
Nearly 1 million Americans get stent placement each year to clear blocked arteries. But, many ask: how fast can arteries clog again after this?
We get your worry. After a stent is put in, keeping your heart health is key. How fast arteries clog again can vary a lot. It depends on things like your lifestyle, other health issues, and following care advice after the procedure.
We aim to help you understand what happens after stent placement. We’ll also show you how to lower the chance of artery clogging.
What Are the Symptoms of a Blocked Stent?What is a stent clog risk? It can happen fast if meds are skipped. Get best risk facts. Medication is vital to prevent dangerous issues.
Key Takeaways
- Understanding the process and risks associated with stent placement.
- Factors influencing artery clogging after stent placement.
- The importance of post-procedure care for maintaining heart health.
- Lifestyle changes that can reduce the risk of artery clogging.
- Monitoring and follow-up care after stent placement.
What Is a Stent and How Does It Work?

It’s important to know what a stent is and how it works for those having heart procedures. We’ll cover what stents are, their role in fixing blocked arteries, and the latest in stent technology.
Definition and Basic Function of Stents
A stent is a small, mesh-like device that keeps arteries open. It’s made of metal or a polymer and supports artery walls narrowed or blocked by plaque.
The stent’s main job is to ensure blood flows to the heart muscle by keeping the artery open. This is done by placing the stent at the blockage site through a catheter. The stent then expands to support the artery walls.
How Stents Help Treat Arterial Blockages
Stents treat arterial blockages by supporting the artery walls, improving blood flow. They’re key in treating coronary artery disease, which can cause heart attacks.
Stents are a common choice in cardiology, a less invasive option than surgery. They help reduce symptoms of angina and boost heart function.
The Evolution of Stent Technology
Stent technology has greatly improved over time. First, bare metal stents were used but had a high restenosis rate. Then, drug-eluting stents were developed to prevent cell growth and reduce restenosis risk.
Recently, bioresorbable vascular scaffolds (BVS) have been introduced. They provide temporary support and then dissolve, aiming to lessen long-term stent complications.
|
Type of Stent |
Description |
Advantages |
|---|---|---|
|
Bare Metal Stents (BMS) |
Made of metal mesh |
Simple design, less expensive |
|
Drug-Eluting Stents (DES) |
Release medication to prevent restenosis |
Reduced risk of restenosis compared to BMS |
|
Bioresorbable Vascular Scaffolds (BVS) |
Temporary support, dissolves over time |
Potential reduction in long-term complications |
We’ve seen big leaps in stent technology, from bare metal to drug-eluting stents and now bioresorbable scaffolds. Each new type has improved patient results and cut down on complications.
The Process of Stent Placement
For many, the stent placement procedure is a lifesaver. It requires careful medical care. Knowing the steps involved can ease worries and prepare patients for what’s ahead.
Preparation for Stent Procedure
Before the stent placement, patients get tested to check their heart health. They might have blood tests, electrocardiograms, and imaging studies like angiograms.
It’s important to tell doctors about any medicines taken. Some might need to stop or change before the procedure. Patients are usually told not to eat or drink for a while before the stent placement.
“The key to a successful stent placement is thorough preparation and a well-coordinated care team,” says a leading cardiologist.
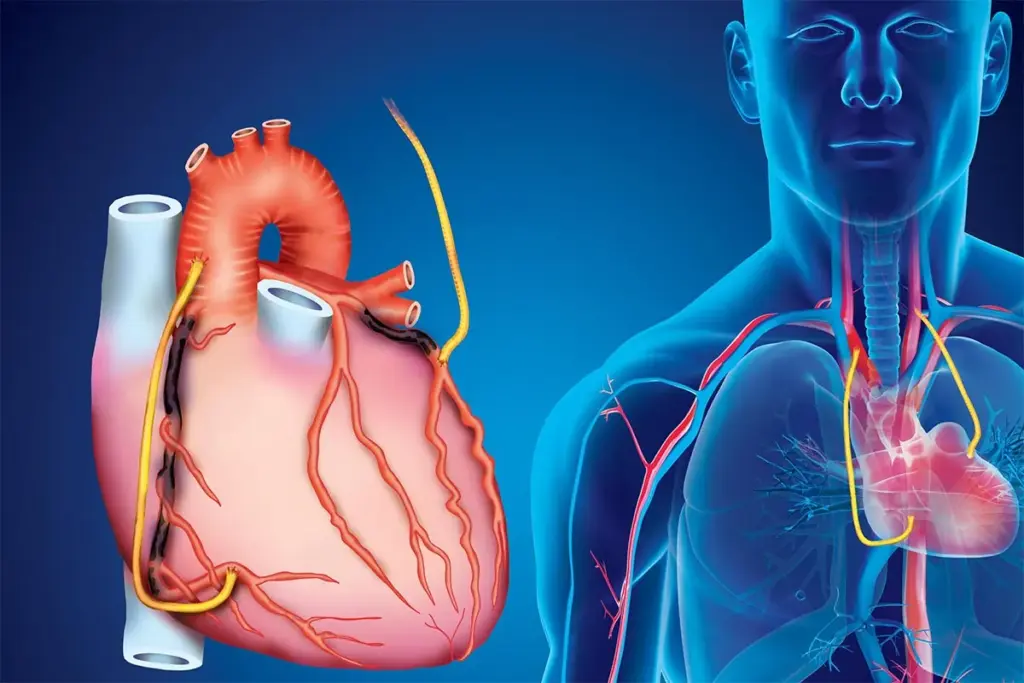
Step-by-Step Explanation of Stent Insertion
The stent placement procedure has several steps:
- Administering local anesthesia to numb the area where the catheter will be inserted.
- Inserting a catheter (a thin, flexible tube) into an artery in the leg or arm.
- Guiding the catheter to the blocked artery using X-ray imaging.
- Inflating a balloon to widen the artery, a process known as angioplasty.
- Deploying the stent to keep the artery open.
- Removing the catheter and closing the insertion site.
Immediate Post-Procedure Care
After the stent placement, patients are watched in a recovery area for hours. Medical staff check for any immediate problems and make sure the patient is okay.
Some patients might wear a Holter monitor for 24 to 48 hours. This tracks heart activity to catch any rhythm issues after the procedure.
|
Care Aspect |
Description |
Importance |
|---|---|---|
|
Monitoring |
Close observation for complications |
High |
|
Medication |
Adherence to antiplatelet therapy |
Critical |
|
Follow-up |
Scheduled check-ups with healthcare provider |
Essential |
Understanding stent placement and following care instructions can greatly improve outcomes. It also lowers the risk of complications.
Different Types of Stents Used in Modern Medicine
Modern medicine uses many stents to fix blocked arteries. Each stent is special and works in its own way. Thanks to new stent technology, patients with heart disease get better care.
Bare Metal Stents (BMS)
Bare Metal Stents (BMS) were the first stents used in heart procedures. They are made of metal and keep the artery open. But, they can cause more problems than newer stents.
Drug-Eluting Stents (DES)
Drug-Eluting Stents (DES) release medicine that stops cells from growing. This helps prevent blockages from coming back. Doctors often choose DES because they work better than BMS.
Bioresorbable Vascular Scaffolds (BVS)
Bioresorbable Vascular Scaffolds (BVS) break down over time. They might be better for people who can’t handle metal stents. BVS could lead to fewer long-term problems.
Specialized Stents for Specific Conditions
There are stents for different needs, like those for leg artery disease. Some stents have special coatings to help them work better. These stents are made just for certain patients.
|
Stent Type |
Key Features |
Restenosis Risk |
|---|---|---|
|
Bare Metal Stents (BMS) |
Metal mesh scaffold |
Higher |
|
Drug-Eluting Stents (DES) |
Releases medication to prevent cell proliferation |
Lower |
|
Bioresorbable Vascular Scaffolds (BVS) |
Dissolves over time |
Variable, potentially lower long-term |
The Timeline of Healing After Stent Placement
Knowing how long it takes to heal after a stent is placed is key. It affects how well you feel and your overall health. The healing process has many stages, from right after the procedure to when the stent fully integrates into your body.
First Few Days Post-Procedure
The first days after getting a stent are very important. Doctors watch for any problems and give you medicine to stop clots and help you heal. It’s vital to do exactly what your doctor tells you to do.
Weeks 1-4: Initial Healing Phase
In the first month, your body starts to heal around the stent. You’ll see less swelling and the endothelialization process begins. This is when the inside of your artery starts to grow over the stent. You might need to keep taking dual antiplatelet therapy to avoid clots.
Months 1-6: Endothelialization Process
The endothelialization process keeps going, making the stent part of your artery wall. By six months, the stent is fully covered by new tissue, lowering clot risk. It’s important to see your doctor regularly during this time to check on your healing.
Long-term Integration of the Stent
As time goes on, the stent becomes a permanent part of your artery. The chance of problems goes down, but it’s important to keep a heart-healthy lifestyle and take your medicine. Regular doctor visits are key to keeping an eye on your stent and heart health.
By sticking to the healing timeline, you can greatly improve your recovery after a stent. It’s a journey that needs patience, following doctor’s orders, and caring for your heart health.
What Is Restenosis? Understanding Artery Re-clogging
Restenosis is when arteries clog again after a stent is placed. This can lead to symptoms coming back or even worse heart problems.
Definition and Mechanisms
Restenosis happens when a stented artery gets narrow again. It’s because the body reacts to the stent by growing new tissue. This new tissue can block the artery.
Understanding how restenosis works is key to finding ways to stop it.
Difference Between Restenosis and Original Blockage
Restenosis and the original blockage are different. The original blockage is usually from plaque buildup. Restenosis is caused by the body’s reaction to the stent. Knowing these differences helps doctors choose the right treatment.
How Common Is Restenosis After Stenting?
How often restenosis happens depends on many things. These include the type of stent, the patient’s health, and the complexity of the blockage. Thanks to new stent technology, restenosis is less common. But it’s a worry, mainly for certain patients.
Patients with diabetes or complex blockages face a higher risk. Using smaller stents also increases the risk. Regular check-ups are key to managing and preventing restenosis.
In short, restenosis is a big deal after stent placement. Knowing what it is, how it happens, and how common it is helps doctors give better care. By understanding the differences and what affects it, we can improve treatment plans and outcomes for patients.
How Quickly Can Arteries Clog After a Stent?
Knowing when arteries might clog after a stent is key for good care and safety. Stent thrombosis, where a clot forms in the stent, can happen at different times. We’ll look at the types and when they happen to help understand this important issue.
Acute Stent Thrombosis (Within 24 Hours)
Acute stent thrombosis happens in the first 24 hours after a stent is put in. This time is very risky because of the trauma from the procedure and the body’s reaction. Quick medical help is needed if you have chest pain or trouble breathing.
Subacute Stent Thrombosis (24 Hours to 30 Days)
Subacute stent thrombosis occurs between 24 hours and 30 days after stenting. The risk of clotting is high during this time, mainly if you don’t take your medicine as told. It’s important to stick to your medication to avoid clots.
Late Stent Thrombosis (30 Days to 1 Year)
Late stent thrombosis happens between 30 days and 1 year after stenting. The risk is lower, but it’s not gone. Problems with the stent or medicine can cause it.
Very Late Stent Thrombosis (Beyond 1 Year)
Very late stent thrombosis is a worry after the first year. It can be caused by the stent not fully healing or by stent material issues. Keeping up with long-term care is important to avoid this.
In summary, knowing the timing of stent thrombosis is vital for both patients and doctors. By understanding the risks at each stage, we can work to prevent problems and get the best results for those with stents.
Risk Factors That Accelerate Artery Re-clogging
It’s important to know what can cause arteries to clog again after a stent is placed. This problem, called restenosis, can make stenting less effective over time.
Patient-Related Risk Factors
There are several things about a patient that can raise the risk of artery clogging. These include:
- Diabetes: People with diabetes face a higher risk because of insulin resistance and inflammation.
- Smoking: Smoking speeds up the buildup of plaque in arteries and can cause stents to fail.
- High Blood Pressure: If blood pressure is not controlled, it can put extra stress on the stented artery.
- High Cholesterol: High levels of LDL cholesterol can help plaque build up.
|
Risk Factor |
Description |
Impact on Stent |
|---|---|---|
|
Diabetes |
Insulin resistance and inflammation |
Increased risk of restenosis |
|
Smoking |
Accelerates atherosclerosis |
Higher risk of stent failure |
|
High Blood Pressure |
Additional stress on stented artery |
Increased risk of complications |
Procedure-Related Risk Factors
Things related to the stenting procedure itself can also affect the risk of artery clogging. These include:
- Stent Type: The type of stent used, like bare-metal, drug-eluting, or bioresorbable vascular scaffolds, can impact how often restenosis happens.
- Stent Size and Placement: If the stent is not the right size or is not placed correctly, it may not expand enough or could harm the artery wall.
To lower the risk of artery clogging, it’s key to make lifestyle changes, take medications as directed, and have regular check-ups. This helps ensure the stent works well over time.
Signs and Symptoms of Stent Failure or Restenosis
Restenosis, or the re-narrowing of arteries after stenting, needs quick action if symptoms show up. After a stent is placed, it’s important to watch your health closely. Look out for warning signs that might mean the stent has failed or restenosis is happening.
Recurring Chest Pain or Angina
One key sign of possible stent failure is chest pain or angina coming back. This pain feels like pressure or discomfort in the chest. It might spread to the arms, back, neck, jaw, or stomach. If you feel this, you should get medical help right away.
Shortness of Breath and Fatigue
Feeling short of breath or unusually tired can also mean the stent isn’t working right. These symptoms happen because the heart isn’t getting enough blood. This can make you feel weaker and less able to do things.
When to Seek Emergency Medical Attention
If you have severe chest pain, trouble breathing, or other scary symptoms, get emergency help fast. Quick action can stop serious problems and help you get better. Don’t wait to get medical help if you’re feeling these signs.
Knowing these signs and symptoms helps you take care of your heart health. Make sure to see your doctor regularly and take your medicines as told. This helps keep your stent working well.
The Critical Role of Antiplatelet Therapy After Stenting
Stent placement is just the start. Antiplatelet therapy is key for long-term heart health. After a stent is put in, there’s a risk of clotting. So, antiplatelet therapy is vital for post-stenting care.
Dual Antiplatelet Therapy (DAPT) Explained
Dual Antiplatelet Therapy (DAPT) uses two drugs to stop clots on the stent. It usually includes aspirin and a P2Y12 inhibitor like clopidogrel or ticagrelor. These drugs work together to prevent platelets from sticking together, lowering the risk of stent thrombosis.
DAPT has been a game-changer for patients with coronary stents. It cuts down stent thrombosis and heart attacks. But, how long to use DAPT depends on the stent type.
Duration of Antiplatelet Therapy Based on Stent Type
The stent type affects how long you need to take antiplatelet therapy. For example, drug-eluting stents (DES) need longer DAPT than bare-metal stents (BMS). Guidelines suggest at least 6 months of DAPT for DES, and 1 month for BMS.
- Drug-Eluting Stents (DES): Need at least 6 months of DAPT.
- Bare-Metal Stents (BMS): Need at least 1 month of DAPT.
Risks of Premature Discontinuation
Stopping antiplatelet therapy too soon is risky. It can lead to stent thrombosis, a serious condition. Stopping early increases the risk of clots, heart attacks, or even death.
It’s important for patients to stick to their antiplatelet therapy. We advise talking to your healthcare provider about any concerns or questions.
Managing Antiplatelet Therapy Before Surgeries
Managing antiplatelet therapy before surgery is tricky. The risk of bleeding must be weighed against the risk of stent thrombosis. Often, we recommend keeping aspirin therapy going during surgery, for those at high risk.
Deciding to keep or stop antiplatelet therapy before surgery depends on many factors. These include the surgery type, patient risk factors, and time after stent placement.
In conclusion, antiplatelet therapy is vital after stenting. Understanding DAPT, its duration, and discontinuation risks helps manage heart health. This reduces the chance of complications.
Preventing Stent Failure and Artery Re-clogging
To prevent stent failure, we need to take several steps. This includes sticking to our medication and making lifestyle changes. Knowing what causes arteries to clog again helps us keep our stents healthy.
Medication Adherence and Management
It’s very important to take your medicine as told after getting a stent. Dual antiplatelet therapy (DAPT) is often used to stop blood clots. It’s key to take your meds on time and know the dangers of stopping too soon.
- Take medications at the same time every day to maintain consistency.
- Inform your healthcare provider about any side effects or concerns.
- Do not stop taking your medication without consulting your doctor.
Lifestyle Modifications for Stent Longevity
Changing our lifestyle helps keep stents working longer. Living a heart-healthy life lowers the chance of arteries clogging again.
- Eat a diet full of fruits, veggies, and whole grains.
- Do regular exercise like walking or biking.
- Stay away from smoking and drink less alcohol.
Regular Medical Follow-ups and Monitoring
Seeing your doctor regularly is key to keeping an eye on your stent. These visits help catch problems early and fix them fast.
- Schedule regular check-ups as recommended by your doctor.
- Report any new or worsening symptoms promptly.
- Do tests like stress tests or angiograms to check your stent.
By following your medicine, making healthy lifestyle choices, and going to regular doctor visits, you can lower the chance of stent failure. This ensures your stent works well for a long time.
Treatment Options When Arteries Re-clog After Stenting
When arteries re-clog after stenting, it’s a serious issue. We need a detailed plan to treat it. We look at many factors to find the best treatment.
Medication Adjustments
Medication adjustments are a key part of treatment. We might change the type or amount of antiplatelet drugs. This helps prevent more clots. We watch patients closely to make sure they get the right medicine.
Repeat Angioplasty and Re-stenting
In some cases, repeat angioplasty and re-stenting are needed. This involves using a balloon to open the artery again and possibly putting in a new stent. We decide on re-stenting based on how bad the clog is and the patient’s health.
Bypass Surgery Considerations
For severe or recurring clogs, bypass surgery might be an option. This surgery makes a new path for blood to flow. We check if surgery is right for each patient, looking at the benefits and risks.
|
Treatment Option |
Description |
Considerations |
|---|---|---|
|
Medication Adjustments |
Changing or adjusting antiplatelet medication |
Effective for preventing further clotting; requires close monitoring |
|
Repeat Angioplasty and Re-stenting |
Using a balloon to widen the artery and potentially placing a new stent |
Minimally invasive; suitable for many patients; may not be effective for complex blockages |
|
Bypass Surgery |
Creating a detour around the blocked artery |
More invasive; considered for complex or recurrent blockages; carries higher risks |
Advancements in Stent Technology to Reduce Re-clogging
The field of interventional cardiology has seen big steps forward in stent technology. This is to lower the chance of restenosis. As we learn more about coronary artery disease, new stent designs are key.
Comparison of Restenosis Rates Between Stent Types
Stents vary in how often they clog back up. Bare Metal Stents (BMS) clog more often than Drug-Eluting Stents (DES). DES releases medicine that stops cells from growing back, lowering clog rates.
|
Stent Type |
Restenosis Rate |
|---|---|
|
Bare Metal Stents (BMS) |
20-30% |
|
Drug-Eluting Stents (DES) |
5-10% |
|
Bioresorbable Vascular Scaffolds (BVS) |
10-15% |
As the table shows, DES have the lowest clog rates. They are often the first choice for many. But, the right stent depends on the patient’s health and the doctor’s advice.
Latest Innovations in Stent Design
New stent designs aim to improve how well they work and help patients more. For example, stents with bioabsorbable polymers or drug-eluting stents are showing great results.
“The future of stent technology lies in its ability to not only keep arteries open but to also promote healing and potentially restore normal vascular function.” – A Interventional Cardiologist
Future Directions in Stent Technology
Stent technology will keep getting better with new materials and bioengineering. Future stents might change shape, release more drugs, or even use stem cells to heal the blood vessels.
As we look to the future, working together is key. Doctors, researchers, and industry must team up to improve stent technology and care for patients.
Conclusion
Knowing how to care for your heart after a stent is key. We’ve covered the basics of stent placement. This includes the types of stents, how they’re placed, and the risks of artery clogging.
To keep your stent working well, follow your doctor’s advice. This means taking your meds, changing your lifestyle, and seeing your doctor often. A holter monitor might be used to check your heart’s rhythm. It’s also important to know the signs of stent problems.
By learning about stents and their role in your heart health, you can help your recovery. A good care plan is vital to avoid artery clogging. This ensures your stent works as it should.
FAQ
What is a stent and how does it work?
A stent is a small, mesh-like device. It’s inserted into a blocked or narrowed artery. This improves blood flow by keeping the artery open.
What are the different types of stents used in modern medicine?
There are several stent types, like bare metal stents and drug-eluting stents. Each has its own benefits and characteristics.
How long does it take for a stent to heal?
The healing process after stent placement takes several months. The first few days are critical. It’s important to follow a healthy lifestyle and medication regimen for proper healing.
What is restenosis, and how common is it after stenting?
Restenosis is when an artery narrows again after stenting. Its frequency depends on the stent type and patient factors.
What are the signs and symptoms of stent failure or restenosis?
Signs include recurring chest pain, shortness of breath, and fatigue. If you notice these, seek medical help right away.
How can I prevent stent failure and artery re-clogging?
To prevent stent failure, follow your medication, make healthy lifestyle choices, and attend regular check-ups.
What is the role of antiplatelet therapy after stenting?
Antiplatelet therapy prevents blood clots on the stent. The therapy duration depends on the stent type and patient factors.
Can I shower with a Holter monitor?
It’s generally advised to avoid showering with a Holter monitor. Water can damage it. But, newer models might be waterproof. Always check your doctor or the device’s instructions.
How does a Holter monitor work?
A Holter monitor is a portable device that records your heart’s activity for 24-48 hours. It tracks your heart rate and rhythm, helping diagnose and treat heart conditions.
What are the side effects of wearing a Holter monitor?
Some may experience minor skin irritation or discomfort from the electrodes. But, most people can wear a Holter monitor without major issues.
How long do I need to wear a Holter monitor?
The time varies based on your doctor’s instructions. It usually ranges from 24 to 48 hours, or sometimes up to 7-14 days.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3103652/








