Last Updated on October 20, 2025 by Bilal Hasdemir

Choosing a bone marrow transplant for Acute Myeloid Leukemia (AML) is a big decision. It can greatly improve survival rates and give you hope again. At Liv Hospital, we help you understand what to expect from AML bone marrow transplant survival in 2025. We focus on patient care and clinical excellence.
Recent studies show that the 5-year survival rate after bone marrow transplant for AML is between 40% and 65%. This depends on your age and the type of transplant. We will talk about the current survival rates and what affects them. This will give you a clear idea of what to expect.
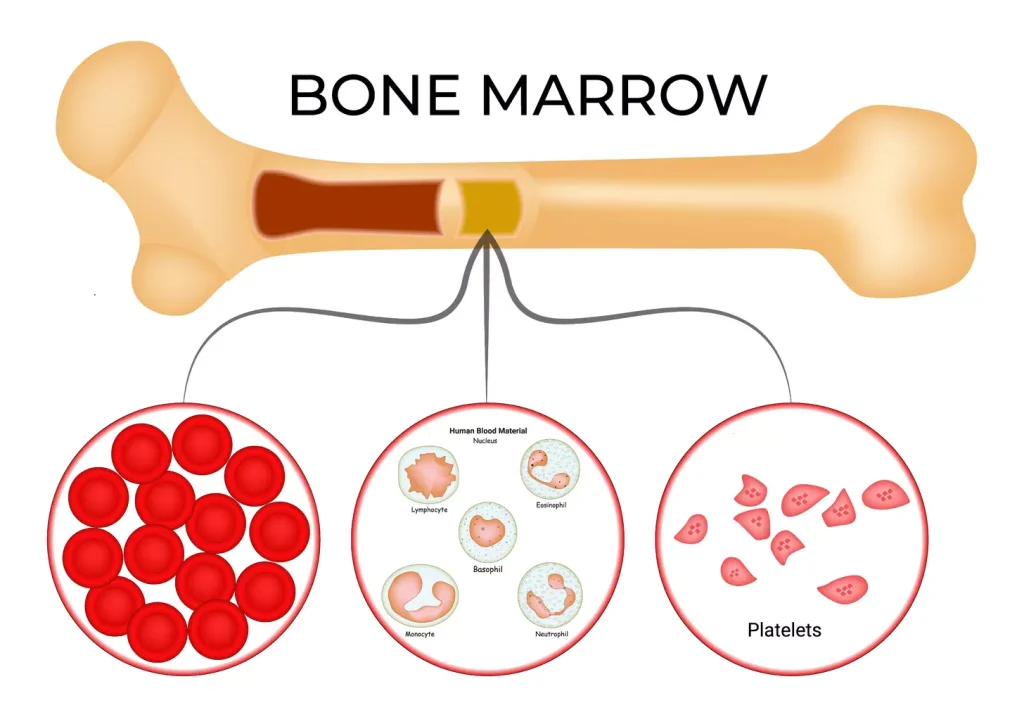
Acute Myeloid Leukemia (AML) is a serious blood cancer that affects the bone marrow. It needs a detailed treatment plan. We will look into AML and how bone marrow transplantation is key in treating it.
AML is marked by fast-growing abnormal cells in the bone marrow. These cells block the production of healthy blood cells. This can cause severe anemia, infections, and bleeding.
Bone marrow transplantation is a major treatment for AML. It replaces damaged bone marrow with healthy stem cells. This can cure AML by removing the diseased marrow and starting normal blood cell production again.
There are two main types of bone marrow transplants for AML: allogeneic and autologous. Allogeneic transplants use donor stem cells. Autologous transplants use the patient’s own stem cells. The choice depends on the patient’s health and disease stage.

Medical research has led to better AML survival rates after bone marrow transplants. Studies show a big jump in survival rates over the last 20 years. This gives hope to those with this tough disease.
The 5-year survival rate for AML patients after bone marrow transplant has greatly improved. Now, about 45-50% of patients who get allogeneic transplants survive for five years.
From 2020 to 2025, survival rates have kept going up. This is thanks to better transplant methods, choosing the right patients, and better care after transplant.
Comparing survival rates, bone marrow transplant clearly helps AML patients live longer. This is true, even for those with high-risk disease.
| Treatment Approach | 5-Year Survival Rate |
|---|---|
| Allogeneic Bone Marrow Transplant | 45-50% |
| Autologous Bone Marrow Transplant | 40-45% |
| Chemotherapy Alone | 20-30% |
These numbers show how key bone marrow transplant is in treating AML. It can greatly improve patient results.
Survival rates after BMT for AML change with age. The patient’s age at transplant is key to success.
Pediatric patients, under 18, often see high survival rates. Some studies show up to 70% survive after transplant. A study in Nature found younger patients do better. This is because they have fewer health issues and a stronger immune system.
Young adults, 18-49, also have good survival chances. Their rates are a bit lower than kids’. Their health and fewer health problems help them do well with the transplant.
Older adults, 50-55 and up, face lower survival rates. This is because they often have more health issues and are less strong. Choosing the right patient and using gentle treatments is very important for them.
Geriatric patients need extra care. Doctors do detailed checks to see if they can handle BMT. They use gentler treatments to reduce harm.
| Age Group | Survival Rate |
|---|---|
| Pediatric | Up to 70% |
| Young Adults | 50-60% |
| Older Adults | 30-40% |
Age really matters for BMT success in AML patients. Knowing this helps doctors make better treatment plans.
Allogeneic and autologous BMT are two ways to treat AML. Each has its own success rates and things to consider. Knowing these differences helps patients and doctors make better treatment choices.
Research shows allogeneic BMT works for about 62% of patients. Autologous BMT works for about 65%. These numbers are based on recent studies and show the general success of AML treatments.
| Transplant Type | Success Rate |
|---|---|
| Allogeneic BMT | 62% |
| Autologous BMT | 65% |
Choosing between allogeneic and autologous BMT depends on several things. These include the patient’s health, the AML’s characteristics, and if a donor is available. Allogeneic BMT is often chosen when there’s a high risk of relapse or if the bone marrow is badly damaged.
A study says the choice between allogeneic and autologous BMT should be based on the patient’s risk factors and disease characteristics. This shows how important it is to tailor treatment to each patient’s needs in AML care.
For allogeneic BMT, the match between donor and recipient is key. Transplants from matched donors usually have better results because they have lower risks of GVHD. Unmatched donor transplants are riskier, but new treatments have made them safer.
Understanding allogeneic and autologous BMT helps patients and doctors make better choices. This can lead to better survival rates and quality of life for AML patients.
In the last twenty years, bone marrow transplant survival rates have greatly improved. This is thanks to new medical technology and better transplant techniques. These changes have led to better results for patients with acute myeloid leukemia (AML).
The last twenty years have seen a big change in bone marrow transplant (BMT) results. Studies show that survival rates have gone up. This is because of better transplant methods, choosing the right patients, and better care after the transplant.
New technology, like better donor matching and advanced immunosuppressive treatments, has helped a lot. Also, managing graft-versus-host disease (GVHD) better has led to better patient results.
Reduced-intensity conditioning (RIC) has made BMT available to more people. This includes older patients and those with other health issues. RIC has led to lower death rates from treatment and better survival chances for some patients.
| Time Period | Survival Rate Improvement | Key Advancements |
|---|---|---|
| 2000-2005 | 15% increase | Better donor matching |
| 2006-2010 | 20% increase | Immunosuppressive regimens |
| 2011-2015 | 25% increase | Reduced-intensity conditioning |
| 2016-2020 | 30% increase | GVHD management |
These changes have all helped improve bone marrow transplant survival rates. They give hope to patients with AML and other blood cancers.
The timing of a bone marrow transplant is key for AML patients. We’ll look at how disease status and transplant timing affect survival rates. This is important for AML patients getting BMT.
Patients transplanted in their first complete remission do better. Studies show a higher survival rate for bone marrow transplant leukemia patients when transplanted early.
Patients with refractory or relapsed AML face tougher challenges. The leukemia relapse after bone marrow transplant survival rate is a big concern. Relapse is a major hurdle in AML management.
Finding the best time for BMT is essential. It’s a balance between avoiding disease progression and transplant risks. The aml stem cell transplant prognosis is better with timely transplantation.
Minimal residual disease (MRD) before and after BMT is a big factor. Patients with MRD positivity might need extra treatments or closer watch. This can help improve survival chances.
In summary, disease status and BMT timing are vital for AML patients’ survival. Knowing these factors helps make better decisions about BMT timing and management.
The journey doesn’t end after a bone marrow transplant. AML patients face many post-transplant complications. These can affect their survival. It’s key to understand these complications for better patient care.
Graft-Versus-Host Disease (GVHD) is a big problem after allogeneic bone marrow transplantation. It happens when the donor’s immune cells attack the recipient’s body. GVHD can be acute or chronic, with chronic GVHD hitting survival harder.
Studies show managing GVHD is key to better bone marrow transplant survival rates in leukemia patients.
Infections are a big worry after a transplant because the immune system is weak. Bacterial, viral, and fungal infections can be deadly. They need close watching and prevention.
The risk of infection is highest in the first few months after transplant. This directly affects the AML BMT success rate.
Organ toxicity is a risk from the conditioning regimen before transplant. It can cause long-term issues like heart problems, lung issues, and secondary cancers. Managing these toxicities is key to better bone marrow transplant prognosis and survival.
In conclusion, complications like GVHD, infections, and organ toxicity are critical for AML patient survival. Effective management of these is vital for better leukemia relapse after bone marrow transplant survival rates and patient outcomes.
The journey doesn’t end with a bone marrow transplant. AML patients face the risk of relapse and its impact on survival. Relapse after bone marrow transplantation (BMT) is a big challenge. It affects the survival rate of patients with Acute Myeloid Leukemia (AML).
Studies show that relapse rates after BMT vary. Factors like the patient’s disease status, transplant type, and graft-versus-host disease (GVHD) play a role. For example, patients with AML in first complete remission have lower relapse rates. Those transplanted in later remissions or with active disease face higher risks.
Survival rates after relapse are generally low. They can vary based on several factors, like when the relapse happens and the patient’s health. Recent data suggest that the leukemia relapse after bone marrow transplant survival rate can improve with timely and effective treatments.
Options for relapse after BMT include chemotherapy, targeted therapy, and sometimes a second transplant. The choice depends on the patient’s past treatments, health, and relapse characteristics. For more on cancers needing stem cell transplant, visit this resource.
Several factors predict relapse risk after BMT. These include minimal residual disease (MRD) before and after transplant, donor type, and conditioning regimen. Identifying these early can help tailor care and potentially improve outcomes for AML patients.
In conclusion, while relapse after BMT is a big challenge, understanding its implications and treatment options can improve survival rates for AML patients. We keep up with advancements in AML stem cell transplant survival rate and bone marrow transplant survival rate leukemia to offer the best care.
For AML patients, knowing what to expect long-term after BMT is key. Thanks to better technology and treatments, their future looks brighter.
Recent studies show a big win in AML treatment: a 10-year survival rate of up to 76% for BMT patients. This proves BMT is a strong option for AML treatment.
Long-term BMT survivors often live well, doing things they did before the transplant. Yet, some may face late effects like chronic GVHD.
Handling late complications is key for BMT survivors’ long-term care. We watch for organ damage and fix issues quickly for the best results.
Long-term survivors face risks of new cancers. Regular check-ups are vital to catch new cancers early and treat them fast.
We’re working hard to make BMT better for AML patients. With new research and treatments, their future is looking up.
New treatments are changing how we fight Acute Myeloid Leukemia (AML), focusing on bone marrow transplants. Studies show big improvements in AML transplant success thanks to these new methods.
CAR-T cell therapy is a new hope for AML patients getting bone marrow transplants. It uses special T cells to fight cancer. Recent studies suggest it could lower relapse rates and boost survival chances.
New ways to prepare for bone marrow transplants are being tested. These aim to cut down on side effects while keeping the treatment effective. Scientists are working hard to make these regimens better, hoping for better survival rates and fewer complications.
Keeping AML patients in remission after transplant is key. New treatments, like targeted drugs and immunotherapies, are being looked at. They might help keep the cancer away for longer, improving transplant success.
Immunotherapies, like checkpoint inhibitors and bispecific antibodies, are being studied. They aim to boost the immune system’s fight against cancer. This could lead to fewer relapses and better survival rates for AML patients.
| Therapy | Potential Benefits | Ongoing Research |
|---|---|---|
| CAR-T Cell Therapy | Reduced relapse rates, improved overall survival | FDA priority review for CAR-T cell therapy |
| Novel Conditioning Regimens | Reduced toxicity, improved graft-versus-leukemia effect | Ongoing research to optimize conditioning protocols |
| Post-Transplant Maintenance Strategies | Prevention of relapse, improved long-term survival | Investigations into targeted agents and immunotherapies |
| Immunotherapy Approaches | Enhanced immune response against leukemic cells | Exploration of checkpoint inhibitors and bispecific antibodies |
These new treatments offer hope for better outcomes in AML bone marrow transplants. As research keeps advancing, we can look forward to even better survival rates and quality of life for AML patients.
The treatment of acute myeloid leukemia (AML) is changing, with bone marrow transplants playing a big role. The outlook for AML bone marrow transplant survival looks good. This is thanks to new treatments and better technology and procedures.
Research shows that the acute myeloid leukemia survival rate bone marrow transplant is getting better. Recent studies point to a big increase in success rates. The bone marrow transplant for AML success rate has also gone up. This is because of better allogeneic and autologous transplant methods.
AML treatment is changing, with the AML bone marrow transplant success rate improving. This is thanks to new conditioning regimens and post-transplant care. Also, adding immunotherapy is expected to make bone marrow transplant survival rate leukemia outcomes even better.
We need to keep watching and reporting on AML treatment progress. This ensures patients get the best care. With ongoing research, we’re hopeful about the future of AML bone marrow transplant survival.
The 5-year survival rate for AML patients after bone marrow transplant varies. It depends on age, disease status, and transplant type. Recent data shows it can be between 40% and 70%.
Age is a big factor in survival after BMT for AML. Kids and young adults do better than older adults. Young adults (18-49) have better chances than those over 50.
Allogeneic BMT has a success rate of about 62%. Autologous BMT is around 65%. The choice depends on disease status and donor availability.
Survival rates have improved a lot in the last 20 years. Advances in technology and procedures have helped. So has the use of reduced-intensity conditioning.
Disease status at transplant time matters a lot. Those in first complete remission do better. Those in later stages or with relapsed disease have lower chances.
Complications like graft-versus-host disease and infections can lower survival rates. Managing these is key to better outcomes.
Relapse can greatly lower survival chances. The risk of relapse varies. Survival after relapse depends on several factors, including when it happens and treatment options.
Long-term survival for AML patients after BMT has improved. Some studies show a 10-year survival rate of about 76%. Long-term survivors may face late complications, which need careful management.
New therapies like CAR-T cell therapy and immunotherapy are being explored. They aim to improve transplant outcomes and survival rates for AML patients.
MRD status is key in deciding when to transplant and survival chances. Those without MRD do better than those with it.
The donor type, matched or unmatched, impacts outcomes. Matched donor transplants usually have better results than unmatched ones.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us