
Coronary artery disease affects millions worldwide. The use of coronary stents is a common treatment. But is it considered a major surgery? We look into the facts to help you understand.
The stent procedure, also known as stent placement, is a minimally invasive treatment. It opens narrowed or blocked coronary arteries. Knowing if it’s a major surgery helps patients prepare for treatment and recovery.
Is a stent major surgery? No, it’s minor. Get best facts. It avoids dangerous chest cutting, offering an amazing and quick recovery path.
Key Takeaways
- The coronary stent procedure is generally not considered a major surgery due to its minimally invasive nature.
- It is used to treat coronary artery disease by opening blocked or narrowed arteries.
- The procedure involves the placement of a stent to keep the artery open.
- Recovery time is typically shorter compared to traditional open-heart surgery.
- Patients can usually resume normal activities within a few days.
What Are Coronary Stents and Their Purpose
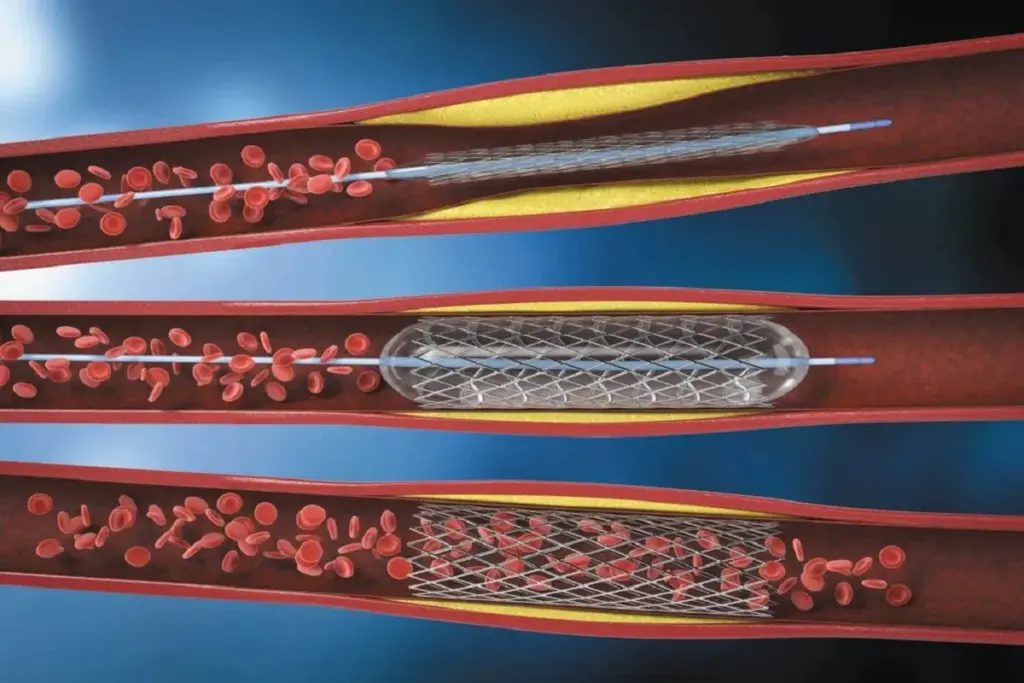
Coronary stents are small, mesh-like tubes that help restore blood flow to the heart. They are key in treating coronary artery disease. This disease clogs the heart’s main blood vessels with calcium and cholesterol.
Definition and Structure of Coronary Stents
A coronary stent is a tiny, expandable tube made of metal mesh. It’s used to open up narrowed or blocked arteries. The stent is on a balloon catheter, which expands it in the artery.
Types of Stents: Bare-Metal vs. Drug-Eluting
There are two main types of coronary stents: bare-metal and drug-eluting. Bare-metal stents are made of metal mesh and keep the artery open physically. Drug-eluting stents are coated with medication that prevents the artery from becoming blocked again.
Drug-eluting stents are often chosen because they lower the risk of in-stent restenosis. But, they require patients to take medication for longer than bare-metal stents.
How Stents Work to Improve Blood Flow
Coronary stents mechanically keep the artery open, improving blood flow. They relieve symptoms like chest pain and shortness of breath. By keeping the artery open, stents reduce heart attack risk and improve heart function.
The procedure to place a stent is done during a cardiac catheterization. The stent is delivered through a catheter in the leg or arm. After it’s expanded, the catheter is removed, leaving the stent to keep the artery open.
Coronary Stent Procedure: Is It Considered Major Surgery?
Understanding coronary stent procedures is key to knowing if they are major surgery. We need to look at what makes a surgery major or minor. Then, we can see how stent placement compares to more serious heart surgeries.
Defining Major vs. Minor Surgical Procedures
Surgeries are split into major and minor based on several things. These include how complex the surgery is, the risk involved, the damage to tissues, and how long it takes to recover. Major surgeries are risky, complex, and take a long time to get over. On the other hand, minor surgeries are less risky, simpler, and have quicker recovery times.
When we look at coronary stent procedures, we must think about these factors. The procedure uses a small incision in the arm or leg to place a stent in the artery. It’s less invasive, but we must consider the risks and complexity involved.
Classification of Stent Placement in Surgical Terms
Coronary stent placement is seen as a minimally invasive procedure. It doesn’t need to open the chest, unlike open-heart surgeries. The procedure uses local anesthesia and sometimes sedation, making it even less invasive.
- The procedure is usually done as an outpatient or with a short stay in the hospital.
- It causes little tissue damage.
- Most people can go back to normal activities in just a few days.
Comparison to Open Heart Procedures
Open-heart surgeries, like CABG, are major surgeries. They open the chest, stop the heart, and use a machine to keep blood flowing. These surgeries are very invasive, risky, and take a long time to recover from.
Coronary stent placement is less invasive and has fewer risks than open-heart surgeries. But, it’s not risk-free. Despite this, stent placement is seen as a minor surgery because it’s less invasive and has quicker recovery times.
In conclusion, while coronary stent procedures are serious, they are not considered major surgeries. This is because they are less invasive and have quicker recovery times.
The Complete Coronary Stent Procedure Explained
We will guide you through the coronary stent procedure, from preparation to post-procedure monitoring. Understanding each step can help alleviate anxiety and prepare you for what’s to come.
Pre-procedure Preparation and Testing
Before undergoing a coronary stent procedure, several tests and preparations are necessary. These include:
- Blood tests to check for any underlying conditions that could affect the procedure
- Electrocardiogram (ECG) to assess heart function
- Imaging tests such as angiography to visualize the coronary arteries
- Review of your medical history to identify any possible risks
It’s also important to tell your doctor about any medications you’re taking. Some may need to be adjusted or stopped before the procedure.
Step-by-Step Process During Stent Implantation
The coronary stent implantation process involves several key steps:
- Administration of local anesthesia to numb the area where the catheter will be inserted
- Insertion of a catheter through an artery in the groin or arm
- Guiding the catheter to the coronary artery using X-ray imaging
- Inflating a balloon to open the blocked artery, a process known as angioplasty
- Deployment of the stent to keep the artery open
Immediate Post-procedure Monitoring
After the stent implantation, you’ll be monitored in a recovery area for a few hours. During this time, medical staff will:
- Check for any complications or adverse reactions
- Monitor your vital signs, such as heart rate and blood pressure
- Keep you under observation for any signs of bleeding or other issues at the catheter insertion site
Most patients can go home the same day or the following day, depending on their condition and the doctor’s assessment.
|
Procedure Step |
Description |
Key Considerations |
|---|---|---|
|
Pre-procedure Testing |
Blood tests, ECG, imaging tests |
Identifying possible risks, assessing heart function |
|
Stent Implantation |
Catheter insertion, angioplasty, stent deployment |
Precision in guiding the catheter, successful stent deployment |
|
Post-procedure Monitoring |
Vital sign monitoring, complication checks |
Ensuring patient stability, addressing any complications promptly |
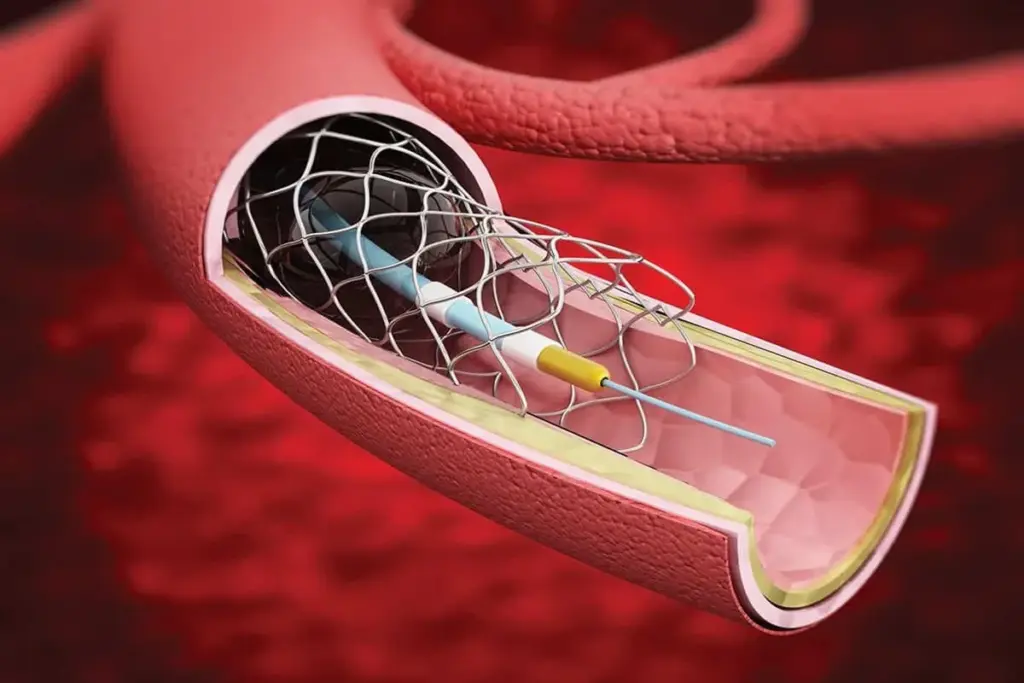
Cardiac Catheterization: The Gateway to Stent Placement
Cardiac catheterization is a key step before stent placement. It lets doctors see the coronary arteries. This is vital for finding out if you need a stent.
The Left Heart Catheterization Process
Left heart catheterization is a small procedure. A catheter is put through an artery in the wrist or groin. It goes to the left side of the heart. This helps us see the coronary arteries and check their health.
The process has several important steps:
- Preparing the access site by cleaning and numbing the area.
- Inserting a sheath into the artery, followed by a catheter.
- Guiding the catheter to the coronary arteries using X-ray imaging.
- Injecting contrast dye to visualize the coronary arteries.
Diagnostic Angiography Before Stenting
Diagnostic angiography is done during left heart catheterization. We use contrast dye to see the coronary arteries. X-ray imaging helps us spot any blockages or narrowings.
Interpreting Coronary Angiogram Results
Understanding coronary angiogram results is key. We look at the images to see how bad any blockages are. This helps us decide if you need a stent.
|
Angiogram Result |
Interpretation |
Typical Action |
|---|---|---|
|
Normal or mild disease |
Little to no blockage |
Medical management or lifestyle changes |
|
Moderate disease |
Some blockage, not severe |
Further evaluation or medical management |
|
Severe disease |
Significant blockage |
Stent placement or CABG |
By understanding the angiogram results, we can make the best treatment plan. This includes deciding if you need a stent.
Understanding Right Heart Catheterization (RHC)
Right Heart Catheterization (RHC) is key for diagnosing and managing heart issues. It’s a detailed procedure that checks the heart’s right side. This helps doctors understand how well the heart is working.
Purpose and Indications for RHC
The main goal of RHC is to see if the heart can pump blood well. It also checks the heart’s chamber and pulmonary artery pressures. This test is for those with heart failure, high blood pressure in the lungs, or before surgery.
RHC helps diagnose and manage heart issues like high blood pressure in the lungs and heart failure. It gives doctors the info they need to decide on treatments, like medicines or other interventions.
Normal RHC Pressure Values and Interpretation
During RHC, doctors measure different pressures in the heart. These include right atrial, right ventricular, pulmonary artery, and pulmonary capillary wedge pressures. Knowing these RHC pressure values is key to understanding the test results.
Normal pressures are usually between 2-6 mmHg for the right atrium and under 20 mmHg for the pulmonary artery at rest. High pressures might show heart failure or high blood pressure in the lungs. Doctors look at these values along with the patient’s overall health.
Difference Between Left and Right Heart Catheterization
Left and right heart catheterizations are both used to check the heart. But they look at different parts. Left heart catheterization is used to see the coronary arteries and check the left ventricle, often during angiography.
Right Heart Catheterization looks at the right side of the heart. It measures pressures in the right atrium, right ventricle, and pulmonary artery. Knowing the differences helps doctors pick the right test for each patient.
Medical Conditions Requiring Coronary Stent Placement
Coronary stent placement is a lifesaving procedure for many patients with heart disease. We often recommend it for patients with specific cardiac issues. These issues significantly impact their quality of life.
Stable Coronary Artery Disease
Stable coronary artery disease (CAD) is a condition where the coronary arteries narrow due to plaque buildup. This narrowing can cause chest pain during physical activity or stress. Coronary stent placement is often considered for patients with stable CAD when medications alone are not enough.
The decision to proceed with stent placement in stable CAD involves several factors. These include the severity of symptoms, the extent of coronary artery narrowing, and the patient’s overall health. Diagnostic tests like stress tests and coronary angiography help determine the need for stent placement.
Acute Coronary Syndromes
Acute coronary syndromes (ACS) include myocardial infarction (heart attack) and unstable angina. These conditions occur when there’s a sudden reduction in blood flow to the heart. Emergency stent placement is a critical treatment for ACS, aiming to restore blood flow to the affected heart muscle.
Timely intervention with stent placement can significantly improve outcomes in patients with ACS. The procedure helps to relieve the blockage, reduce damage to the heart muscle, and improve survival chances.
Recurrent Angina After Previous Interventions
Some patients may experience recurrent angina after previous coronary interventions, such as angioplasty or stent placement. This recurrence can be due to various factors, including in-stent restenosis (re-narrowing within the stent) or new blockages elsewhere in the coronary arteries. In such cases, further evaluation is necessary to determine the best course of action.
For patients with recurrent angina, additional stent placement or other interventions like coronary artery bypass grafting (CABG) may be considered. The choice of treatment depends on several factors, including the location and severity of the new blockage, the patient’s overall health, and previous treatment outcomes.
Let’s examine some key data related to coronary stent placement in various conditions:
|
Condition |
Primary Treatment Goal |
Role of Stent Placement |
|---|---|---|
|
Stable Coronary Artery Disease |
Manage symptoms, improve quality of life |
Relieve angina, improve exercise tolerance |
|
Acute Coronary Syndromes |
Restore blood flow, prevent further damage |
Emergency treatment to restore coronary blood flow |
|
Recurrent Angina After Previous Interventions |
Address underlying causes, relieve symptoms |
May be used to treat in-stent restenosis or new blockages |
Understanding these medical conditions and their treatment options is key for patients and healthcare providers. By recognizing the indications for coronary stent placement, individuals can make informed decisions about their care. This can potentially improve their outcomes.
The Minimally Invasive Nature of Stent Procedures
Stent procedures are a key way to treat coronary artery disease. They offer a safer option than traditional surgeries. We’ll look at why many patients choose stent placement.
Access Points: Radial vs. Femoral Approach
The way a stent is placed can affect the patient’s recovery. There are two main ways: radial and femoral arteries.
The radial approach, through the wrist, is popular for its lower risk of bleeding. It also makes post-procedure care easier. The femoral approach, through the groin, is used for more complex cases.
|
Characteristics |
Radial Approach |
Femoral Approach |
|---|---|---|
|
Bleeding Complications |
Lower risk |
Higher risk |
|
Post-procedure Care |
Easier mobilization |
Requires bed rest |
|
Complexity of Procedure |
Suitable for most cases |
Preferred for complex cases |
Limited Tissue Trauma Compared to Open Surgery
Stent procedures cause less tissue damage than open-heart surgery. This leads to less pain and a quicker recovery.
By making a small skin puncture, we reduce damage to the surrounding tissue. This lowers the risk of complications and speeds up healing.
Same-Day Discharge Possibilities
Stent procedures can allow for same-day discharge for many patients. This reduces healthcare costs and lets patients recover at home.
But, whether a patient can go home the same day depends on their health and the procedure’s complexity. Complications also play a role.
Recovery Timeline After Getting a Stent
Knowing the recovery timeline after a stent is key for patients. It helps them plan and care for their recovery. The time after a stent procedure is very important, and knowing what to expect is vital for a smooth recovery.
First 24-48 Hours Post-Procedure
The first 24 to 48 hours after a stent are watched closely by doctors. During this time, patients stay in the hospital for any immediate issues. “Rest is key in the first 24 hours,” says experts.
Patients should rest and avoid hard work, heavy lifting, and bending. It’s also important to watch for any signs of trouble, like chest pain or trouble breathing.
First Week of Recovery
In the first week, patients start to get back to normal activities with their doctor’s help. It’s important to take all medicines as directed, including dual antiplatelet therapy (DAPT), to stop clots on the stent.
Follow-up visits are set to check on recovery and answer any questions. Patients are also told about diet changes and lifestyle tips for heart health.
Long-term Recovery and Return to Activities
Long-term recovery means making lasting lifestyle changes and sticking to medication. Most people can get back to their usual activities in a few weeks. But, it’s important to listen to their doctor’s advice.
Regular check-ups are needed to see how the stent is working and to check heart health. A study found that “Lifestyle changes are key for long-term success with coronary stent placement.”
By following the recovery timeline, patients can get the best results from their stent. It’s a team effort between the patient and their healthcare team for the best outcome.
Benefits of Coronary Stent Treatment
Coronary stent treatment offers many benefits. It helps with both immediate symptoms and long-term heart health. Stents are key in managing coronary artery disease. They improve patients’ quality of life and lower the risk of future heart problems.
Immediate Symptom Relief
One big advantage of stent placement is quick relief from pain like angina or chest pain. Stents help blood flow to the heart muscle. This makes it easier for patients to do daily tasks without pain. Quick symptom relief is a key sign of a successful stent placement, helping patients get back to their usual activities fast.
Reduced Risk of Heart Attack
Stents are vital in lowering heart attack risk by keeping arteries open. Drug-eluting stents are very effective in stopping arteries from narrowing again. This is great for those with heart disease or at high risk.
Quality of Life Improvements
People who get stents often see big improvements in their life quality. They feel better, can move more, and live more actively. Patients’ overall well-being improves, letting them fully enjoy daily life and a better quality of life.
Comparison to Medical Therapy Alone
Stent treatment has clear advantages over just medicine. Medicine is important for heart disease, but stents offer quicker and more lasting relief. They also handle tough blockages that medicine can’t fix, giving a better treatment plan.
In summary, coronary stent treatment brings many benefits. It offers quick symptom relief, lowers heart attack risk, and boosts quality of life. Knowing these benefits helps patients and doctors choose the best treatment options.
Potential Risks and Complications of Stent Procedures
Coronary stenting is very effective, but it comes with risks. Like any medical treatment, there are possible complications during or after the procedure.
Procedural Complications
Problems during stent placement are rare but serious. These include:
- Arterial damage: The catheterization process can cause injury to the artery.
- Bleeding or hematoma: Bleeding at the catheter site or the formation of a hematoma can occur.
- Stroke or heart attack: Though rare, there’s a risk of stroke or heart attack during the procedure.
In-Stent Restenosis
In-stent restenosis is when the stented artery narrows again. This is more common with bare-metal stents than drug-eluting stents.
Factors increasing the risk of in-stent restenosis include diabetes, small stent size, and incomplete stent expansion.
Stent Thrombosis
Stent thrombosis is a serious issue where a blood clot forms inside the stent. This can cause a heart attack and is very dangerous.
- Acute stent thrombosis: Occurs within 24 hours of stent placement.
- Late stent thrombosis: Can occur months or even years after the procedure.
Bleeding Risks Related to Required Medications
Patients with coronary stents must take antiplatelet medications to prevent clots. But these medications can also increase the risk of bleeding.
Managing bleeding risks involves careful monitoring and possibly adjusting medication dosages.
Essential Medications After Coronary Stent Placement
After a coronary stent is placed, important medications are often given. These help the stent work right and aid in full recovery.
Dual Antiplatelet Therapy (DAPT) Explained
Dual Antiplatelet Therapy (DAPT) is key for patients after a stent is put in. DAPT uses two antiplatelet drugs: aspirin and a P2Y12 receptor inhibitor (like clopidogrel, prasugrel, or ticagrelor). These drugs stop platelets from sticking together and forming clots that could block the stent.
It’s important for patients to know how DAPT prevents stent thrombosis. This is a serious condition. DAPT stops platelets from getting too active, which lowers the chance of clots in the stent.
Duration of Medication Requirements
The time patients need to take DAPT depends on several things. These include the type of stent, the patient’s health, and the disease’s complexity. Usually, patients with drug-eluting stents need DAPT for 6 to 12 months. Those with bare-metal stents might only need it for at least 1 month.
We help figure out the right DAPT time for each patient. This is based on their risk factors and health status.
Managing Side Effects of Antiplatelet Therapy
DAPT is vital but comes with risks. Common side effects include a higher chance of bleeding. This can be from small bruises to serious bleeding. Patients should tell their doctor right away if they notice any bleeding, like easy bruising or blood in urine or stool.
We teach patients how to handle minor bleeding and when to get help fast.
Risks of Premature Discontinuation
Stopping DAPT too soon is a big risk. It can lead to stent thrombosis, heart attacks, or even death. Patients should not stop their antiplatelet therapy without talking to their doctor. Changing DAPT should be decided with a cardiologist, considering the patient’s health and risks.
We stress the importance of sticking to the medication plan. This is to get the best results after a coronary stent is placed.
Alternatives to Coronary Stent Procedures
Looking into other options for coronary stents can help patients find the best fit for their needs. Stents are a common and effective way to treat coronary artery disease. But, not everyone might be a good candidate or might want something else.
Optimal Medical Therapy Approaches
Optimal medical therapy (OMT) is a detailed plan to manage coronary artery disease. It uses medicines and lifestyle changes to control symptoms and slow the disease. This includes antiplatelet agents, beta-blockers, ACE inhibitors or ARBs, and statins.
Research shows OMT can greatly improve outcomes for patients with coronary artery disease. It lowers the risk of serious heart problems.
Coronary Artery Bypass Grafting (CABG)
CABG is a surgery that bypasses blocked or narrowed arteries. It uses grafts, often from the patient’s own veins or arteries. It’s often suggested for complex or multi-vessel disease.
CABG can lead to better survival and fewer symptoms for some patients. But, it’s a more invasive procedure than stent placement, needing a longer recovery.
Lifestyle Modifications as Treatment
Changing your lifestyle is key in managing coronary artery disease. Eating a heart-healthy diet, exercising regularly, quitting smoking, and keeping a healthy weight are important.
These changes can help manage risk factors, improve heart health, and sometimes avoid the need for more invasive treatments.
Newer Interventional Approaches
Newer methods are being explored beyond traditional stents and CABG. These include advanced imaging, new stent technologies, and different access methods.
For example, bioabsorbable stents and drug-coated balloons are new treatments for coronary artery disease. They offer innovative and potentially better options.
|
Treatment Option |
Invasiveness |
Recovery Time |
Benefits |
|---|---|---|---|
|
Optimal Medical Therapy |
Low |
Immediate |
Reduces symptoms, slows disease progression |
|
CABG |
High |
Several weeks to months |
Improved survival, reduced symptoms in complex disease |
|
Lifestyle Modifications |
Low |
Ongoing |
Improves overall cardiovascular health, reduces risk factors |
|
Newer Interventional Approaches |
Varies |
Varies |
Innovative treatments with possible benefits |
In conclusion, while stents are common, there are other options like OMT, CABG, lifestyle changes, and new treatments. The right choice depends on the patient’s health, disease severity, and personal preferences.
Living With a Coronary Stent Long-Term
Living with a coronary stent means you need to take care of your heart every day. You’ll have to change your routine to keep your heart healthy.
Follow-up Care Schedule
It’s important to see your doctor regularly after getting a coronary stent. These visits help make sure the stent is working right and catch any problems early.
|
Timeframe |
Follow-up Activities |
|---|---|
|
1-3 months |
Check stent patency, adjust medications |
|
6-12 months |
Stress test, assess cardiac risk factors |
|
Annually |
Cardiac evaluation, risk factor management |
Lifestyle Adjustments for Heart Health
Choosing a healthy lifestyle is key for those with a coronary stent. This means eating well, not smoking, and keeping a healthy weight.
- Eat a balanced diet rich in fruits, vegetables, and whole grains
- Engage in regular physical activity, as recommended by your healthcare provider
- Manage stress through techniques like meditation or yoga
Exercise Recommendations and Limitations
Exercise is important for heart health, but there are rules for those with a coronary stent. Most can start normal activities a few days to a week after the procedure.
Recommended exercises: Brisk walking, swimming, cycling
Exercises to avoid: High-intensity activities, heavy lifting
Managing Cardiac Risk Factors
Keeping your heart risk factors under control is key for long-term health. This means managing blood pressure, cholesterol, and diabetes.
Understanding and managing these factors can greatly improve your health and life quality.
Special Considerations for Stent Patients
As a stent patient, knowing certain things is key for a smooth recovery and good health. After getting a coronary stent, you need to pay attention to many parts of your life. This helps avoid problems and keeps you feeling well.
Travel Considerations
Traveling with a coronary stent is usually safe, but you must be careful. Tell your airline about your health and any medicines you take when you book. It’s smart to carry a medical ID and a doctor’s letter about your health and treatment.
- Make sure you have enough of your medicines.
- Keep your medicines in their original packaging in your carry-on.
- Look up the medical facilities at your destination for emergencies.
Medical ID Information
A medical ID can save your life in an emergency. It tells doctors about your stent and medicines, helping you get the right care.
Think about these things when getting a medical ID:
- Make sure it has your name, stent type, and medicines.
- Pick a strong ID that lasts a long time.
- Tell a family member or friend about your medical ID and where it is.
Future Medical and Dental Procedures
Always tell your doctor about your stent before any medical or dental work. Some procedures might need changes to your medicine or special care to avoid risks.
For dental work, keeping your teeth clean is very important. This helps stop infections that could harm your stent.
MRI and Other Imaging Compatibility
Most coronary stents work well with MRI scans. But, you must tell your MRI technician about your stent, including what kind it is and when it was put in.
Knowing these special things helps stent patients live healthy, active lives. Always talk to your doctor for advice on managing life with a coronary stent.
When to Seek Emergency Care After Stent Placement
Knowing when to get emergency care after a stent is key. After a coronary stent, it’s vital to watch for complications. Knowing when to get help fast is lifesaving.
Warning Signs of Stent Complications
Stent placement is usually safe, but complications can happen. Watch for these signs:
- Chest Pain or Discomfort: A sign the heart isn’t getting enough blood.
- Shortness of Breath: Feeling winded even when sitting or lying down.
- Severe Fatigue: Feeling extremely tired for no reason.
- Dizziness or Fainting: Feeling dizzy or fainting.
- Rapid or Irregular Heartbeat: Feeling your heart beat fast or irregularly.
Symptoms That Require Immediate Attention
If you have these symptoms after a stent, get emergency care right away:
|
Symptom |
Description |
|---|---|
|
Severe Chest Pain |
A crushing feeling in the chest that spreads to the arm, neck, or jaw. |
|
Confusion or Difficulty Speaking |
Slurred speech, confusion, or trouble understanding others. |
|
Weakness or Numbness |
Sudden weakness or numbness in the face, arm, or leg. |
Differentiating Normal Recovery from Complications
Some discomfort or bruising at the catheter site is normal after a stent. But, it’s important to tell the difference between normal recovery and complications. If you’re not sure, it’s safer to get medical help.
By knowing the warning signs of stent complications and when to seek emergency care, you can have a smoother recovery. This helps avoid risks from stent placement.
Conclusion
We’ve looked into coronary stents, what they are, and how they work. We’ve also covered the procedure, its benefits, and risks. In short, coronary stent placement is a way to keep heart arteries open, improving blood flow.
It’s key to know about stent aftercare and possible stent complications. Following the stent summary guidelines helps patients recover well. This way, they can avoid problems and get the best results.
Coronary stent placement is a great option for heart disease. It improves life quality and lowers heart attack risk. Knowing about the procedure helps patients make good choices. This leads to a successful coronary stent conclusion.
FAQ
What is a coronary stent and how does it work?
A coronary stent is a small, mesh-like tube. It keeps the coronary arteries open, improving blood flow to the heart. It’s placed in the narrowed or blocked artery during an angioplasty, expanding to keep the artery open.
Is a coronary stent considered major surgery?
No, placing a coronary stent is a minimally invasive procedure, not major surgery. It’s done through a small puncture in the wrist or groin. Most patients can go home the same day.
What is the difference between a bare-metal stent and a drug-eluting stent?
Bare-metal stents are made of metal mesh and work by mechanically keeping the artery open. Drug-eluting stents release medication that prevents cell growth. This reduces the risk of the artery narrowing again. Drug-eluting stents have a lower rate of restenosis compared to bare-metal stents.
What is right heart catheterization (RHC), and why is it performed?
Right heart catheterization is a procedure that involves inserting a catheter into the right side of the heart. It measures the pressures in the heart and lungs. It’s used to diagnose and manage conditions like pulmonary hypertension and heart failure.
What are normal pressure values during a right heart catheterization?
Normal pressures during RHC vary. Generally, the mean pulmonary artery pressure is less than 20 mmHg. The pulmonary capillary wedge pressure is between 6-12 mmHg. These values help diagnose various heart and lung conditions.
How is a coronary stent implanted, and what are the steps involved?
The coronary stent implantation involves accessing the coronary artery through a catheter. This is usually done via the radial or femoral artery. The steps include angiography to identify the blockage, balloon angioplasty to open the artery, and then stent placement to keep the artery open.
What are the benefits of having a coronary stent?
The benefits of having a coronary stent include immediate symptom relief and reduced risk of heart attack. It also improves quality of life. Stents can be more effective than medical therapy alone in managing coronary artery disease.
What are the risks and complications of coronary stent placement?
Potential risks and complications include procedural complications, in-stent restenosis, stent thrombosis, and bleeding risks. These risks are important to understand for making informed decisions.
What medications are required after coronary stent placement?
After coronary stent placement, patients need dual antiplatelet therapy (DAPT) to prevent clot formation on the stent. The duration of DAPT varies based on the stent type and individual patient factors.
How long does it take to recover from a coronary stent procedure?
Recovery from a coronary stent procedure is relatively quick. Most patients can resume normal activities within a few days to a week. The first 24-48 hours are critical for monitoring, and follow-up care is necessary for long-term recovery.
Can I travel after getting a coronary stent?
Yes, but wait a few weeks after the procedure. Carry medical identification and information about your stent and medications when traveling.
Are there any lifestyle changes I need to make after getting a coronary stent?
Yes, making lifestyle adjustments is key for maintaining heart health. This includes diet modifications, regular exercise, managing cardiac risk factors, and adhering to prescribed medications.
Reference
JAMA Network. Evidence-Based Medical Insight. Retrieved from https://jamanetwork.com/journals/jama/fullarticle/1748148[1








