Last Updated on November 26, 2025 by Bilal Hasdemir
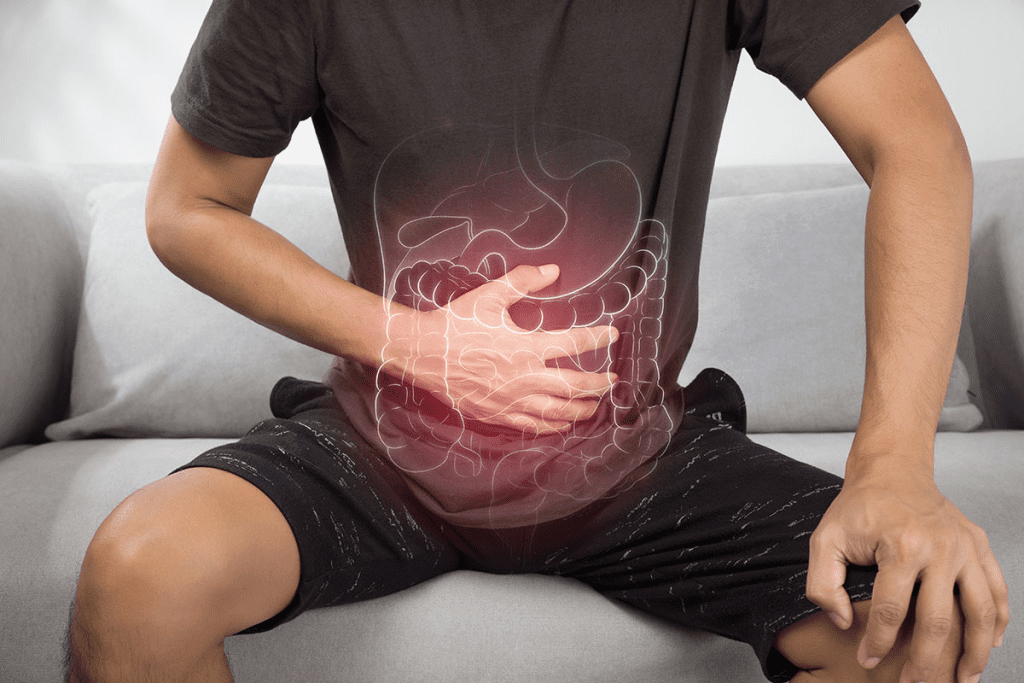
Nearly 50% of cancer patients get radiation therapy. Many of them face gastrointestinal side effects, like colon damage.
Radiation proctitis happens when the colon gets hurt by radiation injury. This usually comes from radiotherapy for cancer. Knowing about its causes, symptoms, and treatments is key. It helps manage the condition and improve life quality for those affected.
Key Takeaways
- Radiation therapy can cause damage to the colon.
- Radiation proctitis is a common side effect of pelvic radiation.
- Understanding the causes and symptoms is key for effective management.
- Treatment options vary based on the condition’s severity.
- Early diagnosis can greatly improve treatment outcomes.
The Effects of Radiation on Colon Tissue
It’s important to know how radiation impacts colon tissue to manage side effects. Radiation therapy is used to treat many cancers. But, it can harm the colon in ways that are immediate and delayed.
This harm can cause a variety of symptoms and problems.
How Radiation Damages Cells
Radiation changes cells’ DNA, causing them to die or not work right. Ionizing radiation can break DNA strands, messing up cell function. This damage can start an inflammatory response, affecting nearby tissue.
The cells in the colon are very sensitive to radiation. When these cells get damaged, it can cause inflammation and ulceration. This can weaken the colon wall over time, leading to chronic conditions like radiation proctitis.
Immediate vs. Delayed Tissue Response
The body’s response to radiation can be split into immediate and delayed effects. Immediate effects happen right away or soon after treatment. Symptoms like diarrhea and stomach pain are common. These are due to the body’s quick inflammatory response to radiation.
Delayed effects show up months or years later. These can include long-term inflammation, tissue scarring, and serious issues like rectal bleeding or strictures. Knowing when these effects happen is key to caring for patients and preventing long-term harm.
What is Radiation Proctitis?
Radiation proctitis is inflammation of the rectum, most often occurring in patients receiving pelvic-area radiation therapy.
Definition and Clinical Presentation
Radiation proctitis damages the lining of the rectum because of radiation. Symptoms can range from mild to severe. They include bleeding, diarrhea, and pain in the rectum.
This condition can really affect a person’s life. It needs proper care and treatment.
Clinical manifestations can show up during or after radiation therapy. They can be either acute or chronic. Acute happens during or right after treatment. Chronic can appear months or years later.
Incidence Rates Among Cancer Patients
The chance of getting radiation proctitis depends on the cancer type and radiation dose. People getting radiation for pelvic malignancies like prostate, cervical, and rectal cancers are more at risk. Studies show that 5% to 20% of patients getting pelvic radiation therapy might get radiation proctitis.
Knowing the risk factors and how common it is helps in managing and preventing it. The dose of radiation, how much of the rectum is exposed, and how a person reacts to radiation all matter.
Cancer Treatments That Can Cause Colon Damage
Certain cancer treatments can harm the colon. This includes radiation for colorectal, prostate, and gynecological cancers. A common issue is radiation proctitis, which is inflammation of the rectum lining.
Colorectal Cancer Radiation
Radiation therapy is used to treat colorectal cancer. It can be used alone or with surgery or chemotherapy. But, it can also damage healthy tissue around the cancer, causing colon damage and radiation proctitis.
Prostate Cancer Radiation
Prostate cancer radiation therapy can also harm the colon. The prostate is close to the rectum. This means the colon can get exposed to radiation, leading to radiation proctitis.
Gynecological Cancer Treatments
Radiation therapy for gynecological cancers can also cause colon damage. The pelvic area, where the colon is, gets exposed to radiation. This increases the risk of radiation proctitis.
It’s important to know the risks of these treatments. Patients should be watched for signs of radiation proctitis. Early action can help prevent long-term problems.
Recognizing Symptoms of Radiation Damage
It’s important to know the signs of radiation proctitis early. This condition can cause many gastrointestinal problems. These issues can really affect how well you live your life.
Common Gastrointestinal Symptoms
Diarrhea, urgency, and feeling like you didn’t finish going are common symptoms. These can make everyday tasks hard. Spotting these symptoms early is key to managing them well.
Some people might also get constipation or have changes in their bowel habits. This can be just as tough. Doctors need to watch these signs closely and adjust treatment plans as needed.
Rectal Bleeding and Discharge
Seeing bright red or maroon blood when you go to the bathroom is a big sign. It means you need to see a doctor right away. Rectal discharge can also happen, making things worse.
If you notice bleeding or discharge, it’s important to get checked out. A doctor can figure out how bad the radiation proctitis is and what to do next.
Pain and Discomfort Patterns
The pain from radiation proctitis can feel different for everyone. Some might feel a dull ache, while others might have sharp pains. Pain when you go to the bathroom is a big problem for many.
Understanding your pain is important for finding ways to make it better. Doctors can suggest different ways to help with these symptoms. This can really help improve your life.
Diagnosing Radiation-Induced Colon Damage
Healthcare providers use a mix of clinical checks, endoscopy, and imaging to spot radiation proctitis. This method is key to figuring out how bad the damage is and what treatment is needed.
Clinical Evaluation Process
The first step is a detailed medical history and physical check-up. Doctors look for signs like rectal bleeding, pain, and changes in bowel movements. They also check the patient’s radiation therapy history.
Understanding symptoms is very important. This includes:
- Figuring out how bad and long symptoms last
- Finding out what makes symptoms better or worse
- Seeing how symptoms affect the patient’s life
Endoscopic and Imaging Studies
Endoscopy, like sigmoidoscopy or colonoscopy, lets doctors see the rectal lining directly. They can spot inflammation, ulcers, or other signs of radiation damage.
Imaging tests, like CT scans or MRI, show more about the damage and possible problems like strictures or fistulas. These tests help doctors understand how severe the damage is and plan the best treatment.
Diagnosing radiation damage in the colon is a detailed process. It combines clinical checks and advanced tests. This way, doctors can accurately diagnose and treat radiation proctitis.
Acute vs. Chronic Radiation Proctitis
Radiation proctitis can be acute or chronic, each with its own traits and needs. Knowing the difference is key for the right treatment.
Timeframe and Symptom Differences
Acute radiation proctitis happens right after or during radiation therapy, usually in the first few weeks. Symptoms include diarrhea, urgency, and discomfort. On the other hand, chronic radiation proctitis can start months or years later. It can get worse over time, causing more severe symptoms like bleeding, pain, and bowel changes.
Acute symptoms usually go away after treatment ends. But chronic symptoms can last, needing constant care.
Progression and Prognosis
The way radiation proctitis progresses varies. Acute radiation proctitis might get better once treatment stops. But sometimes, it can turn into the chronic form. Chronic radiation proctitis, though, is a long-lasting issue. It can cause serious problems like strictures, fistulas, and ongoing bleeding.
How well a patient does with radiation proctitis depends on the symptoms’ severity and how long they last. Early treatment and care are important for better outcomes. For chronic cases, ongoing monitoring and treatment are needed to manage symptoms and avoid complications.
In summary, it’s important to tell acute from chronic radiation proctitis to give the right treatment. Understanding the differences helps doctors provide better care.
Medical Treatments for Radiation Proctitis
Managing radiation proctitis involves several treatments. These include anti-inflammatory drugs and protective agents. The right treatment depends on how bad the symptoms are and the patient’s health.
Anti-inflammatory Medications
Anti-inflammatory drugs are often the first choice for treating radiation proctitis. Mesalamine and corticosteroids help lessen inflammation. This makes symptoms like bleeding and diarrhea better. Mesalamine works best when applied directly to the affected area.
Sucralfate and Protective Agents
Sucralfate is also used to treat radiation proctitis. It forms a protective layer over ulcers, helping them heal. Sucralfate enemas are a common treatment, putting the medication right in the rectum.
Antibiotics and Other Medications
Antibiotics might be needed to fight off infections that can happen with radiation proctitis. Other drugs help control diarrhea and manage pain. These can greatly improve a patient’s life quality.
Every treatment plan for radiation proctitis is unique. It considers the severity of symptoms, the damage from radiation, and the patient’s health history. A healthcare provider will work with the patient to create a detailed treatment plan.
Advanced Interventions for Severe Cases
For severe radiation proctitis, advanced treatments are key. When usual treatments don’t work, doctors use more complex methods. These help ease symptoms and improve life quality for patients.
Endoscopic Therapies
Endoscopic therapies are a valuable option for severe cases. Argon Plasma Coagulation (APC) is one such therapy. It uses argon gas and electrical current to treat bleeding and inflammation.
Benefits of APC:
- Minimally invasive procedure
- Effective in controlling bleeding
- Reduces symptoms and improves quality of life
Hyperbaric Oxygen Treatment
Hyperbaric oxygen therapy (HBOT) involves breathing pure oxygen in a pressurized room. It boosts oxygen to damaged tissues, aiding in healing. HBOT is effective in treating radiation proctitis by reducing inflammation and promoting tissue repair.
| Treatment | Benefits | Potential Side Effects |
| Hyperbaric Oxygen Therapy | Promotes healing, reduces inflammation | Ear barotrauma, oxygen toxicity |
| Argon Plasma Coagulation | Controls bleeding, reduces symptoms | Rare complications include bowel perforation |
Surgical Options for Refractory Cases
In severe cases, surgery might be needed. Surgical options include repairing or removing damaged rectum parts. Surgery can offer significant relief but comes with risks.
Considerations for Surgical Intervention:
- Severity of symptoms and impact on quality of life
- Failure of other treatments
- Overall health and surgical risk assessment
Understanding advanced interventions helps patients and doctors choose the best treatment for severe radiation proctitis.
Nutritional Management and Dietary Considerations
A well-planned diet is key to lessening radiation proctitis’s impact on the colon. It helps manage the condition, reduce symptoms, and enhance life quality for those affected.
Foods to Avoid During Treatment
Some foods can make radiation proctitis symptoms worse. It’s wise to steer clear of:
- Spicy foods that can irritate the rectal lining and cause discomfort.
- High-fiber foods such as beans, cabbage, and broccoli that can be hard to digest.
- Dairy products if you are lactose intolerant, as they can cause more gastrointestinal issues.
- Caffeine and alcohol that can dehydrate the body and make symptoms worse.
Beneficial Dietary Choices
Choosing the right foods can help manage radiation proctitis. Here are some suggestions:
- Low-fiber foods like white bread, bananas, and applesauce that are easier to digest.
- Adequate hydration by drinking plenty of water all day.
- Electrolyte-rich beverages to replace lost salts and minerals.
- Probiotics found in yogurt or supplements to support gut health.
A study in the Journal of Clinical Gastroenterology found that “Dietary modifications can significantly impact the management of radiation proctitis, improving patient outcomes.”
“A diet rich in essential nutrients and fiber can help mitigate the effects of radiation on the gastrointestinal system.”
– Journal of Clinical Gastroenterology
By choosing the right foods, patients can manage their symptoms better and improve their overall health.
Managing Daily Life with Radiation Proctitis
Living with radiation proctitis is tough. It requires a mix of strategies to handle symptoms well. Patients need to adjust to bowel changes, find ways to ease rectal pain, and keep their quality of life good.
Coping with Bowel Changes
Bowel changes are common in radiation proctitis. Diarrhea, urgency, and incontinence can really disrupt daily life. To tackle these issues, patients can try:
- Maintaining a food diary to identify trigger foods
- Eating smaller, more frequent meals
- Avoiding foods high in fiber or spice
One patient found that keeping a food diary helped. They noticed dairy products made their symptoms worse, so they cut down on them.
“The key to managing bowel changes is being mindful of what you eat and how it affects you.”
Strategies for Rectal Pain Relief
Rectal pain is a big challenge with radiation proctitis. Topical treatments and medications can help. Here are some strategies:
- Using sucralfate enemas to protect the rectal mucosa
- Taking pain relief medication as prescribed by a healthcare provider
- Applying warm compresses to the affected area
Maintaining Quality of Life
Keeping a good quality of life with radiation proctitis takes a team effort. It involves medical care, lifestyle changes, and emotional support. Staying connected with healthcare providers and support groups is key.
A healthcare professional said, “A care plan that covers physical and emotional needs is vital for patients with radiation proctitis.”
By using these strategies and staying informed, patients can manage their symptoms better. This helps improve their quality of life.
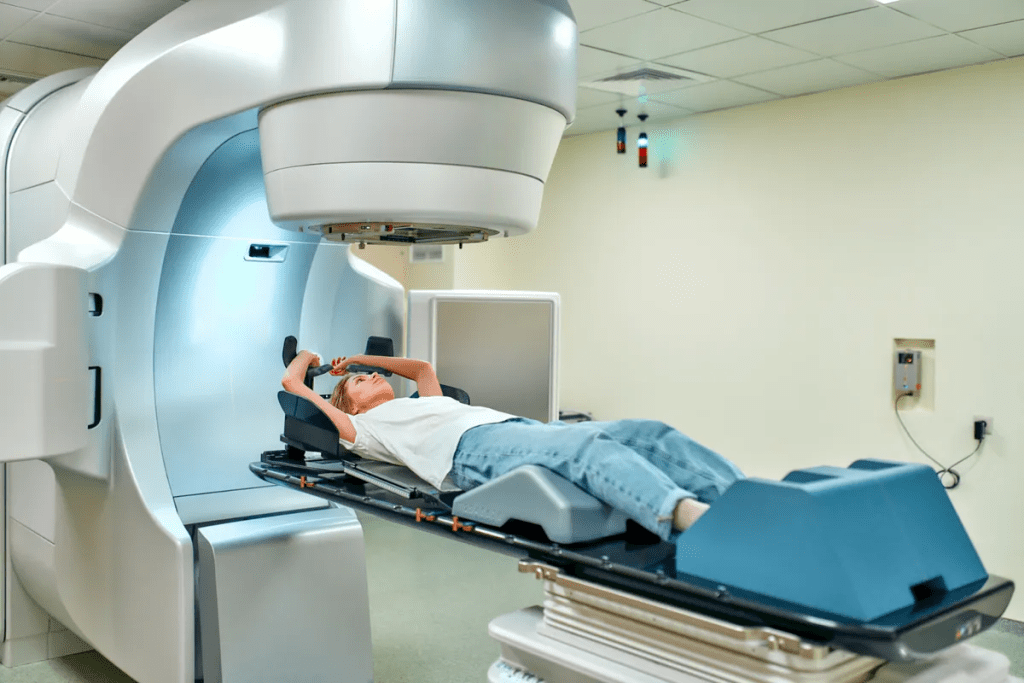
Modern Radiation Techniques That Minimize Colon Damage
Modern radiation methods have changed cancer treatment a lot. They greatly lower the chance of colon damage. New tech in radiation lets doctors give more precise and better treatment.
Intensity-Modulated Radiation Therapy (IMRT)
Intensity-Modulated Radiation Therapy (IMRT) is a high-tech way to send radiation to tumors. It uses special computer programs to adjust the radiation beams. This makes sure the tumor gets the right dose, while keeping healthy tissues safe.
This method is great for tumors near the colon. It cuts down the chance of damage from radiation. Research shows IMRT lowers side effects in the gut for patients getting radiation.
Image-Guided Radiation Therapy (IGRT)
Image-Guided Radiation Therapy (IGRT) makes radiation treatment even more precise. It uses X-rays or CT scans to guide the beams to the tumor. This way, the radiation hits the tumor right on, even if it moves or is close to important areas.
IGRT is super helpful for tumors in the pelvic area. It lets doctors adjust the beams in real-time. This keeps the colon safe from damage.
Long-term Complications of Radiation Damage
Long-term effects of radiation on the colon can be serious and varied. This requires detailed care. Radiation proctitis, caused by radiation therapy, can lead to chronic problems.
Strictures and Fistulas
Strictures and fistulas are major complications. Strictures narrow the colon or rectum, causing blockages. Fistulas create abnormal connections, leading to pain, blockages, and infections.
These issues can greatly reduce a patient’s quality of life. They often need surgery to fix. Treatment may include dilation for strictures and repair for fistulas, along with symptom management.
Chronic Bleeding Issues
Chronic bleeding is a common issue from radiation proctitis. It can be mild or severe, damaging blood vessels. This bleeding can cause anemia and needs ongoing care.
Endoscopic treatments, like argon plasma coagulation, can stop the bleeding. Regular check-ups are key to managing this problem.
Functional Bowel Changes
Radiation can also cause functional bowel changes. Symptoms include diarrhea, urgency, and incontinence. These can greatly impact daily life, requiring diet changes and medication.
Dietary advice and medications can help manage symptoms. Sometimes, more treatments are needed for specific issues.
Psychological Impact of Chronic Radiation Proctitis
The mental effects of chronic radiation proctitis are often overlooked. Yet, they greatly affect patients’ lives. Dealing with this condition is tough, affecting both body and mind.
Dealing with Uncertainty and Chronic Symptoms
People with chronic radiation proctitis feel many emotions. They might feel anxious, frustrated, or even depressed. The ongoing nature of their symptoms, like bleeding and pain, can really disrupt their daily routines.
Coping Strategies are key to handling the mental side. These can include:
- Getting help from healthcare professionals
- Trying stress-reducing activities like meditation or yoga
- Joining support groups for advice and shared experiences
As one patient shared, “
It’s been a journey, learning to live with the symptoms and finding ways to manage the pain and discomfort. Support from family, friends, and healthcare providers has been invaluable.
“
Support Resources and Coping Strategies
Access to the right support can really help. This includes:
- Professional counseling for anxiety and depression
- Learning materials to better understand the condition
- Online forums and support groups for connection
Early intervention and a detailed care plan can lessen the mental impact. This improves overall well-being.
By recognizing the mental side of chronic radiation proctitis and providing the right support, healthcare providers can offer better care. This improves patients’ quality of life.
Emerging Research and Future Treatments
New research is uncovering ways to treat radiation proctitis, giving hope to patients. As we learn more about this condition, new treatments are being developed. These aim to fix the damage caused by radiation in the colon.
It’s important to find new treatments because radiation proctitis affects cancer survivors’ lives a lot. Recent studies are working on treatments that are more effective and easier to use.
Stem Cell Therapies
Stem cell therapies are a promising area of research for treating radiation proctitis. Stem cells can turn into different types of cells, which might fix damaged tissue. Early trials have shown positive results, with some patients seeing big improvements.
Stem cells could help grow back damaged mucosa and fix tissue function. This could offer a lasting fix for those with radiation proctitis.
Novel Anti-inflammatory Approaches
Researchers are also looking into novel anti-inflammatory approaches for radiation proctitis. They’re creating new medicines that target inflammation in the condition.
These new treatments aim to lessen symptoms and help patients feel better. Early trials suggest they might be effective, giving hope for better managing radiation proctitis.
The future of treating radiation proctitis looks bright. Ongoing research and trials are leading to new, better ways to help patients.
When to Seek Specialized Medical Care
Knowing when to see a specialist is key for managing radiation proctitis. People who have had radiation therapy for cancers like prostate, cervical, or colorectal should watch their health closely after treatment.
Warning Signs That Require Immediate Attention
Certain symptoms need immediate medical help. These include:
- Severe rectal bleeding: Heavy or ongoing bleeding from the rectum is a big warning sign.
- Increased pain: If your rectal pain or discomfort gets worse and doesn’t get better with usual treatments, seek help.
- Changes in bowel habits: If you have persistent diarrhea, constipation, or any big change in how you go to the bathroom, it’s important to act fast.
- Fever or infection signs: Fever, chills, or other signs of infection could mean you have a complication.
If you notice any of these symptoms, call your healthcare provider right away.
Finding Specialists in Radiation Proctitis
Finding the right specialist is vital for managing your condition well. Here’s how to do it:
- Ask for referrals: Your primary care doctor or oncologist can suggest specialists.
- Check credentials: Make sure the specialist has experience with radiation proctitis.
- Consider a gastroenterologist: A gastroenterologist is great for treating issues with the colon and rectum, which are affected by radiation proctitis.
Seeing a specialist can help you get care that fits your needs. This can greatly improve your life quality.
Conclusion: Navigating Life After Radiation Treatment
Life after radiation treatment means dealing with radiation proctitis and its lasting effects. It’s key to manage this well to improve your life quality.
Radiation proctitis can really affect your daily life. It can cause rectal bleeding, pain, and changes in bowel movements. Knowing about treatments and lifestyle changes is important to lessen these symptoms.
Handling radiation proctitis long-term needs a full plan. This includes changing your diet, finding coping strategies, and sometimes using advanced medical treatments. These steps help you deal with life after radiation treatment better.
New research brings hope for better managing radiation proctitis. Keeping up with these new findings helps you make better choices for your care.
FAQ
What is radiation proctitis?
Radiation proctitis is inflammation and damage to the lower part of the colon (rectum). It’s caused by radiation therapy. This therapy is often used to treat cancers like colorectal, prostate, and gynecological cancers.
What are the common symptoms of radiation proctitis?
Symptoms include diarrhea, rectal bleeding, discharge, pain, and discomfort. These symptoms can affect daily life and vary in severity.
How is radiation proctitis diagnosed?
Doctors use a clinical evaluation, endoscopic exams, and imaging studies. These help see the rectum and check for damage extent and other conditions.
What is the difference between acute and chronic radiation proctitis?
Acute radiation proctitis happens during or soon after treatment. Chronic cases occur months or years later. Chronic cases can be more severe and last longer.
What treatments are available for radiation proctitis?
Treatments include anti-inflammatory meds and protective agents like sucralfate. There are also endoscopic therapies, hyperbaric oxygen therapy, and surgery for severe cases.
How can dietary changes help manage radiation proctitis?
Avoiding spicy or high-fiber foods and staying hydrated can help. Choosing the right foods can manage symptoms.
Can modern radiation techniques reduce the risk of colon damage?
Yes, newer techniques like IMRT and IGRT aim to protect healthy tissues. This reduces the risk of radiation proctitis.
What are the long-term complications of radiation damage to the colon?
Complications include strictures, fistulas, chronic bleeding, and bowel changes. These can greatly affect quality of life.
How can patients cope with the psychological impact of chronic radiation proctitis?
Seeking support from healthcare providers and support groups is key. Counseling helps manage symptoms and uncertainty, keeping mental health strong.
Are there emerging treatments for radiation proctitis?
Yes, research is exploring new treatments. This includes stem cell therapies and anti-inflammatory approaches for future management.
When should patients seek specialized medical care for radiation proctitis?
Seek care for severe symptoms, significant bleeding, or worsening condition. Finding specialists is important for effective management.
Can radiation proctitis be cured?
While some cases can be managed well, a “cure” depends on damage severity. Treatment aims to manage symptoms and prevent complications.
How does radiation therapy cause colon damage?
Radiation damages colon cells, causing inflammation and symptoms. Damage extent depends on radiation dose and duration.