The British National Formulary (BNF) says cardiac rehabilitation is key after heart procedures. Millions get stents every year. It’s vital to have a full recovery plan.
We think knowing about heart rehabilitation helps patients make better health choices.
After getting a stent, patients often ask what’s next. Cardiovascular rehabilitation programs help. They guide patients back to health and lower heart risk.
We aim to clearly explain why these programs are important and how they help.
Key Takeaways
- Cardiac rehabilitation is a vital component of recovery after stent placement.
- Comprehensive programs support physical and emotional healing.
- Rehabilitation can significantly reduce the risk of future heart issues.
- Personalized care plans are tailored to individual patient needs.
- Participation in rehabilitation programs can improve overall quality of life.
Understanding Stent Procedures and Their Impact

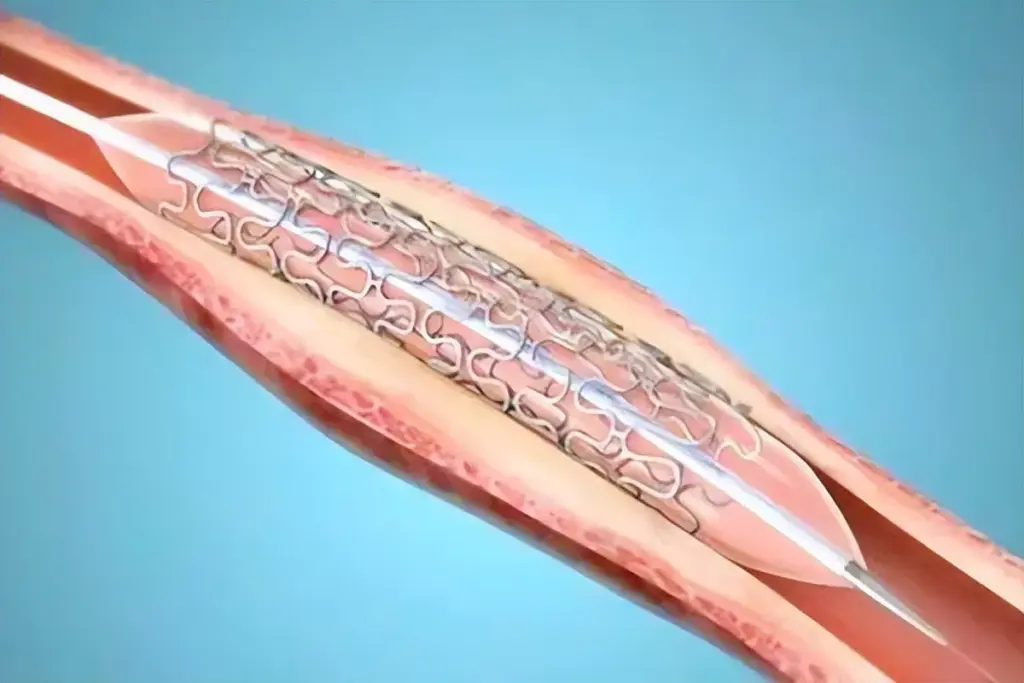
Knowing about stents is key for those with coronary artery disease. A coronary stent is a small, mesh tube. It keeps arteries open, helping blood flow to the heart.
What is a Coronary Stent?
A coronary stent is a medical device for keeping arteries open. It’s made of metal mesh and used in percutaneous coronary intervention (PCI). The stent is placed at blockages to stop arteries from narrowing.
Common Reasons for Stent Placement
Stents are often used for big blockages in coronary arteries. Doctors decide based on symptoms, blockage size, and health. Stent placement helps improve life quality for many patients.
Immediate Post-Procedure Recovery
After stent placement, patients are watched for hours. Most can go home the same or next day. It’s vital to follow doctor’s advice on meds, follow-ups, and lifestyle changes. This helps avoid complications and aids in healing.
The Importance of Cardiac Rehab After Stent Placement
Cardiac rehab after stent placement is very important. It’s part of a full care plan to help patients get better after heart events or procedures. “Cardiac rehabilitation is a medically supervised program to improve cardiovascular health in patients who have experienced heart conditions or procedures,” says the cardiology team.
Definition and Purpose of Rehabilitation
Cardiac rehab is a program with exercise, heart-healthy living education, and stress counseling. Its main goal is to help patients fully recover, improve heart health, and lower future heart risks. By joining a cardiac rehab program, patients can see better heart function and less heart disease symptoms.
Managing heart health and improving life quality are key. Cardiac rehab is customized for each patient, ensuring a personal recovery path.
When Rehabilitation Should Begin
When to start cardiac rehab varies based on health and stent procedure details. Usually, it starts a few days to a week after hospital discharge. Starting early is important for a quicker recovery, helping patients regain strength and confidence.
“Early rehabilitation after cardiac events or procedures is critical for the best recovery,” says a leading cardiologist.
Duration of Typical Rehabilitation Programs
Cardiac rehab programs last several months. They usually range from 12 to 24 weeks, with session frequency decreasing as progress is made. The exact time depends on patient progress, needs, and program structure. Patients are closely monitored, and their progress is checked regularly to adjust the program as needed.
Understanding the importance of cardiac rehab after stent placement helps patients actively participate in their recovery. This improves heart health and overall life quality. We stress the importance of complete care plans with cardiac rehab for the best patient outcomes.
Components of a Complete Cardiac Rehab Program
Cardiac rehabilitation is more than just one thing. It includes medical checks, supervised workouts, and learning new habits. A full cardiac rehab program is key for healing after a stent procedure.
Medical Evaluation and Monitoring
The first step is a detailed medical evaluation. This check-up lets doctors know how you’re doing and what risks you might face. Monitoring keeps going during the program to make sure you’re doing well.
VA health care offers community care for veterans. This includes cardiac rehab services. It shows how important it is to have easy access to medical checks and monitoring.
Supervised Exercise Training
Supervised exercise training is a big part of rehab. It helps you get your heart and body stronger. You’ll work out with experts who make sure you’re doing it right and safely.
Lifestyle Education
Lifestyle education teaches you how to live healthier. You’ll learn about eating right, managing stress, and other things that help your heart. This knowledge helps you make better choices for your health.
Together, medical checks, workouts, and learning new habits make up a complete rehab program. This approach helps patients get the best results for their recovery.
The Medical Perspective: Why Doctors Recommend Cardiac Rehab
Cardiac rehabilitation is essential following stent placement. It’s backed by clinical guidelines and research. Doctors strongly suggest it for patients after stent placement.
Clinical Guidelines and Recommendations
Guidelines say cardiac rehab should include exercise, lifestyle education, and medical checks. This ensures patients get the best care for recovery and long-term health.
Research Supporting Post-Stent Rehabilitation
Studies show cardiac rehab helps patients after stent placement. It improves heart function, lowers future heart risks, and boosts physical strength.
“Cardiac rehabilitation is associated with a significant reduction in mortality and morbidity in patients with coronary artery disease.”
NICE Guidelines
Research shows cardiac rehab improves survival and reduces hospital stays. It also helps manage heart risk factors better.
When Rehabilitation Might Not Be Recommended
Cardiac rehab is usually recommended after a stent. But, some patients might not fit or need special care. This includes those with severe heart failure or unstable angina.
Other factors like patient preference or lack of access can also affect rehab. Doctors work with patients to find the best option for them.
Physical Benefits of Rehabilitation Following Stent Procedures
Cardiac rehabilitation after stent placement offers many benefits. Our team uses advanced tools to understand heart health. We create personalized care plans to support patients fully during their recovery.
Improved Cardiovascular Function
Cardiac rehab boosts cardiovascular function by making the heart more efficient. It increases blood flow too. Patients get to strengthen their heart muscles through supervised exercises, leading to better heart health.
Reduced Risk of Future Cardiac Events
Being part of cardiac rehab programs can reduce the risk of future cardiac events. Patients learn to live healthier and manage risks better. This lowers their chance of another heart problem.
Enhanced Physical Strength and Endurance
Cardiac rehab includes cardiac rehab exercises to boost physical strength and endurance. These exercises help patients regain their physical abilities. They can then confidently return to their daily activities.
Cardiac rehabilitation is key in supporting patients’ recovery and well-being after stent placement. It focuses on these physical benefits.
Psychological and Emotional Benefits of Recovery Programs
Heart health recovery is tough, but cardiac rehab helps a lot. It’s not just about getting better physically. It also deals with the emotional and mental sides of healing after a heart issue.
Managing Anxiety and Depression After Cardiac Procedures
Heart problems can make people feel anxious and depressed. It’s key to handle these feelings during recovery. Cardiac rehab programs offer counseling and stress management to help patients deal with these emotions.
Building Confidence in Physical Activities
Patients often doubt their physical strength after a heart event. Cardiac rehab helps by starting with gentle exercises. This lets patients build confidence in their physical abilities.
Support Networks and Group Dynamics
Support groups are a big part of cardiac rehab. Patients join group sessions. Here, they meet others who’ve faced similar issues, creating a sense of community and understanding.
|
Benefit |
Description |
|---|---|
|
Managing Anxiety |
Counseling and stress management techniques |
|
Building Confidence |
Supervised exercise programs |
|
Support Networks |
Group sessions with peers |
Being part of a cardiac rehab program can change lives. It’s not just about getting better physically. It’s a chance to regain confidence, manage anxiety, and connect with others who get it.
Exercise Components of Cardiac Rehab
Cardiac rehab exercises aim to boost heart health and overall well-being. A structured exercise plan helps patients improve their heart function. It also increases physical strength and endurance, lowering the risk of future heart problems.
Types of Recommended Exercises
Cardiac rehab programs offer various exercises based on each patient’s needs and health. These may include:
- Aerobic exercises like walking, cycling, or swimming to boost heart health
- Resistance training to build muscle strength and endurance
- Flexibility exercises to enhance range of motion and reduce stiffness
Intensity and Progression Guidelines
The exercise intensity in cardiac rehab is set based on the patient’s fitness level and health. Here are the guidelines:
- Start with low to moderate intensity, gradually increasing as the patient gets more fit.
- Progression is based on regular checks of the patient’s exercise ability and health.
- Patients should watch for symptoms and report any concerns to their healthcare team.
Monitoring During Exercise
Monitoring during exercise is key in cardiac rehab to ensure safety and program effectiveness. This includes:
- Continuous ECG monitoring during initial exercise sessions
- Regular blood pressure checks
- Monitoring symptoms like chest pain or shortness of breath
In summary, cardiac rehab exercises are designed to support recovery and health after heart events or procedures. Understanding the types of exercises, intensity guidelines, and monitoring is vital. This way, patients can get the most out of their cardiac rehab program.
Nutritional Guidance and Dietary Changes
Dietary changes are key in cardiac rehab. They help the heart heal and lower the risk of future heart problems. A good diet manages weight, improves cholesterol levels, and controls blood pressure. We stress the need for heart-healthy eating patterns that include lots of fruits, veggies, whole grains, and lean proteins.
Heart-Healthy Eating Patterns
A heart-healthy diet is all about eating foods that are full of nutrients but low in bad fats, salt, and sugar. Here’s what we suggest:
- Eat at least five servings of fruits and veggies a day
- Choose whole grains over refined ones
- Go for lean proteins like poultry, fish, and legumes
- Limit foods high in saturated and trans fats, sodium, and sugar
Dietary Changes to Support Recovery
After a stent, it’s important to make diet changes that help the heart recover. Here’s how:
- Keep sodium intake under 2,300 milligrams a day
- Eat more omega-3 fatty acids from fish, nuts, and seeds
- Drink alcohol in moderation
- Drink plenty of water to stay hydrated
These diet changes help with recovery and keep the heart healthy in the long run.
Managing Cholesterol and Blood Pressure Through Diet
Diet is key in managing cholesterol and blood pressure. Here’s what we recommend:
|
Dietary Component |
Recommendation |
Benefit |
|---|---|---|
|
Saturated and Trans Fats |
Limit intake |
Reduces LDL cholesterol |
|
Fiber |
Increase intake |
Lowers cholesterol levels |
|
Potassium |
Consume potassium-rich foods |
Helps lower blood pressure |
By choosing the right foods, patients can greatly improve their heart health and lower the risk of future heart problems.
Lifestyle Modifications Beyond Exercise and Diet
Comprehensive cardiac rehab programs go beyond just exercise and diet. They focus on lifestyle changes that are key for recovery and long-term health after stent placement.
Smoking Cessation Support
Quitting smoking is a big step in heart health. Smoking greatly increases the risk of heart problems. Cardiac rehab offers help to stop smoking, including:
- Counseling sessions
- Nicotine replacement therapy
- Prescription medications
- Support groups
Stress Management Techniques
Managing stress is also important. Chronic stress can harm the heart. Learning stress-reducing techniques is essential. Some methods include:
- Meditation and mindfulness practices
- Deep breathing exercises
- Yoga and tai chi
- Cognitive-behavioral therapy
Sleep Optimization Strategies
Good sleep is vital for heart health. Improving sleep quality is important. Strategies include:
- Establishing a consistent sleep schedule
- Creating a sleep-conducive environment
- Avoiding caffeine and electronics before bedtime
Medication Adherence
Following medication instructions is critical. Medications like antiplatelet agents and statins help manage heart health after stent placement. Cardiac rehab programs teach patients about their medications and how to take them right.
Insurance Coverage and Access to Cardiac Rehab
Getting insurance for cardiac rehab can be tricky. But it’s key for getting the care you need. We’ll look at how insurance works and what affects your access to these important programs.
Medicare and Private Insurance Coverage
Most insurances, including Medicare, cover cardiac rehab. Medicare Part B usually pays for it if you’ve had a heart attack or surgery. Private insurance might have different rules, so it’s good to check your policy.
“Cardiac rehab is vital for many heart patients,” saysa cardiologist. “Knowing your insurance can help you get into these programs.”
Typical Costs and Financial Considerations
Even with insurance, you might have to pay some out-of-pocket. This could be copays, deductibles, or coinsurance. The cost of rehab can vary a lot, from $1,000 to $5,000 or more.
- Average cost per session: $20 to $100
- Number of sessions: Usually 36 over several months
- Additional costs: Costs for tests, procedures, or extra services
Overcoming Barriers to Participation
Some people can’t get to cardiac rehab because of insurance, transport, or schedules. Many hospitals offer flexible times, help with transport, or home programs.
Veterans can check if the VA covers cardiac rehab. Knowing your options can help you get the care you need.
Working with your doctor and insurance can help you get the rehab you need. It’s important for your recovery and health.
Alternative and Home-Based Rehabilitation Options
Healthcare is changing, and so are the ways we recover after stent placement. Now, more people are choosing alternative and home-based rehab options. These choices are flexible and convenient, making it easier for patients to stick to their rehab plans.
Structured Home Programs
Structured home programs let patients follow a rehab plan from home. They include exercises, diet advice, and tips for a healthier lifestyle. Each plan is made just for the patient’s needs.
Key parts of these programs are initial checks, custom exercise plans, regular checks, and heart-healthy living tips. This structured approach helps patients keep up with their recovery.
Digital and Telehealth Rehabilitation Services
Digital and telehealth services are big steps forward in cardiac rehab. They use online platforms to offer rehab programs from anywhere. This means patients can get support and monitoring in real-time.
Benefits of digital rehab include easier access, more flexibility, and remote monitoring. Studies show digital platforms are being considered for use in places like the NHS for cardiac rehab.
When Home-Based Programs Are Appropriate
Home-based programs work well for many patients. They’re great for those who can’t get to rehab centers easily. This could be because of where they live, mobility issues, or personal reasons.
But, whether home-based programs are right for someone depends on their needs and situation. Doctors look at the patient’s health history, current condition, and what they prefer. This helps decide the best rehab path for each person.
Long-Term Outcomes: Comparing Patients Who Complete Rehab vs. Those Who Don’t
Research shows that patients who finish cardiac rehab after a stent do better in the long run. This section looks at the outcomes for those who stick with rehab and those who don’t.
Survival and Recurrence Rates
Studies show that rehab patients live longer and have fewer heart problems than those who skip rehab. Cardiac rehab’s success comes from its full program of medical checks, exercise, and lifestyle tips.
Quality of Life Differences
Cardiac rehab also boosts patients’ quality of life. Rehab participants feel better physically, have less anxiety and depression, and enjoy life more.
Rehab’s success comes from its wide approach. It helps with physical recovery and also improves mental health and lifestyle. Rehab teaches patients to manage their health, leading to more active and happy lives.
Return to Work and Normal Activities
Cardiac rehab helps patients get back to work and daily activities. It boosts their strength and confidence, making it easier to get back to normal.
- Enhanced physical strength and endurance
- Improved cardiovascular health
- Better management of cardiac risk factors
Patient Testimonials and Case Studies
Patient stories and case studies show rehab’s positive effects. Many say rehab gave them a new sense of purpose and well-being. These stories inspire others to start or continue their rehab journey.
“Cardiac rehab was a game-changer for me. It not only helped me recover physically but also gave me the tools to manage my condition and improve my overall quality of life.”
Looking at the long-term results, it’s clear rehab is key for patients after a stent.
Conclusion: Making an Informed Decision About Post-Stent Rehabilitation
Cardiac rehabilitation after a stent is key to getting better. It helps people understand the benefits and parts of a good rehab program. This way, they can make smart choices about their recovery.
Cardiac rehab is more than just working out. It includes medical checks, learning about lifestyle, and getting mental support. These parts help improve heart health, lower the chance of heart problems, and boost overall health.
When thinking about rehab after a stent, it’s important to consider if it’s right for you. This lets patients play a big role in their healing. It can lead to better health and a happier life in the long run.
Choosing cardiac rehab means knowing its value, what to expect, and the options available. By doing this, people can get the most out of their recovery. They can move forward with hope and confidence.
FAQ
What is cardiac rehabilitation, and why is it necessary after stent placement?
Cardiac rehabilitation is a program that includes medical checks, exercise training, and lifestyle education. It’s needed after stent placement to boost heart function and lower future heart risks. It also improves physical and emotional health.
How long does a typical cardiac rehabilitation program last?
A typical program lasts from weeks to months, usually around 12 weeks. It depends on individual needs and progress.
What are the benefits of starting cardiac rehab early after stent placement?
Starting early improves heart function and reduces anxiety and depression. It also boosts recovery and helps build confidence and healthy habits.
What types of exercises are recommended in cardiac rehab?
Exercises include walking, cycling, resistance training, and flexibility exercises. They’re tailored to each person’s needs and monitored by healthcare professionals.
Will I be monitored during exercise in cardiac rehab?
Yes, you’ll be closely watched during exercise. This includes checking heart rate, blood pressure, and ECG readings for safety and effectiveness.
How does cardiac rehab help with managing anxiety and depression?
It offers a supportive environment for sharing experiences and connecting with others. Education on stress management also helps manage anxiety and depression.
Is cardiac rehab covered by insurance?
Many insurance plans, including Medicare, cover cardiac rehab. But coverage varies by provider and policy. Always check with your insurance.
Can I participate in cardiac rehab if I have other health conditions?
Programs are tailored for various health conditions. But some conditions may need special attention. Always discuss your health with your healthcare provider.
Are there alternative or home-based cardiac rehab options?
Yes, there are home-based and digital/telehealth options. They’re good for those who can’t go to traditional programs.
How does cardiac rehab impact long-term outcomes after stent placement?
Completing cardiac rehab improves long-term outcomes. It reduces mortality rates, enhances quality of life, and lowers future heart risks. Many patients see a positive impact on their well-being.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC7262778/[4








