
Nearly 900,000 Americans face blood clots each year. Many cases are linked to certain medicines. It’s key to know the risks to prevent and treat them on time.
Some medications raise the risk of blood clots a lot. These include many prescription drugs for different health issues.
Key Takeaways
- Certain medications can increase the risk of blood clot formation.
- Understanding the risks is key for prevention.
- Prescription drugs for various conditions can be linked to blood clots.
- Awareness of medications linked to blood clots helps in timely treatment.
- Knowing about blood clotting medications is vital for patient safety.
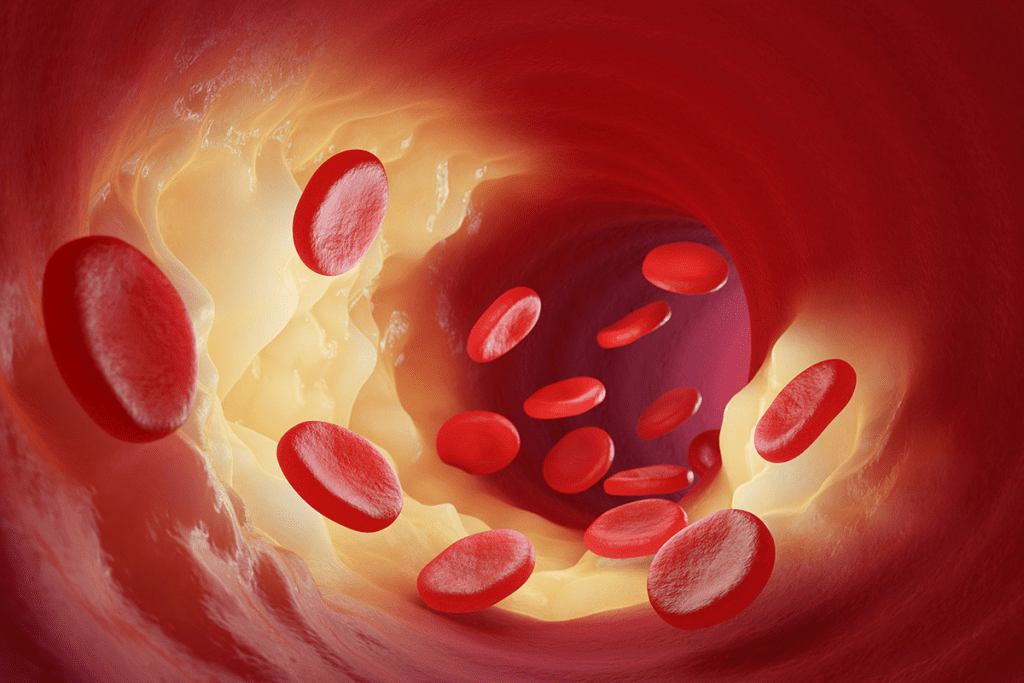
Understanding Blood Clots and Their Formation
Blood clots form when platelets and proteins in the blood stick together. This is a natural process that helps stop bleeding when a blood vessel is hurt. But, it can become harmful under certain conditions.
The Normal Blood Clotting Process
The normal clotting process starts when a blood vessel is damaged. Platelets stick to the damaged area and release signals for more platelets. This leads to the formation of fibrin, making the clot stable.
Pathological Blood Clot Formation
Pathological clots form without injury inside a blood vessel. They can be caused by genetics, medical conditions, or certain drugs. These clots can block blood flow, causing serious problems like DVT, PE, and stroke.
Types of Blood Clots and Their Locations
Blood clots can occur in different places, like the legs, lungs, or brain. The location and type of clot affect the severity and treatment. Knowing about these clots is key to diagnosing and treating them.
How Medications Influence Blood Clotting Mechanisms
Medications and blood clotting have a complex relationship. They can change how blood clots, affecting blood vessels and platelets. Some drugs can make clotting better or worse.
Medication Effects on Coagulation Pathways
Medications can change the coagulation cascade. This is a series of reactions that form blood clots. Anticoagulant medications stop clots by blocking certain factors. But, some drugs might make clotting riskier by boosting certain factors.
Medication-Induced Changes in Blood Vessel Walls
Some drugs can alter blood vessel walls. This can lead to changes that help or hinder clotting. For example, vasoconstrictors can make vessels narrower, raising clot risk due to higher pressure.
Impact on Platelet Function and Aggregation
Platelets are key in clotting. Some drugs, like antiplatelet drugs, stop platelets from clumping. But, other drugs might make platelets more likely to form clots.
Understanding how drugs impact blood clotting mechanisms is crucial for effective patient management. This helps manage risks tied to pharmaceuticals and blood clot risks. Doctors must balance medication benefits with risks, including clotting risks.
Hormonal Medications and Blood Clot Risks
Hormonal medications are linked to blood clots. They’re used for menopause symptoms, birth control, and reproductive issues. But, these treatments can raise the risk of blood clots.
Combined Oral Contraceptives
Combined oral contraceptives (COCs) contain estrogen and progestin. They increase the risk of blood clots. The risk is highest in the first year and depends on the progestin type and estrogen dose.
Women on COCs should watch for blood clot symptoms. If they notice anything unusual, they should see a doctor.
Risk factors for blood clots in COC users include smoking, obesity, and family history of blood clots. Doctors should consider these before prescribing COCs.
Hormone Replacement Therapy (HRT)
Hormone replacement therapy (HRT) is used for menopause symptoms. It also raises blood clot risk, most in the first year. Oral HRT is riskier than transdermal HRT.
The type of HRT matters too. HRT with estrogen and progestogen is riskier than estrogen alone.
Monitoring patients on HRT for blood clot signs is key. This is true for those with mobility issues or clotting history.
Selective Estrogen Receptor Modulators (SERMs)
SERMs are used for osteoporosis and sometimes breast cancer. They can affect blood clot risk, but the overall benefit must be weighed for each patient.
Doctors should talk to patients about SERM risks and benefits. This is important for those with clotting history or other risk factors.
Cancer Treatments Associated with Blood Clots
Certain cancer therapies can increase the risk of blood clots, a serious condition. These treatments save lives but can have side effects like blood clotting.
Chemotherapy Agents
Chemotherapy is a common cancer treatment. But, some chemotherapy agents raise the risk of blood clots. For example, L-asparaginase used in treating acute lymphoblastic leukemia can significantly increase the risk of thrombosis.
Targeted Cancer Therapies
Targeted therapies aim to target specific cancer cells. They can affect the body’s clotting mechanisms. For instance, bevacizumab, used in treating various cancers including colorectal and lung cancer, has been linked to an increased risk of arterial thromboembolic events.
Hormone Therapies for Cancer
Hormone therapies are used in treating hormone-sensitive cancers like breast and prostate cancer. They can also affect blood clot risk. Tamoxifen and aromatase inhibitors are examples of hormone therapies that have been associated with an increased risk of thrombosis.
The following table summarizes the cancer treatments associated with blood clots:
| Treatment Type | Examples | Associated Risk |
| Chemotherapy | L-asparaginase | Increased risk of thrombosis |
| Targeted Therapy | Bevacizumab | Arterial thromboembolic events |
| Hormone Therapy | Tamoxifen, Aromatase inhibitors | Increased risk of thrombosis |
It’s important to understand the risks of cancer treatments. Healthcare providers must weigh the benefits against the risks, including blood clots.
Cardiovascular Medications and Thrombosis Risk
Certain cardiovascular medications can increase the risk of blood clots. This is why it’s important to watch patients closely. These drugs help manage heart conditions but can also cause blood clots.
Antihypertensive Medications
These drugs treat high blood pressure, a big risk for heart disease. While mostly safe, some can raise the risk of blood clots. For example, some beta-blockers might affect how blood clots.
Antiarrhythmic Drugs
These drugs help control irregular heartbeats. Some, like Class III, can increase the risk of blood clots. This is because they can make the heart’s rhythm more unstable.
Statins and Other Lipid-Lowering Agents
Statins are used to lower cholesterol and reduce heart disease risk. They are mostly safe but can affect blood clotting in complex ways. Some studies show they might lower the risk of blood clots, while others have little effect.
Vasoconstrictors and Vasodilators
These drugs are used for conditions like angina and high blood pressure. Vasoconstrictors can raise blood pressure and increase the risk of blood clots. On the other hand, vasodilators can lower blood pressure and might protect against blood clots.
| Medication Class | Effect on Thrombosis Risk |
| Antihypertensive Medications | Variable; some may increase risk |
| Antiarrhythmic Drugs | Some may increase risk, particular Class III |
| Statins | Generally reduce risk, but effects can vary |
| Vasoconstrictors | May increase risk |
| Vasodilators | May reduce risk |
A cardiovascular expert notes, “Using these medications is a delicate balance. We need to manage heart risks while avoiding blood clots.”
“Managing heart disease with medications is complex. We must weigh the risks and benefits carefully.”
Cardiovascular Research Journal
Psychiatric Medications Linked to Blood Clots
Psychiatric medications are key in treating mental health issues. Yet, they can increase the risk of blood clots in some patients. This is a big worry because many people have these conditions and blood clotting issues.
The link between these medications and blood clots is complex. Some drugs can change how blood clots by affecting different body processes.
Antipsychotic Medications
Antipsychotics help with schizophrenia and bipolar disorder. But, they can also raise the risk of blood clots. Some types of these drugs are more likely to cause this problem.
- Increased Risk: People taking these drugs should watch for signs of deep vein thrombosis.
- Mechanism: It’s not fully understood, but it might be due to the drugs’ effects on blood and clotting factors.
Antidepressants
Some antidepressants, like SSRIs, can lead to bleeding and clotting issues. This is a bit strange, but it’s a known side effect.
- SSRIs might affect how platelets work, which could increase bleeding risk.
- Clotting risk can also depend on the patient, including their genes.
Mood Stabilizers
Mood stabilizers, like lithium, are for bipolar disorder. Their direct link to blood clots is not as clear. But, they can affect body processes that might raise clot risk.
Monitoring: It’s important to watch for any signs of blood clotting in people taking mood stabilizers.
Drugs That Cause Blood Clots: Over-the-Counter Medications
Many people use OTC medications without thinking about the risks. Some of these drugs can increase the chance of blood clots. It’s important to know the risks of certain OTC drugs.
NSAIDs and Blood Clot Risk
NSAIDs help with pain and reduce swelling. But, some NSAIDs can raise blood clot risk. It’s key to use them as directed to avoid problems.
Decongestants and Vasoconstriction
Decongestants in cold and allergy meds can narrow blood vessels. This might raise blood pressure and clot risk. Be careful, if you have high blood pressure or heart disease.
Supplements with Clotting Effects
Some supplements can affect blood clotting. Herbal supplements might interact with blood thinners or affect clotting. Always talk to a doctor before taking new supplements, if you’re on blood thinners.
In summary, OTC meds are handy but can pose risks. Knowing these risks helps us use them safely. This way, we can lower our chance of blood clots.
Immunomodulatory Drugs and Blood Clot Formation
Immunomodulatory drugs help control the immune system. They are used for treating autoimmune diseases, cancers, and preventing transplant rejections. But, they can also increase the risk of blood clots.
Corticosteroids
Corticosteroids are known for their anti-inflammatory and immune-suppressing effects. Yet, long-term or high-dose use can raise the risk of blood clots. It’s thought that they affect the blood’s clotting process and boost clotting factors.
Biologics and Targeted Immunotherapies
Biologic agents, like monoclonal antibodies and TNF inhibitors, have changed how we treat autoimmune diseases and some cancers. While mostly safe, some biologics may increase the risk of blood clots. The risk depends on the drug and the patient.
Thalidomide and Related Compounds
Thalidomide is mainly used for treating multiple myeloma and comes with a high risk of blood clots. This risk is even higher when it’s used with other drugs like dexamethasone or chemotherapy. Lenalidomide and pomalidomide, thalidomide’s relatives, also pose a risk of blood clots, making it important to prevent them in high-risk patients.
| Drug Class | Examples | Thrombosis Risk |
| Corticosteroids | Prednisone, Methylprednisolone | Increased with long-term or high-dose use |
| Biologics | TNF inhibitors (Etanercept), Monoclonal antibodies (Rituximab) | Varies by agent and patient population |
| Thalidomide and derivatives | Thalidomide, Lenalidomide, Pomalidomide | Significant risk, specially in combination therapies |
COVID-19 Vaccines and Blood Clot Concerns
COVID-19 vaccines have been key in fighting the pandemic. But, worries have grown about their link to blood clots. It’s vital to know the risks and benefits of these vaccines.
Understanding Vaccine-Induced Immune Thrombotic Thrombocytopenia
Vaccine-induced immune thrombotic thrombocytopenia (VITT) is a rare but serious issue. It causes blood clots and low platelet counts. Research on VITT shows the need to spot its symptoms and understand it to manage risks.
Adenovirus Vector Vaccines and Clotting Risk
Adenovirus vector vaccines, like the AstraZeneca vaccine, have been linked to a higher risk of blood clots. Though rare, it’s key for doctors to know about this risk.
mRNA Vaccines Safety Profile
mRNA vaccines, from Pfizer-BioNTech and Moderna, have a different safety record. They have side effects, but blood clot risks are much lower. Ongoing studies keep checking their long-term safety.
Risk-Benefit Analysis in Context
When looking at COVID-19 vaccines, weighing risks and benefits is key. Vaccines help prevent severe COVID-19 and stop it from spreading. But, for some, like those at risk for blood clots, a closer look is needed.
| Vaccine Type | Associated Risk | Frequency |
| Adenovirus Vector | Thrombosis with Thrombocytopenia Syndrome (TTS) | Rare |
| mRNA Vaccines | Low risk of blood clot-related issues | Very Low |
Studying COVID-19 vaccines helps us understand their safety better. As new data comes in, health guidelines get updated. This ensures people get the most accurate and timely info.
Anticoagulant Medications: When Blood Thinners Cause Clots
Anticoagulants are meant to stop blood clots. But, some can actually make clots more likely. This is a big deal for doctors to know, as it affects how they treat patients.
Heparin-Induced Thrombocytopenia
Heparin-induced thrombocytopenia (HIT) is a serious problem. It happens in some people taking heparin. Despite low platelets, HIT increases the risk of blood clots.
Key Features of HIT:
- Thrombocytopenia after heparin exposure
- Presence of anti-heparin/PF4 antibodies
- High risk of new or progressive thrombosis
Warfarin-Induced Skin Necrosis
Warfarin-induced skin necrosis is rare but serious. It happens early in treatment and causes skin lesions. It’s thought to be due to warfarin’s initial effect of increasing clot risk before it starts to thin blood.
Direct Oral Anticoagulants (DOACs) and Paradoxical Clotting
DOACs are popular because they’re easy to use and don’t need constant monitoring. But, there are reports of clotting problems with them, though it’s rare.
| Anticoagulant | Mechanism of Action | Associated Clotting Risk |
| Heparin | Activates antithrombin | HIT |
| Warfarin | Inhibits vitamin K-dependent clotting factors | Warfarin-induced skin necrosis |
| DOACs (e.g., rivaroxaban, apixaban) | Directly inhibits thrombin or factor Xa | Paradoxical clotting |
In conclusion, anticoagulants are key in preventing blood clots. But, they can also cause problems. Knowing this helps doctors take better care of their patients.
Risk Factors That Increase Medication-Induced Clot Likelihood
It’s important to know what increases the chance of blood clots from medicines. Some people are more at risk because of their genes, health, and lifestyle.
Genetic Predispositions
Genetics can make some people more likely to get blood clots from medicines. Those with conditions like Factor V Leiden or prothrombin gene mutation face a higher risk.
Pre-existing Medical Conditions
Having certain health issues can also raise the risk of blood clots. For example, cancer, heart disease, and obesity can make clots more likely, even with medicine.
Lifestyle Factors
Smoking and staying in bed for a long time can also increase the risk. People who smoke or are bedridden for a while are more at risk.
Drug Interactions That Enhance Clotting Risk
Some medicines can make blood clotting worse when taken together. This can lead to serious health problems.
Doctors need to think about these risks when prescribing medicines. By understanding the role of genes, health, and lifestyle, they can help keep patients safe.
Recognizing Signs and Symptoms of Medication-Induced Blood Clots
It’s important to know the signs of blood clots caused by medication. These clots can happen anywhere in the body. Knowing the symptoms helps get medical help fast.
Deep Vein Thrombosis Symptoms
Deep vein thrombosis (DVT) is a blood clot in the deep veins, usually in the legs. You might notice swelling, pain, or tenderness in your leg. The skin might also feel warm or look red.
Pulmonary Embolism Warning Signs
A pulmonary embolism (PE) is when a blood clot goes to the lungs. This can block blood flow. Look out for sudden shortness of breath, chest pain, and coughing up blood.
Cerebral Venous Thrombosis Indicators
Cerebral venous thrombosis (CVT) is a blood clot in the brain’s sinuses. You might have a severe headache, feel confused, have seizures, or see changes in your vision.
When to Seek Emergency Medical Attention
If you have severe chest pain, trouble breathing, a bad headache, or swelling and pain in your limbs, call for emergency help. Quick medical care is key to treating blood clots.
| Condition | Common Symptoms |
| Deep Vein Thrombosis | Swelling, pain, warmth, or redness in the affected limb |
| Pulmonary Embolism | Sudden shortness of breath, chest pain, coughing up blood |
| Cerebral Venous Thrombosis | Severe headache, confusion, seizures, vision changes |
Monitoring and Prevention Strategies for High-Risk Patients
To lower the risk of blood clots, healthcare providers must use strong monitoring and prevention plans for high-risk patients. This includes medical checks, preventive steps, and lifestyle changes.
Medical Monitoring Protocols
High-risk patients need regular health checks to watch their condition and change treatment plans if needed. This includes:
- Regular blood tests to check for clotting factors and platelet count
- Imaging tests such as ultrasound or CT scans to detect any clot formation
- Monitoring for signs and symptoms of blood clots, such as swelling, pain, or shortness of breath
Table: Medical Monitoring Protocols for High-Risk Patients
| Monitoring Protocol | Description | Frequency |
| Blood Tests | Checking clotting factors and platelet count | Every 3 months |
| Imaging Tests | Ultrasound or CT scans to detect clot formation | As needed based on symptoms |
| Symptom Monitoring | Checking for signs of blood clots | Ongoing |
Preventive Anticoagulation Approaches
For some high-risk patients, preventive anticoagulation therapy may be recommended. This involves the use of anticoagulant medications to prevent the formation of blood clots.
Anticoagulant medications can be taken orally or injected, depending on the patient’s needs and medical history. The healthcare provider will choose the anticoagulant and dosage based on the patient’s individual factors.
Lifestyle Modifications to Reduce Risk
Lifestyle changes can also play a big role in reducing the risk of blood clots. High-risk patients are advised to:
- Stay hydrated by drinking plenty of water
- Engage in regular physical activity, such as walking or swimming
- Avoid prolonged periods of immobility
- Maintain a healthy weight
Alternative Medication Options
In some cases, alternative medications may be considered for high-risk patients to minimize the risk of blood clots. This could involve switching to a different medication or adjusting the dosage of the current medication.
By implementing these monitoring and prevention strategies, healthcare providers can significantly reduce the risk of medication-induced blood clots in high-risk patients.
Conclusion: Balancing Medication Benefits and Blood Clot Risks
It’s important to balance the good and bad of medications to avoid blood clots. Some drugs, like hormonal treatments and cancer therapies, can increase the risk of blood clots. Knowing these risks is key for doctors and patients.
Thinking carefully about the benefits and risks of medications can help avoid problems. Doctors need to consider the good a drug does and its chance of causing blood clots, mainly for those at high risk. This helps them choose the best treatment and how to watch for side effects.
Patients should watch for signs of blood clots and get help if they notice anything odd. Working together, doctors and patients can lower the risks of medications. This way, they can get the most out of treatment while staying safe.
FAQ
What are the most common medications associated with blood clots?
Medications that can lead to blood clots include hormonal contraceptives and hormone replacement therapy. Also, some chemotherapy agents and psychiatric drugs like antipsychotics and antidepressants are linked to this risk.
How do hormonal medications increase the risk of blood clots?
Hormonal medications, like birth control pills and hormone therapy, can make blood clot more easily. They do this by changing how blood clots and affecting clotting factors.
Can cancer treatments cause blood clots?
Yes, some cancer treatments can raise the risk of blood clots. This includes chemotherapy and hormone therapies. They can damage blood vessels and change how blood clots, affecting platelets.
Are there any cardiovascular medications that can cause blood clots?
Yes, certain heart medications can increase blood clot risk. This includes drugs for high blood pressure and irregular heartbeats. These risks are higher for people with heart problems.
How do anticoagulant medications sometimes cause blood clots?
Anticoagulants, like heparin and warfarin, can sometimes cause blood clots. This is rare but can happen due to conditions like heparin-induced thrombocytopenia or warfarin-induced skin necrosis.
What are the signs and symptoms of a medication-induced blood clot?
Signs of a blood clot from medication include swelling and pain in the legs. You might also feel short of breath or have chest pain. Severe headaches or confusion are also symptoms.
How can the risk of medication-induced blood clots be minimized?
To lower the risk of blood clots from medication, monitor your health closely. Use preventive treatments when needed. Make healthy lifestyle choices and consider other medication options for those at high risk.
What lifestyle factors can increase the risk of medication-induced blood clots?
Lifestyle choices that raise the risk of blood clots include smoking and being overweight. Not being active and staying immobile for long periods also increase the risk.
Can genetic predispositions play a role in medication-induced blood clots?
Yes, genetic factors like factor V Leiden or prothrombin gene mutations can increase blood clot risk. They affect how blood clots.
How do COVID-19 vaccines relate to blood clot concerns?
Some COVID-19 vaccines, like those using adenovirus vectors, have been linked to rare cases of blood clotting. This is due to a condition called vaccine-induced immune thrombotic thrombocytopenia.
References
UK National Health Service (NHS) “ Side effects of anticoagulant medicines including potential paradoxical clotting risks
https://www.nhs.uk/medicines/anticoagulants/side-effects




































