute Coronary Syndromes
Acute coronary syndromes (ACS) are sudden heart blood flow issues. They include heart attacks and unstable angina. Heart stent placement is often urgent for heart attacks, to get blood flowing again.
Knowing what causes heart attacks is key to preventing and treating them. Heart attacks happen when blood flow to the heart is blocked, damaging or killing heart muscle.
Pre-Procedure Pain and Discomfort
Many people worry about pain and discomfort before heart stent surgery. It’s important to know what to expect.
Symptoms Before Stent Placement
Before heart stent surgery, patients may feel several symptoms. These include:
- Chest pain or discomfort, known as angina
- Shortness of breath
- Fatigue
- Dizziness or lightheadedness
These symptoms happen when the heart’s arteries get narrow or blocked. This is often due to atherosclerosis or plaque buildup.
Angina and Chest Pain
Angina is chest pain or discomfort when the heart doesn’t get enough oxygen. It feels like a squeeze or pressure in the chest.
Angina can start with physical activity or stress. It usually goes away with rest or medicine. Knowing about angina helps manage symptoms before surgery.
Differentiating Cardiac Pain from Other Types
Not all chest pain is heart-related. It’s key to tell the difference for the right treatment.
Cardiac pain, like angina, has specific signs. These include:
- A squeezing or heavy feeling in the chest
- Pain that spreads to the arms, back, neck, jaw, or stomach
- Discomfort that gets worse with activity and eases with rest
Medicines like Lipitor (atorvastatin) help control cholesterol. They lower heart disease risk. Knowing what is atorvastatin used for helps manage heart health.
Preparing for Heart Stent Surgery
Getting ready for heart stent surgery is key to a good outcome. We’ll help you with medical checks, adjusting meds, and what to do right before surgery.
Medical Evaluations and Tests
We do many tests before your surgery to check your health and heart. These include:
- Blood tests to find any health issues or risks.
- Electrocardiogram (ECG) to see how your heart’s electrical system works.
- Echocardiogram to look at your heart’s shape and how it works.
- Stress test to see how your heart does under stress.
- Coronary angiography to see blockages in your heart’s arteries.
These tests help us understand your heart and plan your stent placement.
Medication Adjustments
We often need to change your meds before surgery. You might need to:
- Keep taking meds like rosuvastatin 10 mg to lower cholesterol.
- Stop some meds that could mess with the surgery or increase bleeding risk.
- Change the dose of some meds to keep you safe during the surgery.
It’s important to follow our advice on meds to reduce risks and get the best results. If you’re on rosuvastatin, knowing what is rosuvastatin used for helps you understand its role in your care.
What to Expect Before the Procedure
Before your surgery, we’ll give you detailed instructions. This includes:
- Fasting for a set time before the surgery.
- Avoiding certain foods or drinks that could affect the surgery.
- Arranging for someone to drive you home after the surgery.
- Following any special pre-surgery routines we suggest.
By following these steps, you can help make your heart stent surgery go smoothly and successfully.
The Heart Stent Procedure Explained
Angioplasty and stent placement are common in cardiology, helping those with coronary artery disease. Many patients feel anxious about these procedures. We’ll explain the process, including angioplasty and stent placement, how long it takes, and the anesthesia used.
Angioplasty and Stent Placement Process
The procedure has two main steps: angioplasty and stent placement. Angioplasty uses a balloon to widen a blocked artery. A thin, flexible tube guides the balloon, which inflates to push plaque against the artery walls, improving blood flow.
After angioplasty, a stent is placed to keep the artery open. The stent is a small, mesh-like tube that expands at the blockage site. There are different stents, like bare-metal and drug-eluting stents, which release medication to prevent re-narrowing.
Duration of the Procedure
The procedure’s length varies, usually taking 30 minutes to a few hours. It depends on the blockage’s complexity and the number of stents. We aim to complete it efficiently.
Types of Anesthesia Used
Local anesthesia numbs the area where the catheter is inserted, often in the groin or arm. This reduces discomfort during the procedure. Conscious sedation may also be used to relax the patient. It keeps the patient awake but calm.
Using local anesthesia and conscious sedation makes the procedure more comfortable. We’ll discuss anesthesia with you beforehand to address any concerns.
- Key aspects of the procedure include:
- Minimally invasive technique
- Use of local anesthesia and conscious sedation
- Angioplasty to widen the blocked artery
- Stent placement to keep the artery open
Understanding the heart stent procedure helps patients prepare, reducing anxiety and improving their experience.
Pain Levels During Heart Stent Surgery
The feeling of pain during heart stent surgery depends on several factors. These include the use of local anesthesia and conscious sedation. These methods are key in reducing pain during the procedure.
Local Anesthesia and Conscious Sedation Effects
Local anesthesia numbs the area where the catheter is inserted. This is usually in the groin or arm. It makes sure patients don’t feel pain in the procedure area.
Conscious sedation helps patients relax and feel more at ease during surgery. It doesn’t make patients unconscious but keeps them calm and relaxed.
Sensations During Catheter Insertion
When the catheter is inserted, patients might feel a slight pinch or pressure. This is usually mild and short-lived. The use of local anesthesia helps reduce any discomfort from this step.
Discomfort During Balloon Inflation
When the balloon inflates to open the blocked artery, some might feel pressure or discomfort in the chest. This is often described as a tight feeling, not pain. The feeling is usually brief and goes away once the balloon is deflated.
What Most Patients Actually Feel
Most patients say they feel little to no pain during the surgery. The mix of local anesthesia and conscious sedation helps manage pain well. While experiences can vary, most agree the procedure is tolerable.
Is Heart Stent Surgery Painful? The Truth About Discomfort Levels
When you think about heart stent surgery, knowing how much pain it causes is key. This surgery is lifesaving but can make you worry about pain. We’ll look at how much pain people feel, compare what they expect to what they actually feel, and talk about what affects pain during the surgery.
Pain Scale Assessment
Doctors use a pain scale to measure pain. It goes from 0 to 10, with 0 being no pain and 10 being the worst. Most people say their pain is between 2 and 4 during the surgery, which is mild.
“The pain scale is a valuable tool for us to understand the patient’s experience,” says a cardiologist. “It helps us tailor our approach to pain management, ensuring that our patients receive the most appropriate care.”
Comparing Expected vs. Actual Pain
People often worry about how much pain they’ll feel during heart stent surgery. But, most people don’t feel as much pain as they think. This is because of local anesthesia and conscious sedation.
A study in the Journal of Cardiology found that most patients felt less pain than they thought. This shows how important it is to educate patients and manage their expectations.
Factors That Influence Pain Perception
Many things can change how much pain someone feels during heart stent surgery. These include:
- Anxiety Levels: More anxiety can make pain feel worse.
- Pain Tolerance: People who can handle more pain might feel less discomfort.
- Effectiveness of Anesthesia: The skill of the doctor and the type of anesthesia used can greatly affect pain levels.
- Patient Health: Your overall health and any other medical conditions can also change how you feel pain.
Knowing these factors helps doctors manage pain better. This makes the experience of heart stent surgery better for patients.
Immediate Post-Procedure Pain
After heart stent surgery, patients often wonder about pain during the first few days. This time is key for watching and handling any pain.
Recovery Room Experience
After the surgery, patients go to the recovery room. Here, doctors watch their vital signs and check for pain. “The recovery room experience can vary,” says a cardiologist. “Some feel tired, while others might have some pain at the insertion site.”
Many patients worry about the recovery room. But our team works hard to make your stay comfortable. We keep a close eye on you and adjust our care to ease any discomfort.
Common Discomfort at the Insertion Site
Discomfort often happens at the site where the catheter was put in. This can feel like a bruise or be more painful. It depends on the person and the procedure.
|
Symptom |
Frequency |
Typical Duration |
|---|---|---|
|
Bruising |
Common |
1-2 weeks |
|
Soreness |
Very Common |
1-7 days |
|
Swelling |
Occasional |
1-5 days |
Chest Sensations After Stent Placement
Some people feel chest sensations after the stent is placed. These can be mild or feel like tightness. It’s important to know the difference between normal feelings and signs of trouble.
Always follow your doctor’s advice and report any unusual or severe symptoms. While some pain is okay, some symptoms need quick medical help.
Knowing about immediate pain and discomfort can help ease worries. Being informed and ready can make this important time easier and more comfortable.
Pain Management After Heart Stent Surgery
Patients who have had heart stent surgery need a variety of ways to manage pain. It’s key for a smooth recovery and to reduce discomfort.
Medications for Pain Relief
Doctors often give patients medicines to help with pain after surgery. These can include pain relievers like acetaminophen or ibuprofen. They also give antiplatelet drugs to stop blood clots. It’s important to take these medicines as directed by your doctor.
Non-Pharmaceutical Pain Management Techniques
There are also non-medical ways to manage pain after heart stent surgery. Deep breathing, progressive muscle relaxation, and guided imagery can help.
|
Technique |
Description |
Benefits |
|---|---|---|
|
Deep Breathing Exercises |
Slow, deep breaths to relax the body |
Reduces stress and anxiety |
|
Progressive Muscle Relaxation |
Tensing and relaxing different muscle groups |
Relieves physical tension |
|
Guided Imagery |
Focusing on positive, calming images |
Distracts from pain and promotes relaxation |
When to Contact Your Doctor About Pain
Some pain is normal after heart stent surgery. But, there are times when you should call your doctor. If the pain is very bad or getting worse, or if you have other symptoms like trouble breathing or feeling dizzy, get help right away. Also, if you have any side effects from your medicines, talk to your doctor.
Recovery Timeline and Pain Expectations
Knowing how long it takes to recover after heart stent surgery is key to managing pain. The recovery time can vary, but there are general guidelines to help you prepare.
First 24 Hours After the Procedure
The first 24 hours after heart stent surgery are very important. Most patients stay in the hospital for a few hours after the procedure. They might go home the same day or stay overnight for more observation.
You might feel some pain or discomfort at the catheter site. This can be managed with pain medicine. It’s important to rest and avoid hard activities during this time. Your doctor will tell you how to care for the site and what activities to avoid.
First Week of Recovery
In the first week, you might feel some pain or discomfort, but it should get better. You might feel tired and weak, but this should improve as the week goes on.
You can start doing light activities a few days after. But, it’s important to listen to your doctor about when to start doing harder activities or exercising. Paying attention to how your body feels and adjusting your activities is key to a smooth recovery.
|
Recovery Stage |
Expected Pain/Discomfort |
Activities |
|---|---|---|
|
First 24 Hours |
Moderate pain at insertion site |
Rest, avoid strenuous activities |
|
First Week |
Mild to moderate discomfort |
Gradually resume light activities |
|
Long-term |
Minimal to no pain |
Resume normal activities, including exercise |
Long-Term Recovery and Pain Resolution
In the long term, most people see a big improvement in their symptoms and less pain. The stent keeps the artery open, improving blood flow to the heart.
It’s important to live a heart-healthy lifestyle. This includes eating well, exercising regularly, and taking your medicine as directed. This helps support your long-term recovery and heart health.
Potential Complications and Associated Pain
It’s important to know about the possible problems with heart stent surgery. The procedure is usually safe, but knowing about risks helps. Being informed is key.
Stent Restenosis
Stent restenosis is when the artery gets narrow again after a stent is placed. This can cause angina or chest pain to come back. It happens because new tissue grows inside the stent.
Doctors say the chance of restenosis depends on the stent type. Drug-eluting stents, for example, lower this risk more than bare-metal stents.
Blood Clots and Stent Thrombosis
Blood clots and stent thrombosis are serious issues after stent placement. Stent thrombosis is when a clot forms inside the stent, which can cause a heart attack. This risk is higher in the first few months.
- Symptoms of stent thrombosis include sudden chest pain and shortness of breath.
- Immediate medical attention is required if these symptoms occur.
Allergic Reactions to Stent Materials
Some people might have allergic reactions to stent materials. Symptoms can be mild, like skin irritation, or severe. It’s important to tell your doctor about any allergies before the procedure.
Bleeding or Vascular Complications
Bleeding or vascular problems can happen at the catheter site or inside. These can cause pain, swelling, or bruising. Sometimes, more procedures are needed to fix these issues.
Knowing about these risks and talking to your doctor can help manage them. This ensures the best outcome for you.
Living with a Heart Stent
Having a heart stent means making big changes in your life. You’ll need to adjust your daily habits to keep the stent working right. This helps keep your heart healthy too.
Long-Term Lifestyle Adjustments
Life with a heart stent means eating better and quitting smoking. You’ll also need to find ways to handle stress. Eating foods like fruits, veggies, whole grains, and lean meats is key. Try to cut down on fats, cholesterol, and salt too.
Managing stress is important. Try meditation, yoga, or deep breathing to calm down. Don’t forget to see your doctor regularly. They’ll check how the stent is doing and your heart health.
Key Lifestyle Adjustments:
- Eat a heart-healthy diet
- Stop smoking
- Find ways to manage stress
- Go to regular health check-ups
Ongoing Medication Requirements
People with heart stents often take medicines to stop blood clots. It’s very important to take these medicines as told. This keeps the stent safe and your heart healthy.
“Taking antiplatelet medicines is key in the first year after getting a stent. It really lowers the chance of stent problems.” – American Heart Association
If you have any worries or side effects, talk to your doctor. They can help with any issues and change your medicine if needed.
|
Medication Type |
Purpose |
Duration |
|---|---|---|
|
Antiplatelet |
Prevent blood clots on the stent |
At least 12 months |
|
Statins |
Lower cholesterol levels |
Ongoing |
|
Beta-blockers |
Reduce heart workload |
Varies |
Physical Activity and Exercise Recommendations
It’s good to stay active with a heart stent. But start slow and don’t push too hard too soon.
Talk to your doctor before starting any new exercise. They can give advice that fits your health and needs.
- Start with easy activities like walking or stretching.
- Slowly make your exercises harder and longer.
- Avoid lifting heavy or bending a lot.
By making these lifestyle changes and following your doctor’s advice, you can live a healthy and active life with a heart stent.
Patient Experiences with Heart Stent Pain
Patients who have had heart stent surgery share a common hope and recovery story. Heart stent surgery is a big medical step. Hearing from others can help those getting ready for it.
Real-Life Testimonials
Many patients have shared their heart stent surgery stories. They talk about pain and getting better. For example, a patient, 55, said he felt little pain during the surgery and was back to normal in a week. His story shows how important it is to get care that fits you.
A patient, 62, talked about some chest pain after her surgery. But with medicine and rest, she felt better. Her experience shows how important it is to follow doctor’s orders and ask for help when you need it.
Variations in Pain Perception
Pain levels can differ a lot for people getting heart stents. Things like how much pain you can handle, your health, and the surgery details can affect your pain.
Some might feel only a little pain, while others might feel more. It’s key for doctors to understand these differences to help each patient better.
Coping Strategies from Former Patients
People who’ve had heart stents often find ways to deal with pain and getting better. They stick to their medicine, change their lifestyle, and get help from doctors and family.
- Eating healthy and exercising
- Taking all medicine as prescribed
- Keeping in touch with doctors for advice and support
By sharing their experiences and tips, patients help others who are about to have heart stent surgery.
Conclusion
It’s important for patients to know about heart stent surgery and its pain levels. We’ve looked at the different types of stents and when they’re used. We also talked about the pain people feel during and after the surgery.
We discussed how to recover and manage pain after the surgery. Following the doctor’s instructions is key to feeling better and recovering well. Most people find the pain after heart stent surgery to be manageable.
Knowing what to expect during and after stent placement helps patients prepare. It also helps them make better choices about their care. Our aim is to support and guide patients through the whole process, ensuring they get the best care for heart stent surgery.
FAQ
What is a heart stent and why is it used?
A heart stent is a small, mesh-like device. It keeps the coronary arteries open. This improves blood flow to the heart. It’s mainly used to treat coronary artery disease.
How painful is heart stent surgery?
Most patients feel little pain during the procedure. This is because of local anesthesia and conscious sedation. Some might feel discomfort when the catheter is inserted or the balloon is inflated.
What are the common symptoms before stent placement?
Symptoms include angina, chest pain, and shortness of breath. These happen because of reduced blood flow to the heart. This is often due to coronary artery disease or other conditions.
How long does the heart stent procedure take?
The procedure itself takes about 30 minutes to an hour. But, getting ready and recovering can take several hours in total.
What type of anesthesia is used during heart stent surgery?
Local anesthesia numbs the area where the catheter is inserted. Conscious sedation helps the patient relax during the procedure.
What are the possible complications of heart stent surgery?
Complications can include stent restenosis, blood clots, and allergic reactions to stent materials. There’s also a risk of bleeding or vascular complications.
How is pain managed after heart stent surgery?
Pain is managed with medications and non-pharmaceutical techniques. Patients should contact their doctor if they have severe or persistent pain.
What is the recovery timeline after heart stent surgery?
Most patients can get back to normal activities in a few days to a week. Full recovery usually takes a few weeks.
Are there any long-term lifestyle adjustments needed after getting a heart stent?
Yes, patients are often advised to make lifestyle changes. This includes dietary adjustments, increased physical activity, and quitting smoking to keep their heart healthy.
Can I exercise with a heart stent?
Yes, regular exercise is encouraged. But, it’s important to follow your healthcare provider’s specific recommendations. This ensures safety and effectiveness.
What medications are required after heart stent surgery?
Patients are usually prescribed antiplatelet medications to prevent blood clots. They may also need medications to manage conditions like high cholesterol or hypertension.
How do I know if my stent is working properly?
Your healthcare provider will check your condition through follow-up appointments and tests. This ensures the stent is working right and there are no complications.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/11867031/





