Brain tumor surgery is a complex procedure that needs precision and care. The main goal is to remove unhealthy cells in the brain while keeping the healthy tissue around it safe.
Liv Hospital uses advanced techniques for brain cancer surgery. These include microsurgical tools, endoscopic surgery, and laser ablation. These methods help remove the tumor precisely, reducing damage to the brain.
Removing the tumor is key for both malignant and non-malignant brain masses. This surgery can greatly improve a patient’s condition. It offers hope to those facing this tough diagnosis.
Key Takeaways
- Advanced surgical techniques are used for precise brain tumor removal.
- Liv Hospital prioritizes patient-centered care in brain cancer surgery.
- The goal is to remove the tumor while preserving healthy brain tissue.
- Surgical intervention is vital for both malignant and non-malignant tumors.
- Patients can see a big improvement after brain mass removal.
Understanding Brain Tumors and Their Classification

It’s key to know the different types of brain tumors to create good treatment plans. Brain tumors fall into two main groups: malignant and non-malignant.
Types of Brain Tumors: Malignant vs. Non-Malignant
Malignant brain tumors grow fast and spread to other brain areas. They are aggressive and can be deadly if not treated quickly. Non-malignant (benign) tumors grow slower and don’t spread, but they can cause problems because of where they are and how big they get.
Knowing if a tumor is malignant or non-malignant helps decide how to treat it. Malignant tumors need strong treatments like surgery, radiation, and chemotherapy. Benign tumors might just need surgery or watching, based on their type and how they affect the patient.
Common Locations and Growth Patterns
Brain tumors can happen in many places in the brain. Where they are and how they grow affects brain function. Some tumors grow slowly and stay benign, while others grow fast and can harm important brain areas.
| Tumor Type | Common Location | Growth Pattern |
| Meningioma | Near the surface of the brain, attached to the meninges | Typically slow-growing |
| Glioblastoma | Cerebral hemispheres | Rapidly growing and invasive |
| Pituitary Adenoma | Pituitary gland | Usually benign and slow-growing |
Impact on Neurological Function
The place and size of a brain tumor greatly affect brain function. Tumors can lead to symptoms like headaches, seizures, and problems with thinking and moving. This depends on which brain areas are affected.
It’s important to understand how a brain tumor might affect brain function for treatment planning. Early diagnosis and treatment can greatly help patients with brain tumors.
Diagnosis and Pre-Surgical Assessment

Diagnosing a brain tumor requires advanced imaging and neurological tests. This detailed approach helps understand the tumor’s nature and the best treatment plan.
Advanced Neuroimaging Techniques
Advanced neuroimaging is key in diagnosing brain tumors. Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) scans give clear brain images. They show the tumor’s size and how it affects the brain.
MRI is special because it can tell different soft tissues apart. This makes it very useful in studying brain tumors.
Biopsy Procedures and Histological Analysis
A biopsy is often needed to confirm a brain tumor diagnosis. This involves taking a tumor sample for examination. Stereotactic techniques help target the tumor precisely.
The biopsy sample is studied under a microscope. This helps find out if the tumor is cancerous and what type it is. It also guides treatment choices.
Determining Surgical Candidacy
After diagnosing a brain tumor, deciding on surgery is the next step. This choice depends on the tumor’s size, location, and type. The patient’s health and brain function also play a role.
Advanced imaging helps surgeons plan the best surgery. They look at how close the tumor is to important brain areas. Tests like functional MRI (fMRI) help assess surgery risks and benefits.
Preparing for Brain Tumor Surgery
Getting ready for brain tumor surgery is key. It involves several important steps. These steps help make the surgery safe and successful.
Comprehensive Medical Evaluations
Before surgery, patients get detailed medical checks. These checks look at the patient’s health and find any surgery risks.
- Cardiovascular Assessment: This checks the heart health to lower cardiac risks during surgery.
- Neurological Examination: It looks at the brain function to set a baseline and spot any issues.
- Laboratory Tests: Blood tests and other exams are done to check for infections and blood issues.
Medication Management and Adjustments
Managing medications is also very important. Some drugs might need to be changed or stopped to avoid surgery problems.
Patients are usually told to:
- Disclose All Medications: Tell their doctor about all drugs, including ones bought without a prescription.
- Adjust Anticoagulant Medications: Change or stop blood thinners to lower bleeding risks.
- Manage Steroids: Adjust steroid doses to control brain swelling.
Patient Education and Informed Consent
Teaching patients is essential. It makes sure they know about their surgery, its risks, and recovery.
“Informed consent is not just a legal requirement; it’s a key part of patient care. It lets patients make smart choices about their treatment.”
Important parts of patient education include:
- Surgical Risks and Benefits: Talking about the surgery’s possible risks and benefits.
- Pre-Surgical Instructions: Giving clear instructions on how to get ready for surgery, like diet and meds.
- Post-Surgical Care: Teaching patients what to expect after surgery and how to care for themselves at home.
By focusing on these areas, patients can be well-prepared for brain tumor surgery. This reduces risks and improves results.
The Surgical Team: Roles and Responsibilities
The success of brain tumor surgery depends on the team’s skill and teamwork. It takes a group of medical experts working together to get good results.
Neurosurgical Expertise Requirements
Neurosurgeons are key in brain tumor surgery. They need special training and knowledge. They must know a lot about the brain, tumors, and surgery.
Key Skills for Neurosurgeons:
- Advanced knowledge of neuroanatomy
- Proficiency in microsurgical techniques
- Experience with intraoperative monitoring
Interdisciplinary Team Coordination
Brain tumor surgery is a team effort. It includes neurosurgeons, anesthesiologists, nurses, radiologists, and rehab specialists. Working together is key for patient safety and success.
| Team Member | Role |
| Neurosurgeon | Performs the surgical procedure |
| Anesthesiologist | Manages patient anesthesia and vital signs |
| Nurses | Assist during surgery and provide post-operative care |
| Radiologist | Provides diagnostic imaging and intraoperative guidance |
State-of-the-Art Surgical Equipment
Modern brain tumor surgery needs the latest equipment. Tools like intraoperative MRI and navigation systems make surgery safer and more precise.
With skilled neurosurgeons, a well-coordinated team, and cutting-edge tools, hospitals can offer top-notch care for brain tumor patients.
Anesthesia and Patient Positioning for Brain Surgery
Brain surgery needs precise anesthesia protocols and careful patient positioning. This helps in a successful tumor removal. The anesthesia team ensures the patient’s comfort and safety during the surgery.
Anesthesia Protocols for Neurosurgery
Anesthesia for brain surgery is customized for each procedure. It aims to keep the brain well-perfused and avoid pressure increases. Total intravenous anesthesia is often chosen for better control over the patient’s brain state.
The chosen anesthetic agents have minimal effects on blood flow and pressure. Monitoring of vital signs is key. The team must also be ready for complications like swelling or bleeding.
Strategic Patient Positioning
Patient positioning is vital in brain surgery. It affects the team’s access to the tumor. Positions like supine, prone, or lateral are chosen based on the tumor’s location.
Proper positioning includes padding and support to prevent injuries. The team must also consider the patient’s physiological responses. Adjustments are made to prevent complications.
Neuromonitoring Setup
Neuromonitoring is essential during brain surgery. It uses electroencephalography (EEG) and somatosensory evoked potentials (SSEP) to monitor brain activity. This helps detect any neurological damage in real-time.
The setup involves placing electrodes and sensors carefully. This ensures accurate readings. The data helps the surgical team make informed decisions, reducing the risk of neurological injury.
Craniotomy: The Gateway to Brain Tumor Access
Craniotomy is a key surgery that removes part of the skull to reach the brain. It’s vital for treating brain tumors. Surgeons use it to directly tackle tumors.
Scalp Incision and Skull Opening Techniques
The first step is making a scalp incision. It’s planned to get to the tumor with less scarring. Then, the scalp layers are cut, and the skull is exposed.
Skull opening techniques depend on the tumor’s spot and the patient’s body. Sometimes, a bone flap is made and put back. Other times, a part of the skull is removed, called a craniectomy.
For more details on neurosurgery, check out neurosurgical guidelines. They offer deep insights into surgical methods and their uses.
Dural Management and Brain Exposure
Next, the dura mater, the brain’s outer layer, is managed. It’s opened carefully to avoid harming the brain. Dural management is key for safe tumor removal.
Techniques for opening and closing the dura are planned with care. This helps avoid problems and aids in healing.
Minimally Invasive Craniotomy Approaches
New methods in neurosurgery include minimally invasive craniotomy approaches. They aim for smaller incisions and less skull removal. This can cause less damage, lower risks, and quicker recovery.
Choosing between traditional and minimally invasive methods depends on the tumor and the patient’s health. Neurosurgeons pick the best approach for each patient.
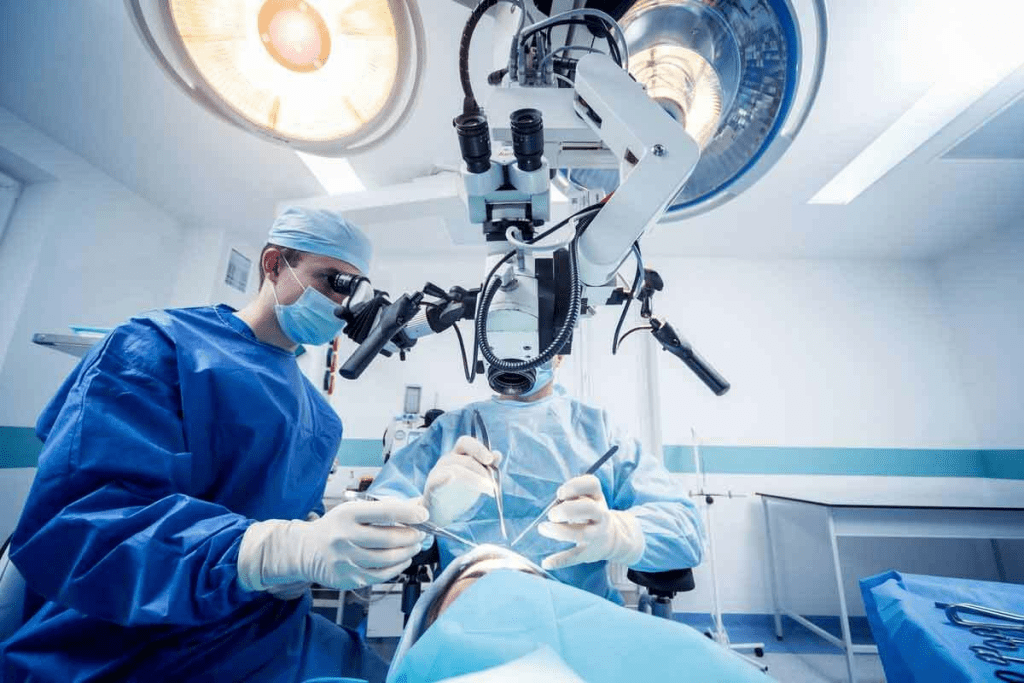
Resection of a Brain Tumor: Surgical Techniques and Protocols
Removing a brain tumor is a delicate task. It involves taking out the tumor while keeping the brain tissue around it safe. This requires advanced surgery and careful planning before the operation.
Microsurgical Dissection and Removal
Microsurgical dissection is key in removing brain tumors. It uses an operating microscope and special tools to carefully separate the tumor from the brain. This method lets neurosurgeons see the tumor and its edges clearly, helping them remove it more accurately.
Key steps in microsurgical dissection include:
- Initial tumor exposure
- Identification of tumor boundaries
- Careful dissection using microsurgical instruments
- Removal of the tumor in a piecemeal fashion or en bloc
Tumor Border Identification Strategies
Finding the edges of a brain tumor is vital for removing it completely without harming the brain. Several methods are used to find these borders, including:
| Strategy | Description |
| Intraoperative MRI | Uses magnetic resonance imaging during surgery to update the tumor’s location and boundaries |
| Fluorescence-Guided Surgery | Employs fluorescent dyes that highlight tumor tissue, making it easier to distinguish from normal brain tissue |
| Neuro-navigation Systems | Utilizes preoperative imaging data to guide the surgeon in real-time during the operation |
Techniques for Preserving Eloquent Brain Areas
Keeping important brain areas safe is essential for brain tumor surgery. Techniques used include:
Awake Craniotomy: Surgery is done with the patient awake. This lets the surgeon watch how the brain works in real time, helping avoid important areas.
By using these advanced methods, neurosurgeons can remove tumors more completely. They also help keep the brain’s functions intact.
Advanced Technologies in Modern Brain Tumor Surgery
The field of brain tumor surgery has seen big changes thanks to new technologies. These advancements have made surgeries more precise and better for patients.
Intraoperative MRI and Navigation Systems
Intraoperative MRI lets surgeons see how much tumor they’ve removed right during surgery. This helps them take out more tumor and avoid harming important brain parts. Navigation systems add to this by showing detailed, 3D images of the brain.
Benefits of Intraoperative MRI:
- Real-time feedback during surgery
- Enhanced accuracy in tumor resection
- Reduced risk of neurological damage
Fluorescence-Guided Tumor Visualization
Fluorescence-guided surgery uses special dyes to light up tumors. This makes it easier for doctors to see and remove tumors. It helps make sure they get all the tumor out.
| Technique | Benefits | Clinical Impact |
| Fluorescence-Guided Surgery | Enhanced visualization of tumor tissue | Improved completeness of tumor resection |
| Intraoperative MRI | Real-time assessment of resection | Reduced risk of neurological damage |
| Laser Ablation | Minimally invasive treatment for deep-seated tumors | Alternative to traditional surgery for inoperable tumors |
Laser Ablation for Deep-Seated Tumors
Laser ablation is a new way to treat hard-to-reach brain tumors. It uses a laser to heat and kill tumor cells. This method is less invasive than traditional surgery.
The advantages of laser ablation include:
- Minimally invasive procedure
- Reduced risk of complications
- Effective treatment for inoperable tumors
These new technologies are big steps forward in brain tumor surgery. They give hope to patients with tough cases.
Intraoperative Monitoring and Brain Mapping
Advanced intraoperative monitoring and brain mapping are key in making brain tumor surgery safer and more effective. These methods help keep the brain’s function intact. This way, patients can recover with fewer problems.
Neurophysiological Monitoring Techniques
Neurophysiological monitoring checks the nervous system’s health during surgery. It includes:
- Electromyography (EMG) to monitor muscle activity
- Electroencephalography (EEG) to assess brain activity
- Somatosensory Evoked Potentials (SSEP) to evaluate sensory pathway function
- Motor Evoked Potentials (MEP) to monitor motor pathway function
Real-time feedback from these methods helps surgeons make better decisions. They can adjust their approach to avoid harming the brain.
Awake Craniotomy for Functional Preservation
An awake craniotomy is a special surgery where the patient stays awake. This lets the team:
- Map brain function in real-time
- Identify and preserve critical areas of the brain
- Maximize tumor removal while minimizing neurological deficits
Patient feedback during awake craniotomy is very helpful. It helps surgeons improve their technique for better results.
Real-Time Assessment of Neural Pathways
Checking neural pathways in real-time is vital for safely removing brain tumors. Techniques like diffusion tensor imaging (DTI) and functional MRI (fMRI) show detailed brain connections and areas.
By combining these advanced imaging methods with monitoring and mapping, surgeons can work with more precision. They can navigate the brain’s complex anatomy with confidence.
Management Options for Inoperable Brain Tumors
Managing inoperable brain tumors needs a mix of advanced treatments and technologies. Surgery is not an option, but other methods can help. These methods can ease symptoms, slow tumor growth, and improve life quality.
Stereotactic Radiosurgery and Radiation Therapy
Stereotactic radiosurgery (SRS) and radiation therapy are key in treating inoperable brain tumors. SRS focuses radiation on the tumor, protecting the brain around it. It works well for smaller tumors.
Radiation therapy might involve treatments spread over time. It’s customized for each patient, based on the tumor’s size and location.
Benefits of SRS and Radiation Therapy:
- Non-invasive treatment option
- High precision in targeting tumors
- Minimal damage to surrounding healthy tissue
Targeted Chemotherapy Protocols
Targeted chemotherapy is another important strategy. It uses drugs that target the tumor’s specific molecular features. This method is more effective and has fewer side effects than traditional chemotherapy.
The right targeted therapy depends on the tumor’s genetic makeup. Research is ongoing to find new targets and improve treatments.
Emerging Treatments and Clinical Trials
New treatments for brain tumors are being explored in clinical trials. These include immunotherapies, gene therapies, and new ways to deliver chemotherapy.
Joining clinical trials can give patients access to new treatments. These treatments might offer better results or a better quality of life.
| Treatment Option | Description | Benefits |
| Stereotactic Radiosurgery (SRS) | Highly focused radiation dose to the tumor | Non-invasive, precise, minimal damage to surrounding tissue |
| Radiation Therapy | Fractionated radiation treatments | Tailored to patient needs, effective for larger tumors |
| Targeted Chemotherapy | Drugs targeting specific tumor molecular characteristics | Effective with fewer side effects, personalized treatment |
Post-Surgical Care and Recovery Journey
The journey after brain tumor surgery is very important. It includes many steps to help the patient get better. These steps help manage any problems and improve brain function.
Immediate Post-Operative Management
Right after surgery, it’s key to avoid problems and make recovery smooth. Patients are watched closely in an ICU or a special neurosurgery ward.
- Monitoring of vital signs and neurological status
- Pain management through medication
- Prevention of infections with antibiotics
A famous neurosurgeon, says, “The care after surgery is as important as the surgery itself.”
“The postoperative period is a time of great vulnerability for the patient, and it requires meticulous attention to detail to prevent complications.”
Recognizing and Addressing Complications
After surgery, some problems can happen. It’s vital to spot and fix them quickly. Issues like infection, swelling in the brain, and brain function problems are common.
| Complication | Symptoms | Management |
| Infection | Fever, wound redness, increased white blood cell count | Antibiotics, possible surgical drainage |
| Cerebral Edema | Headache, confusion, worsening neurological status | Corticosteroids, osmotherapy |
Neurological Rehabilitation Strategies
Rehabilitation is a big part of getting better. It helps patients regain lost brain functions and improve their life quality.
Good rehab includes:
- Physical therapy to improve mobility and strength
- Occupational therapy to regain daily living skills
- Speech therapy for communication disorders
With the right care and rehab, patients can do very well after brain tumor surgery.
Conclusion: The Future of Brain Tumor Surgery
The world of brain tumor surgery is changing fast. New discoveries in neurosurgery and a better understanding of brain tumors are leading the way. We’ve seen how removing a brain tumor is a complex process. It involves making tough decisions, using precise techniques, and caring for patients after surgery.
New technologies are making a big difference. Tools like intraoperative MRI and navigation systems help surgeons find and remove tumors more accurately. Fluorescence-guided tumor visualization and laser ablation for deep tumors are also improving results. These advancements help doctors remove tumors without harming the brain.
The future of brain tumor surgery looks bright. Scientists are working hard to make surgery even better. They aim to improve how well patients recover and find new ways to treat brain tumors. As research continues, there’s hope for better treatments and a brighter future for those with brain tumors.
FAQ
What is the primary goal of brain tumor surgery?
The main aim of brain tumor surgery is to remove the tumor. This is done while keeping the healthy tissue around it safe. The goal is also to keep the brain’s functions working well.
How are brain tumors classified?
Brain tumors are divided into two main types. Malignant tumors grow fast and can spread. Non-malignant tumors grow slower and don’t spread as much. Their location and how they affect the brain also play a role in their classification.
What diagnostic tests are used to identify brain tumors?
To find brain tumors, doctors use MRI scans and biopsies. These tests help figure out if surgery is needed.
Can all brain tumors be removed surgically?
No, not all brain tumors can be taken out by surgery. Some tumors are too close to important brain areas. For these, doctors might suggest other treatments like radiation or chemotherapy.
What is involved in preparing for brain tumor surgery?
Getting ready for surgery includes many steps. Doctors do thorough checks and help manage medicines. They also teach patients about the surgery to get their consent and lower risks.
What techniques are used to resect brain tumors?
Doctors use special techniques to remove tumors. They use microsurgery and try to keep important brain areas safe. This helps keep brain functions working well.
What advanced technologies are used in modern brain tumor surgery?
Modern surgery uses new tech like MRI during surgery and special lights to see tumors. Laser techniques are also used to make surgery safer and more precise.
How is intraoperative monitoring and brain mapping performed?
Monitoring and mapping the brain happen during surgery. Doctors use special tools and keep patients awake to check brain areas. This helps avoid harming important parts of the brain.
What care is required after brain tumor surgery?
After surgery, patients need close care. Doctors watch for any problems and help with recovery. This includes physical therapy to help the brain heal.
What are the management options for inoperable brain tumors?
For tumors that can’t be removed, doctors have other plans. These include radiation, special chemotherapy, and new treatments being tested.
Can benign brain tumors be removed surgically?
Yes, doctors can remove benign tumors. The goal is to take out the tumor and keep the healthy tissue safe.
How is brain tumor removal surgery performed?
Surgery starts with a craniotomy. This means making an incision in the scalp and opening the skull. Then, doctors use microsurgery to remove the tumor.
References
- UC Health. (n.d.). Craniotomy basic level. https://www.uchealth.com/wp-content/uploads/2013/01/PE-Craniotomy_UCNI.pdf
- National Center for Biotechnology Information (NCBI). (2024, October 30). Advancements in imaging and neurosurgical techniques in brain tumor surgery. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11607568/