Coronary artery disease is a big problem worldwide, hitting millions every year. Blocked coronary arteries can be fixed with angioplasty. This method helps blood flow to the heart without needing open-heart surgery.
So, what’s the difference between a stent and angioplasty? Angioplasty uses a balloon to widen narrowed or blocked arteries. A stent is a small, metal mesh tube. It’s placed during or after angioplasty to keep the artery open.
Key Takeaways
- Angioplasty is a procedure used to open blocked coronary arteries.
- A stent is a small, metal mesh tube that keeps the artery open.
- Both procedures are key in treating coronary artery disease.
- Angioplasty restores blood flow to the heart muscle without open-heart surgery.
- Stent placement helps prevent the artery from becoming blocked again.
Understanding Cardiovascular Disease and Blocked Arteries

Cardiovascular disease happens when arteries narrow or block due to plaque buildup. This reduces blood flow to the heart. Symptoms include chest pain and shortness of breath.
Common Causes of Arterial Blockage
Arterial blockage often comes from atherosclerosis. This is when plaque, made of fat, cholesterol, and more, builds up in arteries. Over time, this plaque can harden or rupture, causing blood clots that block the artery.
Several factors can lead to arterial blockage. These include:
- High cholesterol: High levels of LDL cholesterol can cause plaque buildup.
- Smoking: Smoking damages blood vessel linings, making them more likely to block.
- Diabetes: High blood sugar can damage blood vessels and nerves, raising cardiovascular disease risk.
- Hypertension: High blood pressure can damage blood vessel walls, increasing blockage risk.
How Blockages Affect Heart Health

Blocked arteries mean the heart muscle doesn’t get enough oxygen and nutrients. This can lead to serious health issues. The impact depends on where and how much the artery is blocked.
Blocked arteries can cause:
- Angina: Chest pain or discomfort from reduced blood flow to the heart.
- Heart attack: A blockage that cuts off blood flow to a heart part, causing damage or death.
- Heart failure: The heart can’t pump enough blood, possibly due to repeated or severe blockages.
Signs and Symptoms of Arterial Blockage
It’s important to know the signs and symptoms of arterial blockage. This can help get medical help quickly. Common symptoms include:
|
Symptom |
Description |
|---|---|
|
Chest pain (angina) |
Discomfort or pain in the chest, often triggered by exertion or stress. |
|
Shortness of breath |
Difficulty breathing, which can occur at rest or during physical activity. |
|
Fatigue |
Feeling unusually tired or weak, possibly due to reduced blood flow. |
|
Pain or weakness in the legs |
Discomfort or weakness in the legs, often during walking, due to peripheral artery disease. |
Understanding cardiovascular disease and blocked arteries is key. It shows why treatments like angioplasty and stenting are important. Knowing the causes, effects, and symptoms helps people get medical help quickly to avoid serious problems.
What is Coronary Angioplasty?
Percutaneous coronary intervention, or coronary angioplasty, has changed how we treat heart disease. It’s a small procedure that opens up blocked heart arteries. This helps blood flow back to the heart.
Definition and Purpose
Coronary angioplasty uses a balloon to widen blocked arteries. Its main goal is to ease heart pain and prevent heart attacks. It does this by improving blood flow to the heart muscle.
Often, a stent is placed during the procedure. This is a small, mesh-like device that keeps the artery open. But, sometimes angioplasty is done without a stent, depending on the patient’s situation and the blockage’s nature.
History and Development of Angioplasty
“The development of coronary angioplasty has been a landmark in the management of coronary artery disease, providing a less invasive option compared to coronary artery bypass grafting.”
When Angioplasty is Recommended
Doctors usually suggest angioplasty for those with severe heart disease who haven’t gotten better with medicine or lifestyle changes. It’s also an emergency treatment for heart attacks. It quickly opens up the blocked heart area.
- Symptomatic coronary artery disease
- Acute coronary syndrome
- High-risk patients with significant blockages
Knowing about coronary angioplasty helps patients make better choices about their health. They can talk to their doctors about it.
The Balloon Angioplasty Procedure Explained
Learning about balloon angioplasty can make patients feel more at ease. This procedure, also known as percutaneous transluminal angioplasty (PTA), is used to open up narrowed arteries. It’s a minimally invasive method.
Step-by-Step Process
The balloon angioplasty procedure has several important steps:
- A small incision is made in the arm or groin to access the artery.
- A catheter with a deflated balloon is guided to the narrowed section of the artery.
- The balloon is inflated to push aside the plaque and stretch the artery, improving blood flow.
- The balloon is then deflated, and the catheter is removed.
Types of Balloon Catheters Used
There are different types of balloon catheters used in angioplasty:
- Standard Balloon Catheters: These are the most commonly used, fitting most procedures.
- Cutting Balloon Catheters: These have small blades that score the plaque, making it easier to dilate the artery.
- Drug-Coated Balloon Catheters: These balloons are coated with medication to prevent the artery from re-narrowing.
What is a Stent?
Stents are small, mesh tubes used to treat blocked arteries. They are placed in a coronary artery to keep it open. This improves blood flow to the heart.
Definition and Purpose
A coronary stent is a small, metal mesh tube for treating narrow or blocked arteries. Its main goal is to keep the artery open. This improves blood flow to the heart muscle.
Stents are often used with angioplasty to widen narrowed or obstructed arteries. They are designed to be permanent implants. In some cases, they can be biodegradable.
The main goal of stenting is to prevent the artery from re-narrowing after angioplasty. This condition is called restenosis.
Types of Stents Available
There are several types of stents, each with its own benefits and risks. The two main categories are:
- Bare Metal Stents (BMS): These are the original type of stent made from metal mesh. They are less likely to cause allergic reactions but have a higher risk of restenosis compared to drug-eluting stents.
- Drug-Eluting Stents (DES): These stents are coated with medication that is slowly released. This prevents cell proliferation, reducing the risk of restenosis. They are more commonly used today due to their improved outcomes.
|
Stent Type |
Description |
Restenosis Risk |
|---|---|---|
|
Bare Metal Stent |
Metal mesh stent without drug coating |
Higher |
|
Drug-Eluting Stent |
Stent coated with medication to prevent cell growth |
Lower |
Evolution of Stent Technology
The technology behind stents has evolved significantly. Early stents were associated with higher complication rates, including thrombosis and restenosis. Advances in materials and design have led to more sophisticated stents.
The introduction of drug-eluting stents marked a significant improvement. They reduced the incidence of restenosis. More recently, biodegradable stents and stents with newer coatings have been developed. These aim to further enhance safety and efficacy.
As stent technology continues to evolve, we can expect to see even more innovative solutions for treating coronary artery disease. The ongoing development of new materials and designs aims to improve patient outcomes and reduce complications associated with stent placement.
Stent Placement Procedure
Stent placement is a precise process to keep the artery open. It’s key for those with coronary artery disease. It helps get blood flowing to the heart again.
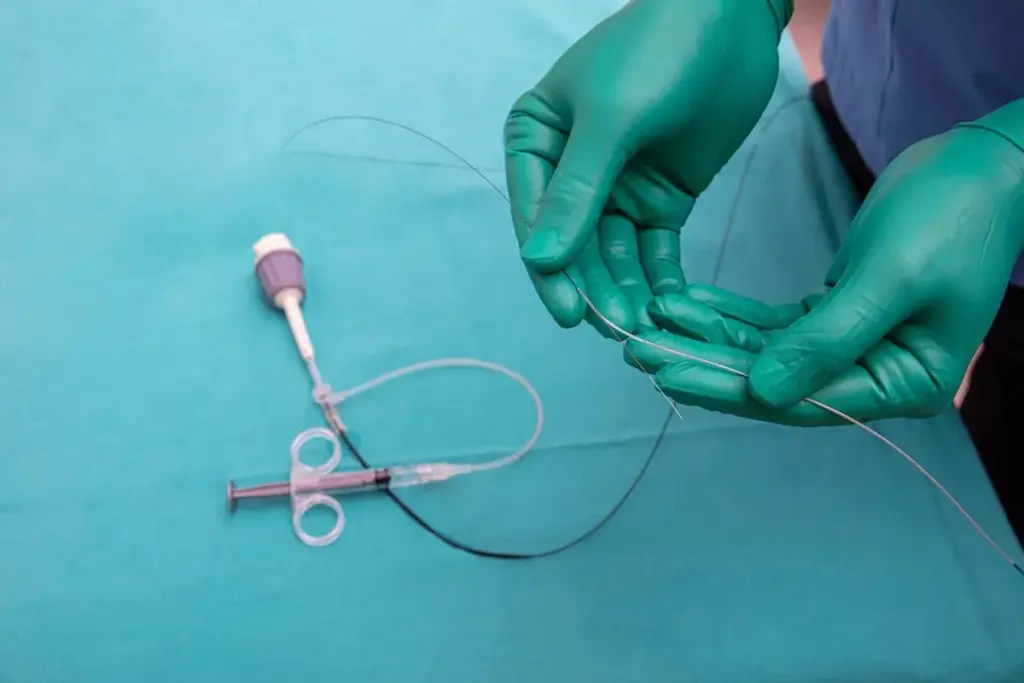
How Stents are Inserted
Stents are put in during an angioplasty. A catheter with a balloon is guided to the blocked artery. Then, the balloon is inflated to widen the artery.
The stent, attached to the balloon, expands to remain in place and keep the artery open.. We use advanced imaging to guide this process. This makes it accurate and lowers risks.
Positioning and Deployment Techniques
Getting the stent in the right spot is key. We use real-time imaging to guide the stent to the blockage. When it’s in place, the balloon inflates to set the stent against the artery walls.
The way the stent is deployed can change based on its type. For example, drug-eluting stents release medicine to stop the artery from narrowing again.
Immediate Post-Stent Evaluation
Right after the stent is set, we check if the artery is open. We look for any issues like bleeding or stent thrombosis.
|
Evaluation Criteria |
Description |
Significance |
|---|---|---|
|
Artery Patency |
Checking if the artery is open |
Ensures blood flow to the heart |
|
Stent Positioning |
Verifying the stent’s correct placement |
Prevents future complications |
|
Blood Flow |
Assessing the restoration of blood flow |
Critical for heart health |
By checking these things, we make sure the stent placement works well. This is good for the patient’s health.
Key Differences Between Stent and Angioplasty
Angioplasty and stent placement are used together to treat coronary artery disease. Angioplasty widens the artery. Stenting places a small mesh device to keep it open.
Procedural Differences
Angioplasty and stenting have different procedures. Angioplasty uses a balloon catheter to widen the artery. Stenting places a stent to keep the artery open after angioplasty.
Key steps for angioplasty include:
- Insertion of a balloon catheter into the narrowed artery
- Inflation of the balloon to widen the artery
- Deflation and removal of the balloon catheter
Stenting involves:
- Deployment of a stent over the balloon catheter
- Inflation of the balloon to expand the stent
- The stent remains to keep the artery open after the balloon is deflated and removed
Outcome Differences
Angioplasty and stenting have different outcomes. Angioplasty alone may not keep the artery open long-term. Stenting reduces the risk of re-narrowing by keeping the artery open with a stent.
Studies show:
- Angioplasty alone has a higher rate of restenosis compared to stenting
- Stenting improves long-term patency rates and reduces the need for repeat procedures
When One is Preferred Over the Other
The choice between angioplasty and stenting depends on several factors. These include the blockage’s severity, patient health, and specific medical scenarios. For example, in emergencies, angioplasty might be used without stenting if the blockage is not severe.
Combined Approach Benefits
Using both angioplasty and stenting is often the best strategy. This method widens the artery immediately and then uses stenting for long-term patency.
The benefits of this combined approach include:
- Immediate relief of symptoms through angioplasty
- Long-term artery patency ensured by stenting
- Reduced risk of complications and re-narrowing
Understanding the differences and benefits of angioplasty and stenting helps healthcare providers tailor treatments. This optimizes outcomes in cardiovascular care.
Preparing for Angioplasty or Stent Procedures
Angioplasty and stent procedures need careful preparation for the best results. We want to make sure you know what to expect and feel comfortable with the steps.
Pre-procedure Testing
We do various tests before the procedure to check your health and artery condition. These might include blood work, ECG, and imaging tests like angiography or ultrasound. These tests help us spot any risks and plan the procedure.
Medication Adjustments
We might need to adjust or stop some medications before the procedure. We’ll look at your current meds, including blood thinners, and tell you what changes are needed. It’s important to follow our advice to reduce risks during and after the procedure.
Fasting and Other Preparations
You’ll likely need to fast before the procedure. We’ll give you clear instructions on fasting and other preparations, like arriving on time and having someone with you. It’s key to follow these instructions carefully for a smooth procedure.
What to Expect on Procedure Day
On procedure day, you’ll go to the catheterization lab for the angioplasty or stent placement. Our team will guide you through each step, making sure you’re comfortable. We know this can be stressful, and we’re here to make it as easy as possible.
By preparing well for your angioplasty or stent procedure, we can work together to get great results and improve your heart health.
When is Balloon Angioplasty Used Without a Stent?
The choice to use balloon angioplasty without a stent depends on many things. These include the patient’s health and the type of blockage in their arteries.
Specific Medical Scenarios
Balloon angioplasty without stenting is often chosen for specific cases. These include:
- Lesions that are relatively short and discrete
- Blockages in smaller coronary arteries where stenting might increase the risk of complications
- Patients with a high risk of bleeding, as stenting often requires longer-term antiplatelet therapy
Also, some patients with a history of in-stent restenosis or those who have had previous stenting complications might be considered for standalone angioplasty.
Advantages of Standalone Angioplasty
There are several advantages to balloon angioplasty without stenting. These include:
|
Advantage |
Description |
|---|---|
|
Reduced Risk of Stent-Related Complications |
By not placing a stent, the risk of stent thrombosis or in-stent restenosis is eliminated. |
|
Less Antiplatelet Therapy Required |
Patients undergoing standalone angioplasty may require shorter or less intensive antiplatelet therapy. |
|
Potential for Repeat Procedures |
If needed, future interventions can be performed without the constraints of previously placed stents. |
Patient Selection Criteria
Choosing the right patients for standalone balloon angioplasty is important. It involves looking at several factors. These include:
- The nature and location of the coronary lesion
- The patient’s overall cardiovascular risk profile
- Previous responses to similar treatments
We use advanced imaging techniques and diagnostic tests to evaluate these factors. This helps us make informed decisions about the best treatment approach.
When is Stenting Necessary After Angioplasty?
Stenting after angioplasty depends on several factors. These include the blockage’s severity and the patient’s heart health.
Medical Indications for Stent Placement
Stenting is often needed after angioplasty for high-risk patients. This includes those with complex blockages, a history of narrowing, or diabetes.
It’s also considered when angioplasty doesn’t fully open the artery. This can happen due to significant narrowing or artery damage.
Emergency Stenting Scenarios
In emergencies like heart attacks, stenting is done right after angioplasty. It’s to quickly restore blood flow.
Stenting is also urgent if angioplasty causes severe damage or sudden blockage.
Planned Stenting Approaches
Stenting is often planned with angioplasty. It’s to keep the artery open and prevent future blockages.
We use advanced imaging to pick the right stent size and placement. This ensures the best results for our patients.
|
Scenario |
Stenting Approach |
Benefits |
|---|---|---|
|
Complex Lesions |
Planned Stenting |
Reduces risk of restenosis |
|
Emergency Situations |
Emergency Stenting |
Restores blood flow quickly |
|
High Risk of Re-narrowing |
Stenting After Angioplasty |
Maintains artery patency |
Understanding when stenting is needed helps us tailor care for our patients. This ensures the best outcomes after angioplasty.
Risks and Complications of Angioplasty
It’s important for patients to know about the risks of angioplasty before they decide to have it. Angioplasty is a common treatment for heart disease. But, it’s not without its risks.
Short-term Risks
Right after angioplasty, patients might face bleeding at the catheter site, blood clots, or allergic reactions to the dye. Bleeding complications can be anything from small bruises to serious bleeding that might need a blood transfusion.
Blood clots are another big risk. They can happen during or right after the procedure. These clots can cause heart attacks or strokes.
Long-term Complications
Over time, patients might face restenosis, or their arteries could narrow again. This happens to a lot of people and might need more treatments.
Another long-term risk is new blockages in other parts of the heart’s arteries. It’s key to keep up with regular check-ups to catch these problems early.
Risk Factors that Increase Complications
Some things can make angioplasty risks higher. These include diabetes, kidney disease, and high blood pressure. People with these conditions need extra care before, during, and after the procedure.
- Diabetes
- Kidney disease
- High blood pressure
How Complications are Managed
Handling angioplasty complications involves medication, lifestyle changes, and sometimes more treatments. For example, taking antiplatelet drugs helps prevent blood clots.
If restenosis happens, repeated angioplasty or stenting might be needed. The best treatment depends on the patient’s situation and the details of their restenosis.
Risks and Complications of Stent Placement
Stent placement is a common treatment for heart disease. But, it comes with risks and complications. It’s important to know what these are.
Stent-Specific Complications
Stent placement can lead to stent-specific complications. These can affect how well the treatment works. There are several main areas of concern.
In-stent restenosis is a big worry. It happens when the artery gets narrow again. This can be due to how the body reacts to the stent.
In-Stent Restenosis
In-stent restenosis is a major issue. It’s when the artery gets narrow again after a stent is placed. We’ll look at why it happens, its symptoms, and how to treat it.
- Causes include neointimal hyperplasia and stent underexpansion.
- Symptoms include recurring angina or chest pain.
- Treatment options include medication and more stenting.
Stent Thrombosis
Stent thrombosis is another serious problem. It’s when a blood clot forms inside the stent. This is a serious emergency that needs quick medical help.
We’ll talk about what increases the risk, symptoms, and how to prevent it.
Bleeding Risks with Antiplatelet Therapy
Patients with stents often take antiplatelet therapy. This helps prevent clots but raises the risk of bleeding.
We’ll discuss how to balance preventing clots and managing bleeding risks. We’ll also look at ways to reduce these risks.
Knowing the risks and complications helps patients and doctors make better choices about treatment.
Recovery After Angioplasty and Stenting
Recovering from angioplasty and stenting involves several steps. You’ll need immediate care, make lifestyle changes, and take ongoing medication. Understanding each stage is key to a successful recovery.
Immediate Post-Procedure Care
Right after the procedure, you’ll be watched closely in a recovery area. Close monitoring helps catch any problems early. You might feel sore or bruised where the catheter was, but this usually goes away in a few days.
Your medical team will give you detailed instructions. They’ll tell you how to care for the catheter site, manage pain, and watch for complications. It’s important to follow these instructions to recover smoothly.
Hospital Stay Duration
The time you spend in the hospital after angioplasty or stenting varies. Many patients go home the same day or the next. But, some might need to stay longer if they have complications or need more observation.
|
Procedure Type |
Typical Hospital Stay |
|---|---|
|
Angioplasty |
Same day or 1 day |
|
Stenting |
1-2 days |
Activity Restrictions
For a few days after the procedure, avoid heavy lifting, bending, or hard work. Gentle walking is okay to help healing and prevent blood clots. Your doctor will tell you when it’s safe to go back to normal activities, like work and exercise.
Long-term Medication Requirements
After angioplasty or stenting, you’ll likely take antiplatelet medications to keep the stent clear of clots. Taking these medications as directed is important to avoid problems. Your doctor will tell you how long you need to take them.
It’s also important to make lifestyle changes. Eat well, exercise regularly, and quit smoking. These habits help with long-term recovery and heart health.
Cost and Insurance Considerations in the US
It’s important for patients to know about the costs of medical procedures like angioplasty or stenting. The prices can change a lot based on where you are, who does the procedure, and your insurance.
Average Costs of Procedures
The cost of angioplasty and stenting can vary a lot in the US. On average, angioplasty can cost between $20,000 to $50,000 or more. This depends on if a stent is used and what kind of stent it is.
Breakdown of Average Costs:
|
Procedure |
Average Cost Range |
|---|---|
|
Angioplasty without Stent |
$20,000 – $30,000 |
|
Angioplasty with Stent |
$30,000 – $50,000 |
|
Stent Placement (additional cost) |
$5,000 – $10,000 |
Financial Assistance Options
For those facing financial hurdles, there are help options. Hospitals, non-profit groups, and drug companies offer financial aid.
Understanding the costs, insurance, and aid can help patients prepare for angioplasty and stenting expenses.
Conclusion
It’s important to know the difference between angioplasty and stent placement for treating heart disease. We’ve seen how these methods help improve heart health and quality of life for those with coronary artery disease.
Angioplasty and stenting have grown a lot, giving patients many choices based on their health needs. Knowing when to use angioplasty alone or with a stent helps patients make better choices for their care.
These treatments are key in managing heart disease, easing symptoms, and improving results for patients. As technology gets better, we’ll see even more improvements in these treatments. This will help more people around the world have better heart health.
FAQ
What is the difference between angioplasty and stenting?
Angioplasty uses a balloon to widen blocked arteries. Stenting places a device to keep the artery open. Both treat blocked arteries but in different ways.
What is a normal resting heart rate?
A normal heart rate is between 60 to 100 beats per minute. It can change with age, fitness, and health.
What are the signs and symptoms of arterial blockage?
Signs include chest pain, shortness of breath, and fatigue. A heart attack is a severe case. Knowing these symptoms is key to getting help fast.
When is angioplasty recommended?
It’s for severe heart disease, heart attacks, or when other treatments fail. The choice depends on the patient’s needs and doctor’s advice.
What are the risks associated with angioplasty?
Risks include bleeding, artery narrowing, and catheter site problems. Knowing these risks helps make informed choices.
What is a stent and how is it used?
A stent is a mesh device in an artery to keep it open. It’s used during or after angioplasty to improve blood flow.
What are the different types of stents available?
There are bare-metal stents and drug-eluting stents. Drug-eluting stents release medicine to prevent artery narrowing.
How is a stent placed?
A stent is placed by guiding a catheter to the artery. The stent is then deployed and checked for correct placement.
What are the risks and complications of stent placement?
Risks include artery narrowing, clotting, and bleeding from antiplatelet therapy. Close monitoring and follow-up care are key to managing these risks.
How do I prepare for angioplasty or stent procedures?
You’ll need to undergo tests, adjust medications, and fast before the procedure. Understanding what to expect helps prepare for the day.
What is the recovery process like after angioplasty and stenting?
Recovery includes immediate care, possibly a hospital stay, and activity limits. Long-term medication and lifestyle changes are also recommended.
How much do angioplasty and stenting procedures cost in the US?
Costs vary by location, insurance, and procedure details. Understanding your insurance and exploring financial help can manage costs.
What is the average cost of angioplasty and stenting procedures?
Costs vary widely. It’s best to check with healthcare providers and insurance for specific estimates. Financial assistance programs may be available.
Are there any long-term medication requirements after angioplasty and stenting?
Yes, long-term antiplatelet therapy and other medications are often needed. Taking the prescribed medication is essential for heart health.
Can angioplasty and stenting be performed together?
Yes, they are often done together. The choice depends on the patient’s condition and the blockage’s severity.
What are the benefits of a combined angioplasty and stenting approach?
This approach can improve outcomes by widening and keeping the artery open. It leads to better blood flow and lower risk of future blockages.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/9062089/





