Last Updated on November 27, 2025 by Bilal Hasdemir

Radiation therapy is a key treatment for cancer. It damages cancer cells’ DNA, killing them or slowing their growth. At Liv Hospital, we know how vital this treatment is and the worries it raises.
Many patients often ask, “Can you have radiation treatment more than once? The answer depends on several factors such as past treatments, the location of the tumor, and the patient’s overall health. In some cases, radiation can be safely repeated, but doctors must carefully evaluate the potential risks to nearby healthy tissues.
The number of times radiation therapy can be given varies. It depends on where the tumor is, the total dose already received, and the body’s ability to tolerate more radiation. Understanding these factors helps explain why there are limits to this treatment and why careful planning is key for your health.
Knowing the limits of radiation therapy ” and when it can be safely repeated ” is important for planning effective treatment. Our team at Liv Hospital aims to offer top-notch healthcare while supporting and guiding international patients with care and compassion.
Key Takeaways
- The number of times radiation therapy can be administered depends on individual factors.
- Previous exposure, tumor location, and overall health are key considerations.
- Careful planning is essential to protect long-term health.
- Limits to radiation therapy are in place to minimize risks.
- Effective treatment planning is vital for cancer patients.
Understanding Radiation Therapy Basics

Radiation therapy is a treatment that uses high-energy particles or waves to kill cancer cells. It’s a key part of cancer care, with different types and uses.
What Is Radiation Therapy and How Does It Work
Radiation therapy damages cancer cells’ DNA, stopping them from growing. This damage comes from high-energy radiation. It can be given from outside the body or placed inside with radioactive material.
External beam radiation therapy (EBRT) is common. It uses a machine outside the body to target tumors. This method is precise, protecting healthy tissues nearby.
Types of Radiation Treatments Available
There are two main types: external beam radiation therapy and brachytherapy. External beam therapy includes 3D conformal, intensity-modulated, and stereotactic body radiation therapy.
Brachytherapy places radioactive material close to the tumor. It delivers a high dose of radiation directly to cancer cells, reducing harm to healthy tissue.
Common Cancer Types Treated with Radiation
Radiation therapy helps treat many cancers, like breast cancer, prostate cancer, lung cancer, and brain tumors. The choice to use radiation depends on the cancer type, stage, and the patient’s health.
It can be used alone or with surgery and chemotherapy. Its effectiveness makes it a key part of cancer treatment plans globally.
Can You Have Radiation Treatment More Than Once?

Whether you can have radiation treatment more than once depends on several factors. These include how much radiation you’ve had before and your overall health. Deciding on more radiation therapy is complex and requires careful thought.
Factors That Determine Eligibility for Repeated Treatment
Many factors decide if you can have radiation treatment again. These include the location and type of the tumor, your overall health, and the previous radiation dose. We look at each case closely, considering these points to see if more radiation is possible.
The location of the tumor matters a lot. Some parts of the body are more sensitive to radiation. If the tumor is in an area already treated with radiation, we must weigh the risks and benefits of more treatment.
Previous Exposure and Cumulative Dose Considerations
How much radiation you’ve had before and the total dose are key when deciding on more treatment. We look at the total dose of radiation you’ve had to assess the risks of more exposure.
The total radiation dose affects the risk of side effects and damage to healthy tissues. We use advanced systems to figure out the total dose and plan the safest treatment.
Time Intervals Between Radiation Courses
The time between radiation treatments is also important. Giving healthy tissues time to recover from radiation is essential. The recovery period depends on the individual and the treatment.
We plan the timing of radiation treatment carefully. We consider the type of cancer, the dose of radiation needed, and your overall health.
Safety Protocols and Maximum Dose Limits
Keeping patients safe during radiation therapy is key. It involves strict safety rules and dose limits. Radiation therapy is a vital part of cancer treatment. It works best when it precisely targets tumors while protecting healthy tissues.
Understanding Maximum Radiation Dose for Cancer
The highest dose a patient can get depends on many things. These include the cancer type, its stage, where it is, and the patient’s health. Maximum doses are set to avoid harming healthy tissues and reduce long-term side effects. Treatments are split into smaller doses to help healthy tissues heal between sessions.
A study on PubMed Central shows how splitting doses can lower toxicity. This knowledge helps doctors tailor treatments to each patient. It aims to be as effective as possible while keeping risks low.
Cumulative Radiation Exposure Concerns
Worry about total radiation exposure is big in radiation therapy. It can increase the chance of side effects and long-term damage. It’s important to plan and watch closely to keep doses safe.
| Tissue Type | Radiation Tolerance | Cumulative Dose Limit |
| Bone Marrow | Low | 20 Gy |
| Liver | Moderate | 30 Gy |
| Lung | Low to Moderate | 20-30 Gy |
How Radiation Affects Healthy Tissue
Radiation therapy can harm healthy tissues, causing side effects. The damage’s severity depends on the dose, treatment length, and tissue type. Knowing how radiation affects healthy tissue is vital for safety. By reducing healthy tissue exposure, doctors can lower complication risks and better patient outcomes.
Radiation Tolerance of Different Body Tissues
It’s important to know how body tissues react to radiation for cancer treatment. The body responds differently to radiation therapy in various tissues and organs.
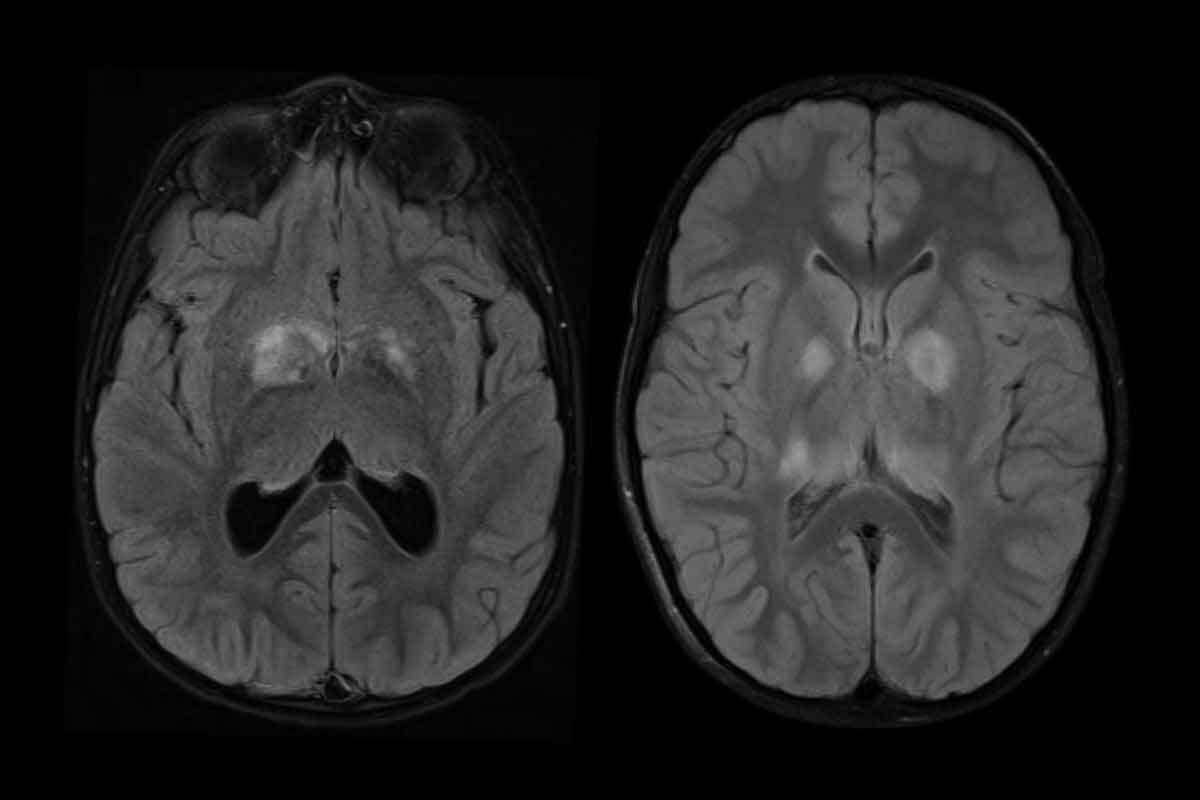
High-Sensitivity vs. Low-Sensitivity Organs
Body organs and tissues vary in their sensitivity to radiation. High-sensitivity organs like the brain, spinal cord, and reproductive organs are more at risk. On the other hand, low-sensitivity organs like the liver, kidneys, and lungs can handle more radiation but are not completely safe.
Knowing the difference between these organs is key when planning radiation therapy. We aim to kill cancer cells while protecting sensitive tissues.
Recovery Periods for Various Tissue Types
Recovery times after radiation vary among tissues. Acute responding tissues like the skin and mucous membranes recover quickly, often in weeks. But late responding tissues like the spinal cord and brain may take months or years to heal, and sometimes the damage is permanent.
Knowing these recovery times helps us decide when and if to repeat radiation treatments.
Why Certain Areas Cannot Receive Radiation Twice
Some body areas can’t handle radiation twice because of the risk of severe damage. For example, the spinal cord can only take so much radiation before it’s at risk for serious problems like myelopathy. The brain and eyes are also very sensitive to radiation, and getting hit twice can cause lasting harm.
We weigh the risks and benefits of radiation therapy for each patient. We consider the specific tissues and organs involved.
Advanced Techniques Enabling Re-Treatment Options
Advanced radiation techniques have changed cancer treatment a lot. They offer new chances for re-treatment in some patients. These new technologies make radiation therapy more precise and safe. This means treatments can be more effective and less harmful to healthy tissues.
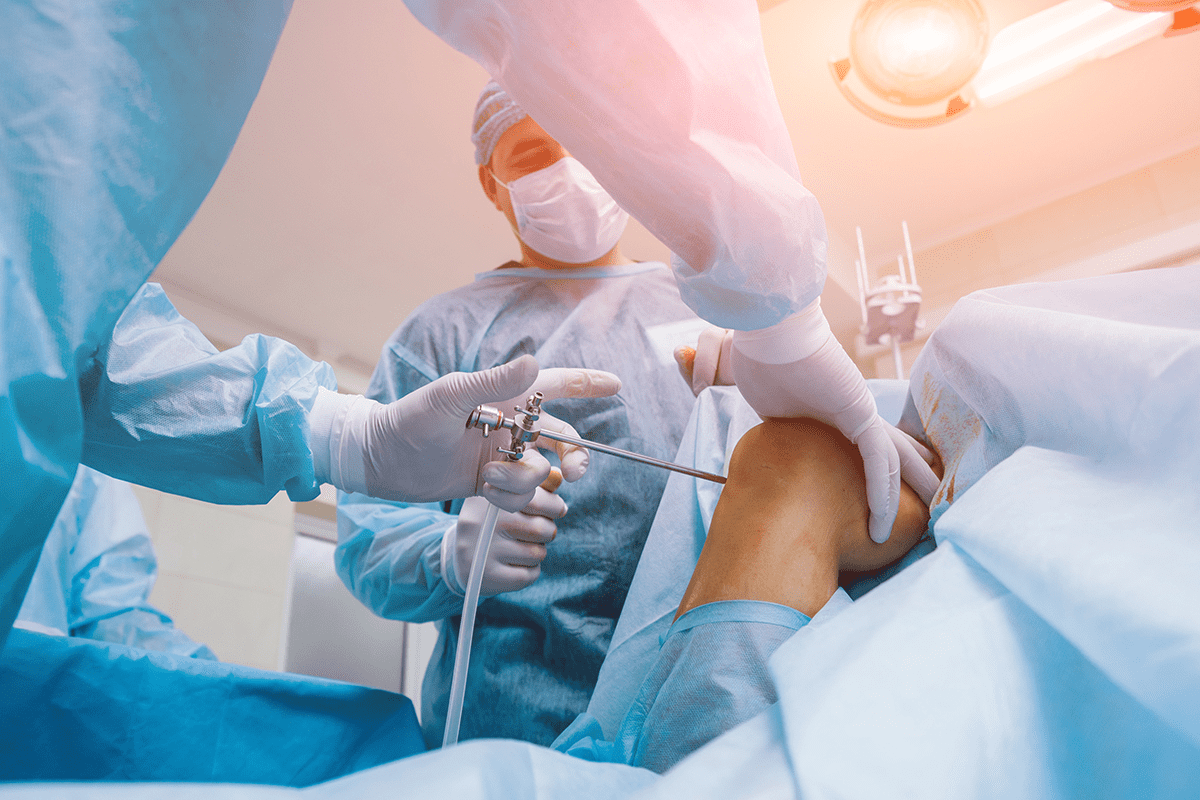
Stereotactic Body Radiotherapy (SBRT) for Repeat Treatments
Stereotactic Body Radiotherapy (SBRT) is a precise radiation therapy. It gives high doses of radiation to small tumors in a few sessions. SBRT is great for treating tumors that come back or spread to places like the spine, liver, or lungs.
Intensity-Modulated Radiation Therapy (IMRT)
Intensity-Modulated Radiation Therapy (IMRT) changes the intensity of the radiation beam. This lets doctors give a precise dose to the tumor, while protecting nearby healthy tissues. IMRT is good for tumors with complex shapes or those near important structures.
Proton Therapy and Other Precision Approaches
Proton therapy uses protons to kill cancer cells. It’s great for tumors near important structures, like brain tumors or tumors in children. It’s very precise and causes less damage to healthy tissues.
Other methods like volumetric modulated arc therapy (VMAT) and image-guided radiation therapy (IGRT) also improve radiation treatment. They make treatments more accurate and effective.
| Technique | Description | Benefits |
| SBRT | Highly precise radiation therapy for small tumors | Effective for treating recurrent or metastatic tumors |
| IMRT | Modulates radiation beam intensity for conformal dose distribution | Spares surrounding normal tissues, ideal for complex-shaped tumors |
| Proton Therapy | Uses protons to kill cancer cells with high precision | Minimizes damage to surrounding healthy tissues, ideal for tumors near critical structures |
These advanced radiation techniques have opened up new possibilities for re-treatment. They offer hope to patients with cancer that comes back or doesn’t go away. These technologies improve treatment outcomes and quality of life for patients.
Typical Radiation Treatment Schedules
Knowing how often radiation therapy is given is key for both patients and doctors. It’s a common treatment for many cancers. The schedule can greatly affect how well the treatment works.
How Often Is Radiation Therapy Administered
Radiation therapy is usually given every day, from Monday to Friday. It goes on for weeks. But, how long and how often it’s given can change based on the cancer type and stage.
Standard treatment protocols are often used for many cancers. They involve giving radiation daily. This helps protect healthy tissues while targeting the tumor.
Standard Five-Day-a-Week Protocols
The usual schedule is treatment five days a week. This conventional fractionation helps control tumors while keeping normal tissues safe.
“The conventional fractionation schedule has been the cornerstone of radiation therapy, providing a balance between efficacy and toxicity.”
Hypofractionation and Accelerated Treatment
In some cases, hypofractionation or accelerated treatment is used. Hypofractionation means giving bigger doses less often. Accelerated treatment shortens the treatment time. Both can be good for certain tumors.
| Treatment Protocol | Description | Typical Use |
| Conventional Fractionation | Daily radiation, 5 days a week | Most cancer types |
| Hypofractionation | Larger doses, fewer fractions | Certain tumor types, palliative care |
| Accelerated Treatment | Compressed treatment schedule | Rapidly growing tumors |
How Many Rounds of Radiation Is Normal by Cancer Type
The number of radiation treatments changes a lot depending on the cancer. Early-stage cancers might need fewer treatments. More advanced cancers might need more.
- Early-stage cancers: Fewer fractions, potentially hypofractionated
- Locally advanced cancers: Standard fractionation, possibly with chemotherapy
- Palliative care: Hypofractionation, for symptom relief
Understanding the different radiation schedules helps patients and doctors make better choices in cancer care.
Combining Radiation with Chemotherapy
Using radiation and chemotherapy together is a strong way to fight cancer. It works well for many types of cancer. This method can be more effective than using just one treatment.
Can You Do Chemo and Radiation at the Same Time?
Yes, you can get chemotherapy and radiation at the same time. This is often used for cancers like head and neck, cervical, and some lung cancers. The choice to use both treatments together depends on the cancer type, stage, and the patient’s health.
Benefits of Concurrent Treatment: Using both treatments together can make treatment more effective. It can:
- Make cancer cells die faster
- Lower the chance of cancer coming back
- Help patients live longer with certain cancers
Benefits of Concurrent Treatment Approaches
Using chemotherapy and radiation together has many benefits. It can lead to better treatment results and longer survival. This method is good for patients with aggressive or advanced cancers.
| Treatment Approach | Benefits | Potential Side Effects |
| Chemotherapy Alone | Targets cancer cells throughout the body | Systemic side effects like hair loss, nausea |
| Radiation Therapy Alone | Precise targeting of tumor sites | Localized side effects like skin irritation |
| Concurrent Chemotherapy and Radiation | Enhanced cancer-killing effect, improved survival rates | Increased risk of side effects, potentially more severe |
Managing Side Effects from Combined Therapies
It’s important to manage side effects when using both treatments. Patients might feel tired, have skin reactions, or stomach problems. Doctors may suggest:
- Supportive care like nutrition advice and pain relief
- Changing the treatment plan, like reducing doses or taking breaks
- Watching closely for side effects
Knowing the good and bad of combining radiation and chemotherapy helps patients make better choices. It’s key to understanding treatment options and making informed decisions.
Managing Side Effects from Multiple Radiation Courses
Managing side effects is key when you have to go through multiple radiation courses for cancer treatment. Radiation therapy can lead to both immediate and long-term effects. These can really affect how well you live your life.
Acute vs. Late Radiation Effects
Radiation effects are split into acute and late types. Acute radiation effects happen right during or soon after treatment. Symptoms like tiredness, skin issues, and nausea are common. These usually go away once treatment ends.
Late radiation effects show up months or years later. They can include scarring, new cancers, and problems with organs. Knowing the difference between these effects is key to managing them well.
Supportive Care Strategies
Supportive care is very important in dealing with radiation therapy side effects. It includes things like pain control, nutrition help, and mental health support. Good supportive care can really help patients feel better and handle treatment better.
| Supportive Care Measure | Description | Benefit |
| Pain Management | Use of medications and other interventions to control pain | Improved comfort and reduced distress |
| Nutritional Support | Dietary counseling and supplements to maintain nutrition | Enhanced recovery and reduced risk of malnutrition |
| Psychological Counseling | Counseling and therapy to address emotional and psychological needs | Better coping mechanisms and reduced anxiety |
Monitoring Long-Term Health After Repeated Radiation
It’s very important to keep an eye on your health after going through many radiation treatments. Regular check-ups and tests help catch and manage late effects early. We stress the need for ongoing monitoring for the best care.
By knowing about radiation therapy side effects and using good supportive care, we can help patients get better care during multiple radiation treatments.
Conclusion: Advancements in Radiation Therapy and Future Directions
Looking at radiation therapy today, we see it’s getting better thanks to research and new tech. This treatment is now more precise, hitting tumors hard while keeping healthy tissues safe.
The future looks bright for radiation therapy. New methods like Stereotactic Body Radiotherapy (SBRT) and Intensity-Modulated Radiation Therapy (IMRT) are on the horizon. These will make treatments more tailored to each patient, using the latest tech for better results.
As radiation therapy keeps growing, new ideas will be key in its development. Focusing on better patient care and treatment success, the future of radiation therapy is set to change cancer treatment for the better.
FAQ
Can you have radiation therapy more than once?
Yes, you can have radiation therapy more than once. But, it depends on several factors. These include the total dose, how long it’s been between treatments, and how sensitive the tissues are.
Why can’t you have radiation twice in the same area?
Some body parts can’t handle radiation twice because of the risk to healthy tissues. The sensitivity of tissues to radiation varies. Areas like the spinal cord are very sensitive and might not handle a second treatment.
What is the maximum number of radiation treatments?
The number of radiation treatments varies. It depends on the cancer type, tumor location, and your health. There’s no one answer for everyone. The decision is made based on your specific situation.
Can you do chemo and radiation at the same time?
Yes, you can have chemotherapy and radiation therapy at the same time. This is often used for certain cancers. But, it depends on your cancer type, stage, and health.
How often is radiation therapy administered?
Radiation therapy is usually given five days a week. But, the schedule can change based on your cancer and treatment plan. Some plans might have more or less frequent treatments.
How many rounds of radiation is normal?
The number of radiation rounds varies by cancer type and stage. Some cancers follow a standard five-day-a-week plan. Others might have different schedules.
What are the benefits of combining radiation with chemotherapy?
Combining radiation and chemotherapy can be more effective. It targets cancer cells in different ways. This can help control the tumor better and lower the chance of it coming back.
How are side effects managed during radiation therapy?
Side effects from radiation therapy are managed with supportive care. This includes medication, lifestyle changes, and nutrition advice. It’s also important to watch your health long-term after treatment.
What is the maximum radiation dose for cancer treatment?
The maximum radiation dose varies by tumor type, location, and your health. The goal is to give enough radiation to control the tumor without harming healthy tissues.
References
- Solberg, T. D., et al. (2011). Quality and safety considerations in stereotactic radiosurgery and stereotactic body radiation therapy. Journal of Applied Clinical Medical Physics, 12(4), 3414. https://pmc.ncbi.nlm.nih.gov/articles/PMC3808746/