Last Updated on December 3, 2025 by Bilal Hasdemir

Deciding to stop chemotherapy is complex and personal. It involves looking at how well the treatment works and its side effects. These factors affect the patient’s life quality.
Oncologists might stop chemo if it’s not working well anymore. Or if the bad effects are too much. Making this choice needs a good understanding of the patient’s health, past treatments, and what they want.
Key Takeaways
- Oncologists consider multiple factors when deciding to stop chemotherapy.
- The decision to discontinue treatment is highly individualized.
- Factors influencing this decision include treatment effectiveness and side effects.
- Patient quality of life plays a crucial role in this decision.
- Oncologists work closely with patients to determine the best course of action.
The Purpose and Goals of Chemotherapy Treatmen
It’s important for patients to understand what chemotherapy aims to do. This treatment can be used in different ways, depending on the cancer type, stage, and the patient’s health.
How Chemotherapy Works Against Cancer Cells
Chemotherapy targets cells that grow fast, like most cancer cells. It uses drugs to kill or slow down these cells. The success of chemotherapy depends on the cancer type and how well the drugs work. It’s especially useful for treating some types of tumors.
Curative vs. Palliative Treatment Intentions
Chemotherapy has two main goals: curative and palliative. Curative chemotherapy tries to get rid of the cancer, aiming for a cure or longer life. Palliative chemotherapy, on the other hand, aims to ease symptoms and improve life quality, especially when a cure is unlikely. Knowing these goals helps set realistic hopes.
Standard Duration of Different Chemotherapy Protocols
How long chemotherapy lasts varies a lot. It depends on the cancer type, treatment goals, and the patient’s health. For example, chemotherapy for breast cancer might last months, while for advanced cancer, it can go on until it stops working. It’s key to regularly check how long chemotherapy should last for each person.
Medical Criteria for Stopping Chemotherapy

Doctors decide to stop chemotherapy based on several important factors. These factors help them know if the treatment is working or if it’s time to try something else.
Successful Completion of Planned Treatment Course
Chemotherapy often stops when the planned treatment is finished. This decision depends on the cancer type, stage, and how well the patient responds. For example, in early-stage breast cancer, treatment might end after 4 to 6 cycles.
A study in the Journal of Clinical Oncology shows that finishing chemotherapy as planned can improve survival. The table below shows how long chemotherapy usually lasts for different cancers.
| Type of Cancer | Typical Chemotherapy Duration |
| Early-stage Breast Cancer | 4-6 cycles (3-6 months) |
| Advanced Colorectal Cancer | Until disease progression or intolerance |
| Testicular Cancer | 3-4 cycles (9-12 weeks) |
Achievement of Cancer Remission
Chemotherapy stops when a patient reaches remission. Remission means a big drop or complete disappearance of cancer signs. Doctors use tests like CT scans and lab tests to check for this.
“The goal of chemotherapy is to achieve a complete response, where there is no evidence of disease. When this is achieved, we can consider stopping treatment,” says, a medical oncologist.
Even if remission is reached, it doesn’t always mean the cancer is gone for good. But it shows the treatment is working, keeping the cancer in check.
Disease Progression Despite Active Treatment
Chemotherapy stops when the disease gets worse despite treatment. This means tumors grow, new metastases appear, or symptoms worsen. At this point, the same treatment won’t help much and could cause more harm.
A study in the Journal of Clinical Oncology suggests changing treatments or joining clinical trials might help more.
Understanding these criteria helps patients and families grasp why chemotherapy might stop. It’s a detailed process that looks at many factors, like treatment goals, patient health, and the balance of benefits and risks.
Intolerable Side Effects Leading to Treatment Cessation
Side effects that are too hard to handle can lead to stopping chemotherapy. This choice is made after careful thought. When the side effects are too severe, doctors and patients must think about the treatment’s benefits and risks.
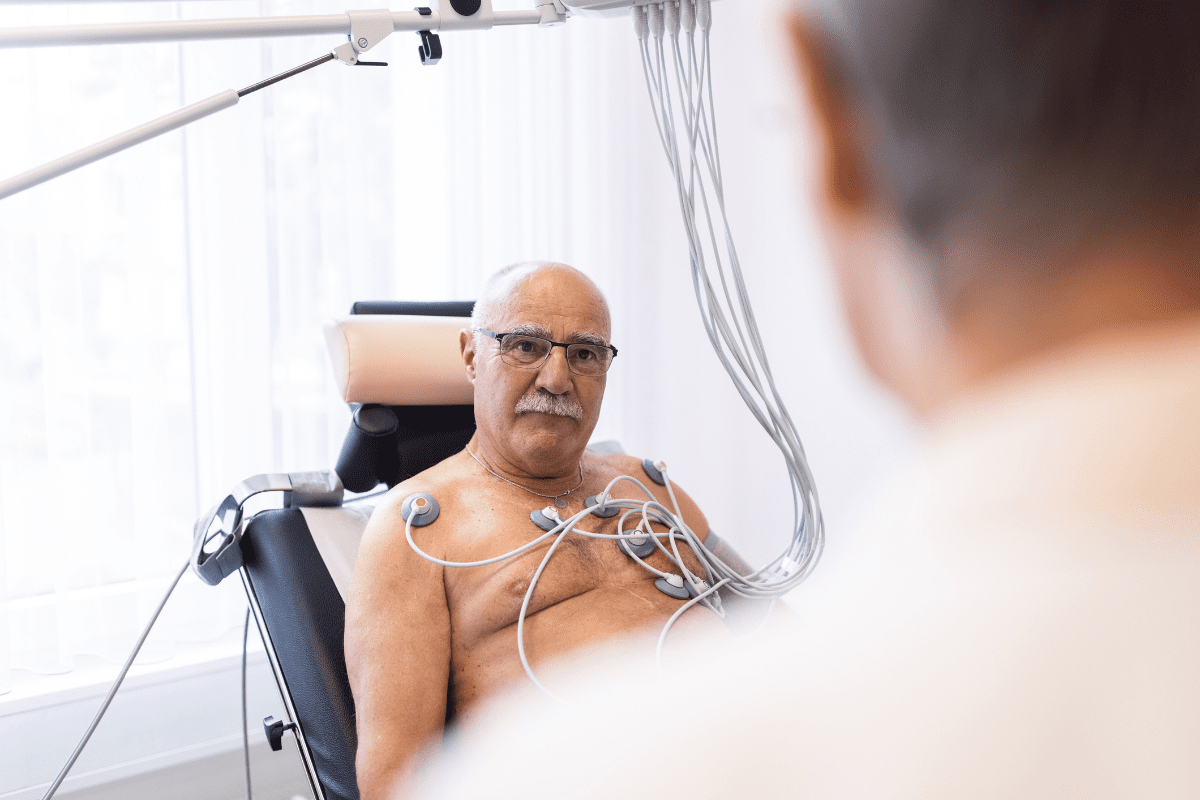
Severe Organ Toxicity and Damage

Chemotherapy can harm vital organs like the heart, kidneys, and liver. If organ damage is found, the risks of continuing treatment might be too high. For example, some treatments can harm the heart, leading to failure if not treated quickly.
It’s important to check organ function regularly. This helps doctors decide if treatment should continue or stop.
Declining Performance Status
A patient’s performance status is key in seeing if they can handle chemotherapy. If a patient’s status drops a lot, it might mean they can’t handle treatment anymore. It could also mean their health is getting worse, even with treatment.
When a patient’s status goes down, they might feel more tired, lose weight, or have trouble doing everyday things. At this point, care might focus more on making the patient comfortable, rather than trying to cure them.
When Risks Outweigh Potential Benefits
Stopping chemotherapy is often chosen when the risks are too high. Doctors look at the patient’s health, how bad the side effects are, and if treatment will work.
In some cases, the risks of continued chemotherapy include physical side effects, emotional strain, and financial burden. When these are considered, stopping treatment is done to protect the patient’s dignity and comfort.
Patient-Driven Reasons for Stopping Chemotherapy
Many factors influence a patient’s choice to stop chemotherapy. These include personal, financial, and social aspects. They all play a role in deciding whether to continue or stop treatment.
Personal Values and Treatment Goals Reassessment
Patients’ personal values and goals are key in making this decision. An oncologist, notes that patients often reassess their priorities during treatment. This can lead to a decision to stop chemotherapy.
They consider the benefits and risks of treatment. They also think about how it affects their quality of life.
“The most important thing is to understand what the patient wants. It’s not just about the treatment; it’s about their life, their family, and their priorities.” –
An Oncologist
Important factors include:
- The impact on personal relationships and family dynamics
- The desire to maintain independence and autonomy
- The need to prioritize comfort and quality of life
Financial and Logistical Burden Considerations
Chemotherapy can be very expensive and logistically challenging. Patients must think about the costs of treatment, travel, and accommodations. They also consider how it affects their job and daily life.
| Financial Burden | Logistical Burden |
| Treatment costs | Travel and accommodations |
| Loss of income | Time spent in treatment |
| Medical expenses | Caregiver responsibilities |
The table shows the financial and logistical challenges. These can make patients think twice about their treatment options.
Family Support System Capacity
The strength of a patient’s family support system is crucial. Patients with strong support may choose to continue treatment. Those with less support may need to look at other options.
Stopping chemotherapy is a personal decision. It’s influenced by many factors. Healthcare providers can better support patients by understanding these reasons.
How Oncologists Evaluate When to Stop Chemotherapy
Oncologists use many factors to decide when to stop chemotherapy. This choice is very important. It aims to get the best results for the patient.
Tumor Response Assessment Methods
One key way to check if chemotherapy is working is by looking at the tumor. Doctors use CT scans, MRI, and PET scans to measure the tumor’s size. Response Evaluation Criteria in Solid Tumors (RECIST) helps them classify the tumor’s response. It shows if the tumor is getting smaller, staying the same, or growing.
Biomarker and Imaging Result Interpretation
Biomarkers and imaging results are very important. Biomarkers are molecules in the body that show if there’s cancer or how well treatment is working. For example, carcinoembryonic antigen (CEA) levels are checked in some cancer patients. Imaging tests like PET scans show how active the tumor is, helping doctors see if treatment is effective.
Multidisciplinary Team Input in Decision-Making
Deciding to stop chemotherapy is a team effort. Oncologists work with surgeons, radiologists, and pathologists. They look at the patient’s overall health, how well the treatment is working, and any side effects. This team approach helps make better decisions about continuing or stopping chemotherapy.
Clinical Signs That Chemotherapy Is Not Working
Chemotherapy’s success is closely watched. Certain signs show if treatment isn’t working. Oncologists check these signs to plan the next steps in treatment.
Progressive Tumor Growth During Treatment
Progressive tumor growth during treatment is a big sign. It means the tumor keeps growing or gets bigger, even with chemotherapy. We use scans to check the tumor’s size and see how treatment is working.
If the tumor keeps growing, it might mean the cancer cells are not responding to the treatment. This is tough news for patients and their families. But it doesn’t mean treatment has failed completely. We talk about other options and make a new plan together.
Development of New Metastatic Sites
Development of new metastatic sites is another sign. Metastasis happens when cancer spreads to other parts of the body. If new metastases show up during treatment, it means the cancer is still spreading.
We find new metastases through tests like scans and biopsies. This helps us change the treatment plan. We look for therapies that can better control the cancer’s spread.
“The appearance of new metastases during chemotherapy is a clear indication that the treatment is not working as intended, necessitating a reevaluation of the therapeutic approach.”
An Oncologist
Worsening Cancer-Related Symptoms
Worsening cancer-related symptoms also show treatment might not be working. Symptoms like pain, fatigue, weight loss, or breathing problems can get worse if the cancer isn’t responding. We watch these symptoms closely and adjust the treatment plan.
Dealing with worsening symptoms needs a full approach. This includes palliative care to improve life quality. We work with a team to support patients physically and emotionally during this tough time.
- Progressive tumor growth indicates chemotherapy resistance.
- New metastatic sites suggest the cancer is spreading.
- Worsening symptoms affect the patient’s quality of life.
Seeing these signs helps us decide if we should keep, change, or stop chemotherapy. Our goal is to give the best care, balancing treatment success with the patient’s well-being.
The Conversation About Stopping Chemotherapy
Talking about stopping chemotherapy is very important. It’s not just about the medicine. It also affects the patient’s feelings and their family’s well-being.
Communicating Treatment Futility
Oncologists need to be kind and clear when talking about stopping chemotherapy. If the treatment isn’t working, they must explain it gently. They use different ways to show why treatment won’t help anymore.
Key elements of this conversation include:
- Explaining the reasons for stopping chemotherapy
- Discussing alternative care options
- Addressing patient concerns and questions
Managing Patient and Family Expectations
It’s important to manage what patients and their families hope for. They often have big hopes and fears. We try to make sure their hopes match what’s possible with treatment.
| Expectation | Reality Check |
| Continued tumor shrinkage | Discussing the likelihood based on current data |
| Survival beyond initial prognosis | Explaining the factors influencing survival |
| Quality of life improvements | Outlining palliative care options |
Shared Decision-Making Frameworks
Shared decision-making is a team effort. It involves doctors, patients, and families making choices together. This way, everyone’s opinions are heard.
Key components of shared decision-making include:
- Information exchange about treatment options
- Discussion of patient values and preferences
- Deliberation on the best course of action
Using shared decision-making helps make sure stopping chemotherapy is a thoughtful choice. It focuses on what’s best for the patient.
Alternative Treatment Options After Stopping Chemotherapy
Stopping chemotherapy doesn’t mean the end of treatment. There are other paths to consider. For patients who have tried traditional chemotherapy, looking into alternative cancer treatments is key.
Transitioning to Targeted Therapies or Immunotherapies
Targeted therapies and immunotherapies are big steps forward in cancer treatment. Unlike traditional chemotherapy, they aim at cancer cells specifically. This reduces harm to healthy cells.
Immunotherapies use the body’s immune system to fight cancer. This is different from traditional treatments. For example, monoclonal antibodies and checkpoint inhibitors are promising in treating many cancers.
Accessing Clinical Trials for Refractory Disease
For those with refractory disease, clinical trials offer new treatments. These trials are key for cancer research. They give patients access to the latest therapies.
- Clinical trials offer new options for those who haven’t responded to standard treatments.
- Being in clinical trials helps cancer research and treatment development.
- It’s important for patients to talk about the benefits and risks with their doctor.
Integrative Medicine Approaches
Integrative medicine combines traditional treatments with complementary therapies. It treats the whole person, not just the disease. This can help manage symptoms and improve quality of life.
Examples include:
- Acupuncture for pain and symptom management
- Mindfulness and meditation for stress reduction
- Nutritional counseling to support overall health
By using these alternative treatments, patients can continue their cancer journey. They get a comprehensive and multifaceted approach to care.
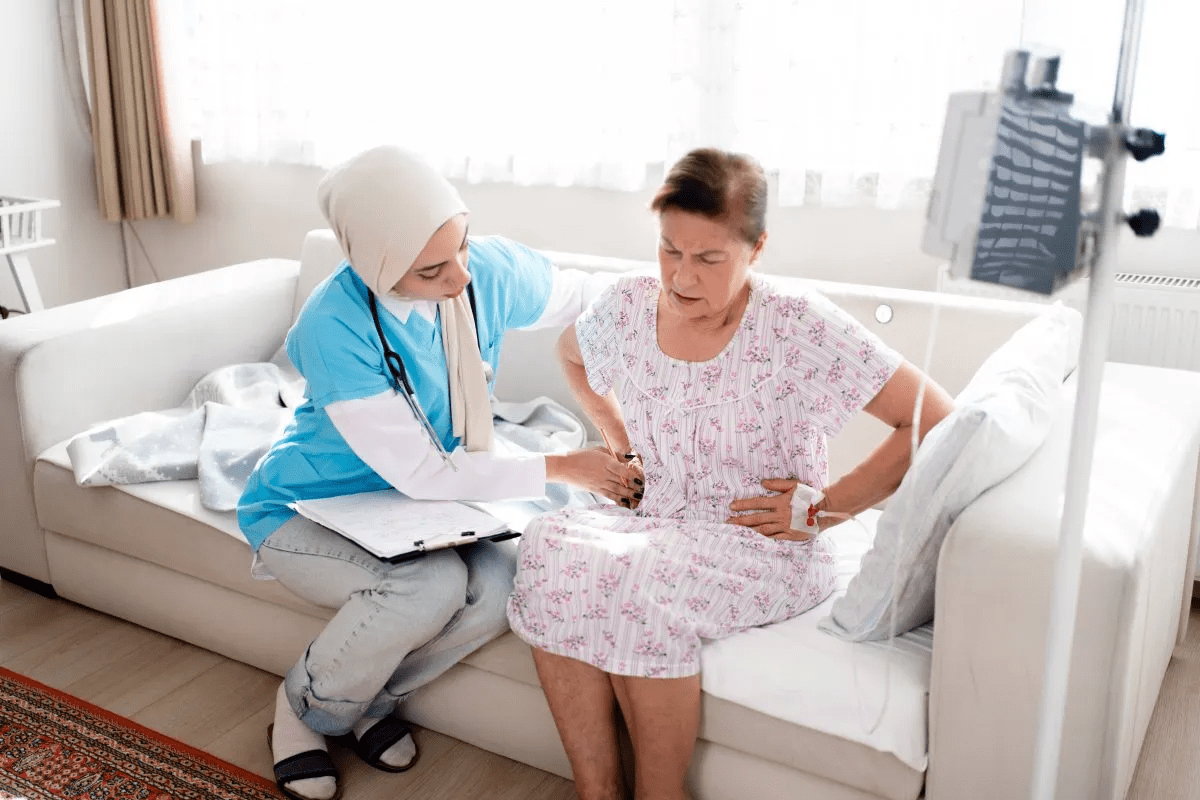
Transitioning to Palliative Care
Switching from curative chemotherapy to palliative care is a big step. It focuses on managing symptoms and improving comfort. This change is not about giving up but about focusing on quality of life.
The Misconception That Palliative Care Means Giving Up
Many think palliative care means giving up on treatment or hope. But, palliative care is actually about providing comprehensive support. It aims to ease symptoms, manage pain, and help with emotional and psychological issues.
The term “palliative” can be confusing. It’s key to know that palliative care is not the end of cancer treatment. It’s a new approach that focuses on the patient’s overall well-being.
Symptom Management Without Cytotoxic Therapy
After stopping chemotherapy, patients face many symptoms. Palliative care teams create personalized symptom management plans. These plans include medications, therapies, and more to ease discomfort and improve life quality.
These plans are made just for each patient. They address physical, emotional, and psychological needs. This way, we can greatly improve the patient’s remaining time.
Maintaining Dignity and Comfort
Palliative care is all about keeping patients’ dignity and comfort. It involves managing symptoms well and offering emotional and spiritual support to patients and their families.
By focusing on patient-centered care, we help people get the support they need during tough times. Our aim is to ensure a high quality of life, even when curative treatments are not possible.
Emotional Impact of Ending Cancer Treatment
Ending cancer treatment is a big step for patients, filled with mixed feelings. It’s important to understand the emotional effects on patients and their caregivers. This journey can be tough.
Processing Feelings of Loss and Uncertainty
Stopping chemotherapy can make patients feel lost and unsure. They might miss the routine of treatment and worry about the future. Healing isn’t just about the body; it’s also about the mind.
Patients often feel a mix of relief and fear about what’s next. It’s okay to feel overwhelmed. Recognizing these feelings is the first step to healing.
Coping Strategies for Patients and Caregivers
Finding ways to cope is key for patients and caregivers after treatment ends. Here are some strategies:
- Seeking support from family and friends
- Engaging in stress-reducing activities like meditation or yoga
- Joining support groups to connect with others
- Exploring hobbies that bring joy
Using these strategies can help manage emotions and look forward to a better future.
Professional Mental Health Support Resources
Professional help is crucial for healing. We suggest looking into counseling and therapy to meet emotional needs.
| Support Resource | Description | Benefits |
| Individual Counseling | One-on-one therapy sessions | Personalized support, emotional processing |
| Support Groups | Group therapy sessions | Community connection, shared experiences |
| Mindfulness Programs | Meditation and yoga classes | Stress reduction, relaxation techniques |
Using these resources can help patients and caregivers deal with the emotional challenges of ending treatment.
The Physical Recovery Process After Stopping Chemotherapy
Stopping chemotherapy starts a new journey: recovering and rebuilding your body. This time is key as your body heals from treatment. The recovery time varies, based on the chemotherapy type, your health, and any other health issues.
Understanding what to expect and how to recover well is crucial. Side effects can go away quickly or take longer.
Timeline for Side Effect Resolution
How long side effects last varies for everyone. Quick effects like nausea and tiredness often get better in a few weeks. But, effects like nerve damage or brain fog might take longer or could last forever.
“The end of chemotherapy is a big milestone, but it’s just the beginning of your recovery,” says an oncologist. “Knowing when side effects will go away helps patients and their families plan and cope.”
Managing Persistent Treatment Effects
Some people may still feel effects from chemotherapy, like constant tiredness, nerve issues, or brain fog. Handling these effects needs a mix of treatments, including medicine, physical therapy, and lifestyle changes.
- For nerve issues, treatments might include pain-relieving medicines.
- Cognitive rehab can help with memory and focus problems.
- Starting with gentle exercises and gradually getting more intense can help regain strength and mobility.
Rebuilding Physical Strength and Function
Getting stronger after chemotherapy takes time and a careful plan. Start with easy exercises and slowly add more as you get better and your doctor says it’s okay.
Nutrition is key in this recovery time. Eating a balanced diet with proteins, vitamins, and minerals helps your body heal. Drinking plenty of water is also important.
Listen to your body and don’t overdo it. Recovery is not a race; it’s about getting your health back at your own pace.
Post-Treatment Surveillance and Monitoring
Stopping cancer therapy doesn’t mean the end of treatment. It’s a time to watch closely. After chemotherapy, patients start a key phase of watching for cancer signs and managing side effects.
After chemotherapy, patients feel relief but also worry. They might see their doctors less often. But, they still need careful watching. Good post-treatment care includes regular tests, learning to spot cancer signs, and planning for long-term care.
Follow-up Testing Protocols
Follow-up tests are key in post-treatment care. The tests and how often they’re done depend on the cancer type, treatment, and health. Common tests include:
- Imaging tests like CT scans or MRI
- Blood tests for tumor markers
- Physical exams to check health and find any problems
For example, a breast cancer patient might need regular mammograms and MRI scans. The oncologist decides the test schedule based on guidelines and the patient’s situation.
| Test Type | Frequency | Purpose |
| Mammogram | Annually | Detect breast cancer recurrence |
| CT Scan | Every 6-12 months | Monitor for metastasis or recurrence |
| Blood Tests | As recommended by oncologist | Check for tumor markers |
Recognizing Signs of Possible Recurrence
Patients are key in watching for signs of cancer coming back. They should notice any changes in their body and tell their doctor. Signs of recurrence include:
- New lumps or masses
- Unexplained pain
- Changes in bowel or bladder habits
- Unintended weight loss
A renowned oncologist, says, “Teaching patients about their condition and signs of recurrence is vital. It helps catch problems early and improves care.”
“The key to successful post-treatment surveillance is a collaborative approach between healthcare providers and patients, ensuring that any signs of recurrence are caught early and addressed promptly.”
An Oncologist
Long-term Survivorship Care Planning
Long-term care planning focuses on the physical, emotional, and social needs of survivors. It deals with treatment side effects, promotes healthy living, and offers mental support.
We help patients create a care plan that meets their needs. This includes watching for late treatment effects, improving quality of life, and coordinating care.
By focusing on detailed post-treatment care, we can improve survivors’ lives and their chances of long-term survival.
Legal and Ethical Aspects of Stopping Chemotherapy
Stopping chemotherapy treatment raises legal and ethical questions. Healthcare providers must carefully consider these issues. They aim to prioritize patient care and respect individual rights.
Patient Rights and Informed Consent
One key principle is the patient’s right to informed consent. Patients should know about their treatment options, including the risks and benefits of stopping chemotherapy. This involves talking openly with the patient, their family, and the healthcare team.
Informed consent is an ongoing process. It’s important to document these discussions and the patient’s decisions.
“Ethical and legal standards in healthcare emphasize that patients have the right to refuse treatment, and this right should be respected by healthcare providers.”
Advance Care Planning Importance
Advance care planning is crucial for patients nearing the end of life. It involves talking about their wishes for care if they can’t make decisions themselves. This planning ensures their preferences are respected and helps family members avoid making tough decisions.
- Discussing patient wishes and values
- Completing advance directives
- Naming a healthcare proxy
Advance care planning gives patients control over their care, even when they can’t communicate their wishes.
Medical Futility Considerations
Medical futility refers to treatments that won’t help the patient. In chemotherapy, it’s when treatment is no longer effective or causes harm. Healthcare providers must assess the patient’s condition and discuss the futility of treatment with the patient and their family.
| Criteria | Description |
| Clinical Assessment | Evaluation of the patient’s current health status and response to treatment |
| Treatment Goals | Review of the original treatment objectives and whether they are still achievable |
| Quality of Life | Consideration of the impact of continued treatment on the patient’s quality of life |
Decisions on medical futility are complex. They require a team effort, including oncologists, palliative care specialists, ethicists, and other healthcare professionals.
Understanding the legal and ethical sides of stopping chemotherapy helps us support patients and their families. We can ensure care is tailored to their needs and respects their autonomy.
Conclusion: Finding Peace with the End of Treatment
Stopping chemotherapy is a big decision. It requires thinking about many things, like the benefits of palliative care. Doctors look at how well the tumor is responding and the patient’s health.
When it’s time to stop chemo, it’s important to do it safely. Moving to other care options is key. Palliative care helps manage symptoms and improves life quality.
We want patients to find peace and make the best of their situation after stopping chemo. Knowing how to quit safely helps them make good choices. This way, they can focus on their well-being.
FAQ
References
- Alexa, T., et al. (2014). Incidence of chemotherapy discontinuation and associated clinical characteristics in advanced non-small cell lung cancer. PMC. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4248059/
- Palmieri, L. J., Dubreuil, O., Bachet, J. B., et al. (2021). Reasons for chemotherapy discontinuation and end-of-life in patients with gastrointestinal cancer: a multicenter prospective AGEO study. ScienceDirect. https://www.sciencedirect.com/science/article/pii/S2210740120301066
What are the main reasons oncologists stop chemotherapy?
Oncologists stop chemotherapy for many reasons. These include finishing a planned treatment, achieving cancer remission, or when the disease gets worse. Side effects that are too hard to handle and patient choices also play a role.
How do oncologists determine if chemotherapy is working?
Oncologists check if chemotherapy is working in several ways. They look at how tumors change, use biomarkers and imaging, and get input from a team. They look for signs like tumors shrinking or staying the same size.
What are the clinical signs that chemotherapy is not working?
Signs that chemotherapy isn’t working include tumors growing, new metastatic sites, and worsening symptoms. These signs mean the treatment isn’t effective, and other options should be considered.
How do oncologists communicate the decision to stop chemotherapy?
Oncologists explain why they stop chemotherapy clearly. They manage expectations and involve patients in decisions. They aim to be compassionate and supportive.
What alternative treatment options are available after stopping chemotherapy?
After stopping chemotherapy, patients have other options. These include targeted therapies, immunotherapies, clinical trials, and integrative medicine. These choices depend on what each patient needs.
What is palliative care, and how does it differ from chemotherapy?
Palliative care focuses on managing symptoms and improving quality of life. It’s not just for the end of life. It can be given with or after chemotherapy.
How can patients cope with the emotional impact of ending cancer treatment?
Patients can deal with ending treatment by facing their feelings and using coping strategies. Getting support from loved ones, groups, and mental health professionals helps.
What is the physical recovery process like after stopping chemotherapy?
Recovering from chemotherapy involves getting rid of side effects and rebuilding strength. The time it takes varies. Healthcare providers offer guidance for a safe recovery.
Why is post-treatment surveillance and monitoring important?
Monitoring after treatment is key for catching recurrence and managing side effects. It involves regular tests and planning for long-term care. This ensures ongoing support.
What legal and ethical considerations are involved in stopping chemotherapy?
Stopping chemotherapy raises legal and ethical questions. These include patient rights, informed consent, and advance care planning. These ensure patients get respectful care.
How can patients make informed decisions about stopping chemotherapy?
Patients can make informed choices by understanding their options. They should discuss their goals and values with their team. Considering treatment effectiveness and quality of life is important.
What happens after chemotherapy is stopped?
After stopping chemotherapy, patients may try other treatments or receive palliative care. They may also enter a monitoring phase. The focus is on managing symptoms and improving quality of life.
Can patients restart chemotherapy if needed?
Sometimes, patients can start chemotherapy again if their disease comes back. This decision depends on their health, previous responses, and current disease status.