When you get a brain tumor diagnosis, knowing about the latest in brain tumor surgery is key. It helps you understand your treatment options better.
At Liv Hospital, we focus on you, the patient. We use the latest technology to make brain mass removal safer and more effective. New surgical methods have greatly improved how well patients do.
We aim to remove as much of the tumor as possible while keeping healthy tissue. This way, we help improve your quality.
Key Takeaways
- Modern brain tumor surgery offers improved patient outcomes.
- Liv Hospital’s patient-centered approach ensures complete care.
- State-of-the-art techniques make brain mass removal safer and more effective.
- Our main goal is to remove as much tumor as possible while keeping healthy tissue.
- Advanced surgical methods help improve patients’ quality of life.
Understanding Brain Masses and Tumors
Brain tumors, whether they are cancerous or not, can be very dangerous. Their symptoms can change a lot based on where they are and how big they are. We will look at the different kinds of brain tumors and how they affect health.
Types of Brain Tumors: Malignant vs. Non-Malignant
Brain tumors fall into two main groups: malignant and non-malignant (benign). Malignant brain tumors are cancerous and can spread to other parts of the brain. On the other hand, non-malignant or benign tumors grow more slowly and don’t spread, but they can cause problems because of their size or where they are.
| Characteristics | Malignant Tumors | Non-Malignant Tumors |
| Nature | Cancerous, invasive | Benign, non-invasive |
| Growth Rate | Rapid | Slow |
| Impact on Surrounding Tissue | Can invade or compress the surrounding brain tissue | Typically compresses the surrounding tissue |
| Treatment Approach | Often requires aggressive treatment, including surgery, radiation, and chemotherapy | May be monitored or treated with surgery or radiation, depending on location and symptoms |
Symptoms and Warning Signs
The symptoms of brain tumors can vary a lot. They depend on the tumor’s location, size, and type. Common symptoms include headaches, seizures, and changes in how you think.
Headaches are often worse in the morning and can make you feel sick. Seizures can happen because the tumor irritates the brain. Changes in thinking, like memory loss or trouble concentrating, can also occur.
It’s important to know these symptoms and what they might mean. This helps doctors diagnose and treat brain tumors early. We will keep exploring how to diagnose and treat brain tumors in the next sections.
The Evolution of Brain Cancer Surgery
Brain cancer surgery has seen a big change, thanks to new tech and methods. We’ve moved from simple to complex surgeries. This change has made neurosurgery much better.
Historical Approaches to Brain Tumor Removal
Old brain surgeries were risky and often failed. Surgeons faced many problems, like infections and bleeding. But, the 19th century brought new hope with antiseptics and anesthesia.
As we learned more, so did our ways of removing tumors. New imaging tools helped plan surgeries better. Yet, the methods were not as advanced, leading to poor results.
Technological Breakthroughs in Neurosurgery
Today, neurosurgery has made huge leaps forward. Computer-assisted navigation systems and intraoperative MRI have made surgeries more precise. These tools help find tumors better and watch the surgery as it happens.
Other big steps include:
- Laser Interstitial Thermal Therapy (LITT): A new way to kill tumor cells with laser heat.
- Robotic-assisted surgery: Makes complex surgeries more precise and easier.
- Advanced imaging techniques, like functional MRI, help plan and perform surgeries better.
These new tools have greatly improved patient outcomes. Here are some key stats:
| Technological Advancement | Pre-Advancement Outcomes | Post-Advancement Outcomes |
| Introduction of Antiseptic Practices | High infection rates | Significant reduction in post-operative infections |
| Computer-Assisted Navigation | Less precise tumor localization | Improved accuracy in tumor removal |
| Intraoperative MRI | Limited real-time feedback | Enhanced ability to monitor and adjust during surgery |
These changes have made brain cancer surgery safer and more effective. They’ve helped a lot of patients.
Diagnosis and Surgical Planning
Getting a precise diagnosis and detailed surgical planning are key to treating brain tumors well. When thinking about you can remove a brain tumor, it’s all about the careful steps before surgery.
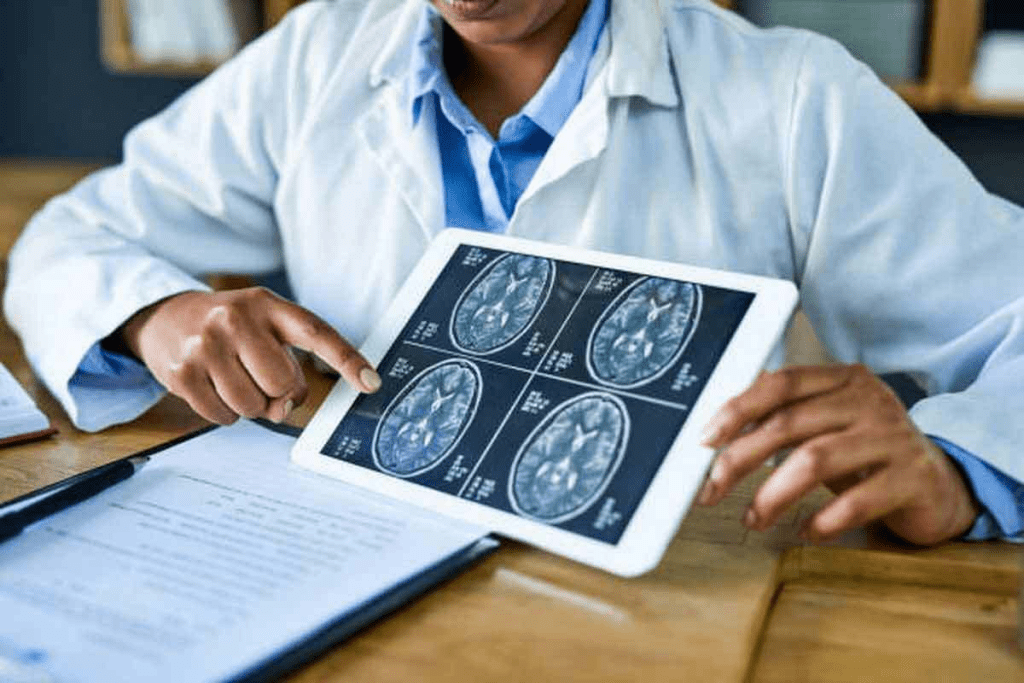
Advanced imaging is vital for finding and planning to remove brain tumors. We use different imaging methods to learn about the tumor and how it affects the brain.
Advanced Imaging Techniques
Tools like MRI and CT scans are key to spotting brain tumors. They give us clear pictures of the tumor’s size, where it is, and how it might affect brain functions. For example, functional MRI (fMRI) helps show which brain areas are important, helping surgeons during the surgery.
The data from these scans is essential for figuring out if surgery is possible and how to do it. Whether it’s removing a benign tumor from the brain or a more complex case, these images are vital.
The Multidisciplinary Tumor Board Approach
After a diagnosis, a team of experts reviews the case to plan the best treatment. This team includes neurosurgeons, oncologists, radiologists, and more. They work together to find the best treatment plan, using their knowledge to consider all aspects of the patient’s health.
When surgery is needed, the team plans it carefully. They think about the tumor’s location and the patient’s health. Their goal is to get the best results, whether that means brain tumor extraction or managing it well.
Brain Mass Removal Surgery Procedures
Removing a brain mass is a detailed process, from start to finish. It can seem scary, but thanks to new tech and methods, results have gotten much better.
Preoperative Preparation
Getting ready for brain mass surgery is key. Preparation is meticulous. Tests like MRI and CT scans help find the tumor’s exact spot and size. Our team looks at your medical history and test results to plan the surgery.
Before surgery, you’ll get advice on what to expect. This includes talking about risks, benefits, and what happens after surgery. You’ll learn about needed care and rehab.
Surgical Approaches to the Brain
Choosing the right surgical approach is important. It depends on the tumor’s location, size, and your health. Our neurosurgeons use methods like craniotomy to reach the brain. They open the skull, remove the tumor, and then close it back up.
The Tumor Resection Process
During tumor resection, our team uses the latest tech. This includes systems that guide the surgery and imaging during it. They aim to remove the tumor safely, without harming the brain.
The success of this surgery depends on our team’s skill and the tech we use. We’re dedicated to giving you the best care for brain surgery for tumor removal.
Innovative Techniques for Brain Surgery Tumor Removal
New methods are changing how brain tumors are treated, giving hope to people all over the world. Neurosurgery is always getting better, thanks to new tech and ways of doing things. This means better results for those having brain tumor surgery.
Awake Craniotomy for Functional Preservation
An awake craniotomy is a complex surgery where the patient stays awake. It lets doctors map brain functions live, keeping important areas safe. It’s great for tumors near brain areas that control speech, movement, or other key functions.
- Real-time brain mapping
- Preservation of critical brain functions
- Reduced risk of post-operative neurological deficits
Laser Interstitial Thermal Therapy
Laser Interstitial Thermal Therapy (LITT) uses laser heat to kill tumor cells. It’s good for tumors deep inside the brain or hard to get to. It’s also for people who can’t have regular surgery.
LITT has many benefits:
- Minimally invasive with smaller incisions
- Reduced risk of infection and complications
- Potential for quicker recovery times
Robotic-Assisted Neurosurgery
Robotic-assisted neurosurgery combines robotics with neurosurgery, making procedures more precise and flexible. Robots offer clear images and allow for detailed work that’s hard with old methods.
The benefits of robotic-assisted neurosurgery are:
- Enhanced precision and accuracy
- Improved visualization through high-definition imaging
- Potential for better outcomes due to minimized human error
These new methods are big steps forward in neurosurgery, giving patients more choices and better chances of success. As tech keeps getting better, we’ll see even more advanced ways to treat brain tumors.
Intraoperative Guidance Technologies
Intraoperative guidance technologies have greatly improved brain tumor surgery. These tools help surgeons navigate the brain’s complex anatomy. This leads to better results in brain tumor removal surgery.
Neuronavigation Systems
Neuronavigation systems are key in modern neurosurgery. They guide surgeons during non-malignant brain tumor surgery with real-time data. These systems use imaging to map the brain, helping locate tumors and important areas.
- Improved accuracy in tumor localization
- Enhanced ability to preserve surrounding brain tissue
- Reduced risk of neurological damage
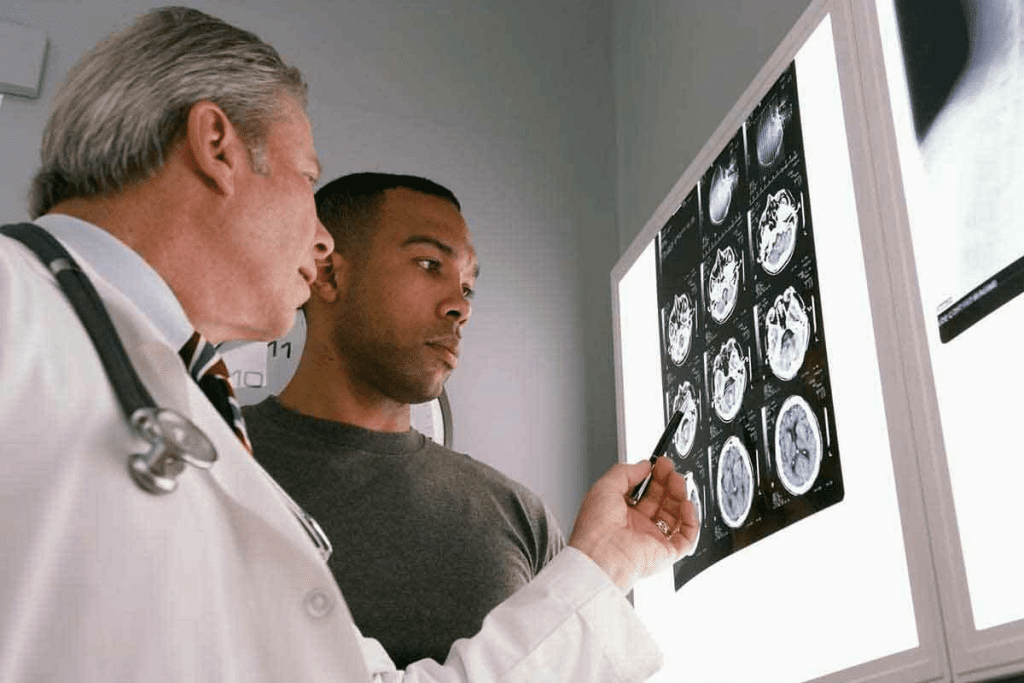
Real-Time Imaging During Surgery
Real-time imaging, like intraoperative MRI, has changed neurosurgery. It lets surgeons see how much tumor is removed during surgery. This helps them make changes to remove more tumor safely.
The benefits of real-time imaging include:
- Immediate feedback on the extent of tumor resection
- Ability to adjust surgical strategy during the procedure
- Enhanced confidence in achieving complete tumor removal
Fluorescence-Guided Surgery
Fluorescence-guided surgery is a new method for how to remove tumors from the brain. It uses a dye that lights up tumor cells, making them easier to see during surgery.
The advantages of fluorescence-guided surgery include:
- Improved visualization of tumor margins
- Enhanced ability to detect residual tumor tissue
- Potential for more complete tumor resection
In conclusion, intraoperative guidance technologies have greatly advanced brain tumor surgery. They give surgeons real-time data and better visualization. This makes brain tumor removal surgery more precise and effective, leading to better patient outcomes.
Maximizing Tumor Removal While Preserving Function
The success of brain tumor surgery depends on a fine balance. It’s about removing the tumor without harming the brain. This balance is key to good outcomes in brain cancer surgery.
Brain Mapping and Cortical Stimulation
Brain mapping and cortical stimulation are vital in brain tumor surgery. Brain mapping creates a detailed brain map. This helps surgeons avoid damaging important brain areas. Cortical stimulation checks brain areas near the tumor during surgery.
Using these methods, surgeons can remove tumors safely. This is very important for tumors near critical brain areas. Here, the difference between the tumor and the normal brain is very small.
Neurophysiological Monitoring
Neurophysiological monitoring gives feedback on the nervous system during surgery. It includes EEG, EMG, and SSEPs. This monitoring helps surgeons avoid damage.
It’s very useful during tumor removal. It lets surgeons quickly spot and fix any issues. This reduces the chance of neurological problems after surgery.
The Balance Between Complete Resection and Safety
The main goal of brain tumor surgery is to remove the tumor completely. But, this must not harm the brain. Sometimes, trying to remove 100% of the tumor is too risky.
Surgeons must think carefully about the benefits and risks. They consider the tumor’s location, size, and how close it is to important brain areas. Techniques like brain mapping and monitoring help make these decisions. They allow for safe tumor removal.
By taking a careful approach to brain tumor surgery, we can improve patient outcomes. This leads to a better quality of life for patients after surgery.
Addressing Inoperable Brain Tumors
When a brain tumor is deemed inoperable, patients and their families face a complex and often daunting treatment journey. This diagnosis can be overwhelming. It’s essential to explore alternative treatment options that can improve patient outcomes.
What Makes a Brain Mass “Inoperable”?
A brain tumor is considered inoperable when it’s located in a sensitive or hard-to-reach area of the brain. This makes surgical removal too risky. Other factors include:
- Tumor size and location
- Proximity to critical brain structures
- Patient’s overall health and medical history
- Tumor type and aggressiveness
Our multidisciplinary team carefully evaluates these factors to determine the best course of treatment.
Alternative Treatment Approaches
For patients with inoperable brain tumors, alternative treatments can provide relief and improve quality of life. These may include:
- Chemotherapy: Targeted chemotherapy can help shrink tumors or slow their growth.
- Radiation Therapy: Advanced radiation techniques, such as stereotactic radiosurgery, can precisely target tumors while minimizing damage to surrounding tissue.
- Palliative Care: Our palliative care team focuses on managing symptoms, pain, and stress to improve patient comfort and well-being.
We also consider clinical trials and emerging therapies that may offer new hope for patients with inoperable brain tumors.
By working together with our patients and their families, we can develop a personalized treatment plan. This plan addresses their unique needs and improves their overall quality of life.
Recovery After Brain Tumor Extraction
The road to recovery after brain tumor surgery is complex. It includes immediate care, rehabilitation, and ongoing check-ups. Each person’s recovery is different and tailored to their needs.
Immediate Post-Operative Care
Right after surgery, care is key. Patients stay in the ICU to watch for any issues. We manage pain, prevent infections, and check on their progress.
Key aspects of immediate post-operative care include:
- Monitoring of vital signs and neurological status
- Pain management through medication
- Prevention of infections using antibiotics
- Early mobilization to prevent complications like deep vein thrombosis
Rehabilitation and Therapy
Rehab is a big part of getting better after surgery. It helps patients regain strength, move better, and think clearly. A team of therapists works together to make a plan just for you.
| Therapy Type | Objective | Benefits |
| Physical Therapy | Improve mobility and strength | Enhances physical function and independence |
| Occupational Therapy | Regain daily living skills | Promotes self-care and daily activity performance |
| Speech Therapy | Enhance communication skills | Improves speech clarity and comprehension |
Long-term Follow-up Protocol
Keeping up with check-ups is important after surgery. We watch for any signs of the tumor coming back. We also manage any lasting effects of the surgery.
Components of the long-term follow-up protocol may include:
- Regular neurological examinations
- Imaging studies (MRI, CT scans)
- Neuropsychological assessments
- Adjustments to the treatment plan as needed
By taking a detailed approach to recovery, we help patients get the best results from brain tumor surgery.
Outcomes and Prognosis Following Brain Tumor Resection
Brain tumor resection outcomes can vary a lot. This depends on the type of tumor and the surgery method. Knowing these factors helps both patients and doctors make better treatment plans.
Factors Affecting Surgical Success
The success of brain tumor removal surgery depends on several things. These include:
- The type and grade of the tumor
- The tumor’s location and size
- The patient’s overall health and age
- The surgical technique used
- The experience of the neurosurgical team
For example, removing a benign tumor from the brain usually has better results than malignant tumor. New surgical methods, like neuronavigation and awake craniotomy, make brain cancer removal safer and more precise.
Survival Rates and Quality of Life
Survival rates after brain tumor resection have improved. This is thanks to new surgery techniques and treatments. Many patients can go back to their usual lives after surgery.
What affects survival and quality of life includes:
- The extent of tumor resection
- The presence of any residual tumor
- The effectiveness of post-operative therapies
- Rehabilitation and support services
Managing Recurrence Risk
It’s important to manage the risk of the tumor coming back after surgery. Regular check-ups and scans are key to catching any recurrence early.
Ways to manage recurrence risk include:
- Adjuvant therapies such as radiation and chemotherapy
- Regular MRI or CT scans for surveillance
- Clinical monitoring for signs of recurrence
- Consideration of clinical trials for novel therapies
By understanding what affects outcomes, patients and doctors can work together. This helps improve care and chances of successful brain tumor removal surgery.
The Future of Removing Tumors From the Brain
We are on the verge of a new era in neurosurgery. Removing brain tumors will become more precise and effective. Emerging technologies and personalized medicine are shaping this future, bringing new hope to patients and doctors.
Emerging Technologies and Techniques
Neurosurgery is changing with new techniques and technology. Some exciting developments include:
- Artificial Intelligence (AI) in Neurosurgery: AI is being used in planning and executing surgeries. It helps make decisions during complex procedures.
- Advanced Imaging Techniques: New imaging, like high-field intraoperative MRI, is improving tumor removal. It also reduces damage to surrounding brain tissue.
- Minimally Invasive Surgery: Techniques like laser interstitial thermal therapy (LITT) are becoming more common. They offer alternatives to traditional surgery for some brain tumors.
Personalized Medicine Approaches
Personalized medicine is changing brain tumor treatment. It tailors treatment plans to each patient’s tumor. This can improve outcomes and reduce recurrence risk.
Key aspects of personalized medicine in brain tumor treatment include:
- Genetic Profiling: Analyzing tumors’ genetic makeup to find specific mutations and therapy targets.
- Tailored Surgical Plans: Creating customized surgical strategies using advanced imaging and data. This maximizes tumor removal while preserving brain function.
- Targeted Therapies: Developing therapies that target specific molecular characteristics of the tumor.
As we advance in these areas, the future of brain tumor removal looks promising. By combining emerging technologies with personalized medicine, we are moving towards a new standard of care. This care is more effective, less invasive, and tailored to each patient’s needs.
Conclusion
Advances in brain surgery for tumors have greatly improved patient results. We’ve looked at how brain cancer surgery has evolved, from old methods to new technologies. Getting a precise diagnosis and planning the surgery are key for success.
New techniques like awake craniotomy and laser therapy have made brain tumor removal more precise. Tools like neuronavigation help surgeons remove tumors while keeping brain function intact. This is a big step forward.
As we keep improving brain cancer surgery, new technologies and personalized medicine are on the horizon. By using the latest surgical methods and care, we can give patients the best chance at recovery. This is a positive outlook for the future of brain surgery.
FAQ
What is brain mass removal surgery?
Brain mass removal surgery, also known as brain tumor resection, is a surgical procedure. It aims to remove a tumor or mass from the brain. This is done while trying to keep healthy brain tissue safe.
What are the goals of brain tumor surgery?
The main goals of brain tumor surgery are to remove as much of the tumor as possible. It also aims to keep neurological function intact. Lastly, it aims to improve the patient’s quality of life.
Can all brain tumors be removed surgically?
No, not all brain tumors can be removed surgically. Some tumors are too big or in the wrong place. In these cases, other treatments might be needed.
What are the symptoms of a brain tumor?
Symptoms of a brain tumor vary. They depend on the tumor’s location, size, and type. Common symptoms include headaches, seizures, weakness, numbness, and changes in cognitive function.
How is a brain tumor diagnosed?
To diagnose a brain tumor, doctors use advanced imaging like MRI, CT scans, and PET scans. They also do a thorough medical evaluation. Sometimes, a biopsy is needed.
What is the role of intraoperative guidance during brain tumor surgery?
Intraoperative guidance technologies help during surgery. They include neuronavigation systems and real-time imaging. These tools help surgeons find and remove tumors safely, without harming nearby brain tissue.
What are some innovative techniques used in brain surgery for tumor removal?
New techniques include awake craniotomy, laser interstitial thermal therapy, and robotic-assisted neurosurgery. These methods can improve results and reduce recovery time.
How can tumor removal be maximized while preserving neurological function?
To remove tumors while keeping brain function intact, doctors use brain mapping and cortical stimulation. They also use neurophysiological monitoring. These methods help identify and protect important brain areas.
What is the recovery process like after brain tumor extraction?
After surgery, the recovery process includes immediate care, rehabilitation, and therapy. It also involves long-term follow-up to watch for recurrence and manage symptoms.
What are the outcomes and prognosis following brain tumor resection?
Outcomes and prognosis vary. They depend on the tumor type, size, and location. They also depend on the patient’s overall health and how well they respond to treatment.
Can brain tumors recur after surgery?
Yes, brain tumors can come back after surgery. Managing the risk of recurrence is a key part of ongoing care.
What emerging technologies are being used in brain tumor removal?
New technologies include better imaging, robotics, and personalized medicine. These advancements are expected to improve care and outcomes.
How is brain mass removal surgery performed?
The surgery involves preparation before the operation. It also includes the surgical approach and the tumor removal process. The goal is to safely remove as much of the tumor as possible.
What is the difference between malignant and non-malignant brain tumors?
Malignant brain tumors are cancerous and grow fast. Non-malignant tumors grow more slowly and may not be cancerous. But they can cause symptoms and need treatment.
References
- Carll, J., et al. (2025). Guideline of guidelines: PSMA PET in staging newly diagnosed intermediate-risk prostate cancer. BJU International. https://pubmed.ncbi.nlm.nih.gov/40704877/
- Jochumsen, M. R., et al. (2024). PSMA PET/CT for primary staging of prostate cancer: A systematic review and meta-analysis. European Urology, 85(3), 245“256. https://www.sciencedirect.com/science/article/pii/S0001299823000557