Neurology diagnoses and treats disorders of the nervous system, including the brain, spinal cord, and nerves, as well as thought and memory.
Send us all your questions or requests, and our expert team will assist you.
Diagnosis and imaging in neurosurgery are focused on identifying structural abnormalities of the nervous system, determining their functional impact, and assessing whether surgical intervention is necessary. Because neurosurgical conditions often involve delicate neural tissue, precise diagnosis is essential to balance potential benefits of surgery against associated risks.
The diagnostic process aims to localize pathology accurately, understand its progression, and guide safe and effective treatment planning.

Clinical evaluation guides imaging decisions.
The diagnostic process begins with a detailed neurological examination to assess how symptoms relate to specific areas of the nervous system. This examination helps determine whether a structural cause is likely and which regions require further evaluation.
Clinical assessment typically evaluates
• Motor strength and coordination
• Sensory function and reflexes
• Cranial nerve integrity
• Cognitive and speech function
• Gait and balance
Findings from this examination shape the imaging strategy.

Context clarifies imaging findings.
A thorough medical history provides insight into the timing, triggers, and progression of neurological symptoms. Sudden onset may suggest acute structural events, while gradual progression may indicate degenerative or compressive processes.
Historical details assist in narrowing diagnostic possibilities and avoiding unnecessary procedures.
Visualization defines surgical planning.
Imaging allows direct visualization of the brain, spinal cord, and surrounding structures, making it central to neurosurgical diagnosis. It helps identify lesions, compression, instability, or vascular abnormalities that may require intervention.
Imaging supports
• Localization of pathology
• Assessment of severity and extent
• Evaluation of surgical accessibility
• Monitoring of disease progression
Accurate imaging is critical for safe decision-making.

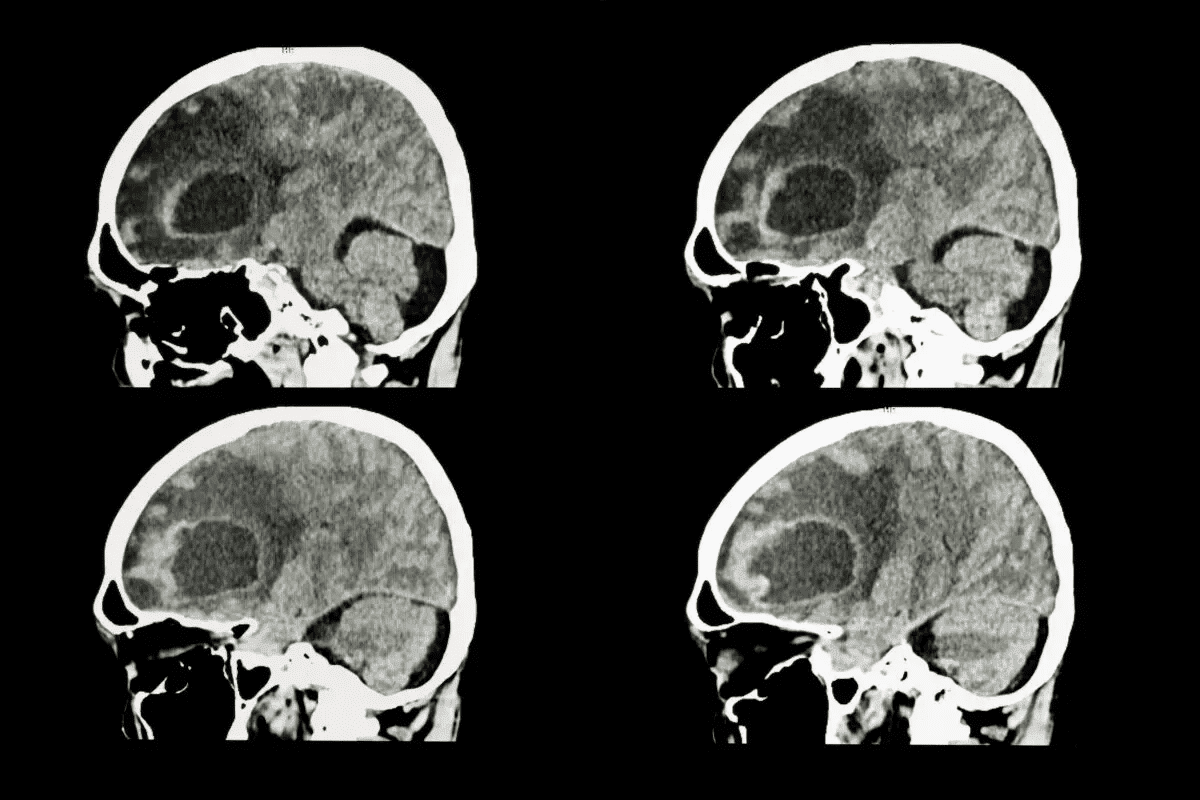
The brain requires detailed assessment.
Imaging of the brain is used to assess conditions affecting brain tissue, ventricles, and surrounding membranes. It helps identify abnormalities that may cause seizures, headaches, cognitive changes, or focal neurological deficits.
Brain imaging assists in understanding both structural and secondary effects such as pressure or displacement.
Spinal anatomy demands precision.
Spinal imaging evaluates the relationship between the spinal cord, nerve roots, discs, and vertebral column. It is essential for diagnosing conditions that cause pain, weakness, or sensory loss.
Spinal imaging helps determine
• Presence of compression or instability
• Extent of neural involvement
• Relationship between bone and neural structures
This information is critical for surgical planning.
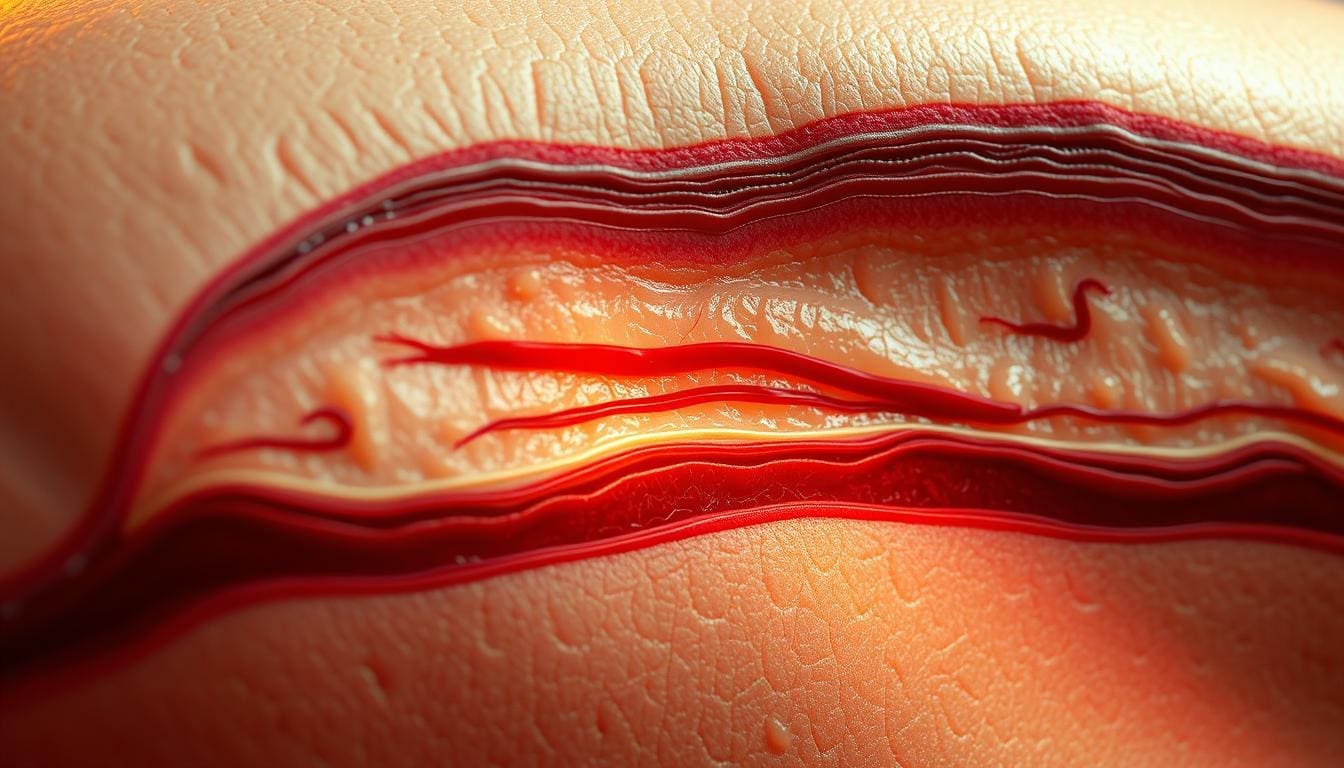
Blood flow affects neural survival.
When vascular abnormalities are suspected, specialized imaging helps evaluate blood vessels supplying the brain and spinal cord. These studies assist in identifying abnormal vessel structure or flow patterns that may pose neurological risk.
Vascular imaging supports risk assessment and intervention planning.
Images must match symptoms.
Imaging findings are always interpreted alongside clinical symptoms and examination results. Not all structural abnormalities cause symptoms, and correlation helps avoid unnecessary surgical intervention.
Functional relevance guides treatment decisions.
Planning minimizes risk.
Imaging provides detailed anatomical information that informs surgical approach, technique, and risk assessment. Precise planning reduces operative risk and supports preservation of neurological function.
Surgical planning relies heavily on imaging accuracy.
Diagnosis continues over time.
Follow-up imaging may be used to monitor disease progression, assess response to non-surgical management, or plan timing of surgical intervention. Changes on imaging are evaluated in relation to symptom evolution.
Ongoing assessment supports timely care.
Complex anatomy complicates diagnosis.
Neurosurgical diagnosis often involves complex anatomy and overlapping conditions. Careful interpretation of imaging, combined with clinical judgment, reduces the risk of misdiagnosis and inappropriate intervention.
Expert evaluation supports accuracy.

Send us all your questions or requests, and our expert team will assist you.
Yes, imaging is essential for surgical planning.
Yes, not all structural findings require surgery.
No, decisions are based on imaging and clinical context.
Yes, especially for monitoring progression or planning timing.
Because surgery targets functional impact, not images alone.


Skull base surgery is a highly complex and delicate procedure. It involves operating on a crowded area of the skull. This area is home to
Nearly 2,000 people in the United States are diagnosed with a rare type of tumor at the cranial base each year. The complexity of cranial

Neurosurgery needs careful anesthetic management to keep patients safe and get the best results. Choosing the right anesthetic is key. Knowing the different anesthesia protocols


Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)