Dementia and Alzheimer’s disease are often confused, but they’re not the same. Dementia is a broad term that means a big drop in how well someone thinks. It includes losing memory, getting confused, and having trouble solving problems or making decisions.
Alzheimer’s disease is the main reason for dementia. It’s a big problem for many people. In 2025, 7.2 million Americans over 65 will have Alzheimer’s dementia. This shows how big of an issue it is for both people and society.
Key Takeaways
- Dementia is a general term for a decline in cognitive function.
- Alzheimer’s disease is the most common cause of dementia.
- The prevalence of Alzheimer’s dementia is expected to reach 7.2 million in Americans aged 65 and older by 2025.
- Understanding the distinction between dementia and Alzheimer’s is key for good care and planning.
- Early diagnosis and action can really help improve life for those affected.
Understanding Dementia and Alzheimer’s: An Overview

Exploring the world of cognitive disorders, it’s key to grasp the difference between dementia and Alzheimer’s. These conditions touch millions globally, affecting not just those diagnosed but also their loved ones and caregivers.
The Global Impact of Cognitive Disorders
Dementia’s global numbers are set to hit over 150 million by 2050. This alarming rise highlights the urgent need for awareness, early detection, and effective management.
- Dementia impacts more than just memory; it affects daily life and overall well-being.
- The financial toll of dementia is huge, with costs expected to skyrocket in the future.
- It’s essential to understand dementia and its types, like Alzheimer’s, to create targeted treatments.
Why Understanding the Difference Matters
Alzheimer’s is the leading cause of dementia, but not all dementia is Alzheimer’s. Knowing the difference is critical for:
- Accurate diagnosis and understanding the future
- Creating personalized treatment plans
- Improving patient care and support
By recognizing the differences, healthcare professionals can provide more precise and effective care. This leads to better outcomes for those dealing with these conditions.
Defining Dementia: A Syndrome of Symptoms

Dementia is a decline in cognitive function that affects daily activities. It’s not a single disease but a group of symptoms. These symptoms include memory loss and thinking problems. It’s a major cause of disability and dependency in older adults worldwide.
What Constitutes Dementia
Dementia includes various cognitive disorders. Symptoms include memory loss, confusion, and difficulty with communication and problem-solving. These issues make daily life hard, affecting independence.
The degenerative nature of dementia means symptoms get worse over time. This is different from normal aging.
Doctors diagnose dementia by checking cognitive and functional abilities. They look for significant decline in daily tasks like managing money and personal care.
Common Manifestations of Dementia
Symptoms of dementia vary, but common ones include:
- Memory loss that affects daily life, such as forgetting recent events or learning new information.
- Confusion and disorientation, which can lead to difficulty understanding the time of day, the day of the week, or the month.
- Difficulty with communication, including finding the right words or following conversations.
- Problem-solving challenges, such as managing finances or making decisions.
- Changes in mood and personality, such as becoming easily agitated, anxious, or withdrawn.
It’s important to understand these symptoms to tell dementia apart from other cognitive disorders, like Alzheimer’s disease. While Alzheimer’s is a common cause, not all dementia is Alzheimer’s. Knowing the difference helps in getting the right diagnosis and treatment.
Alzheimer’s Disease: The Most Common Form of Dementia
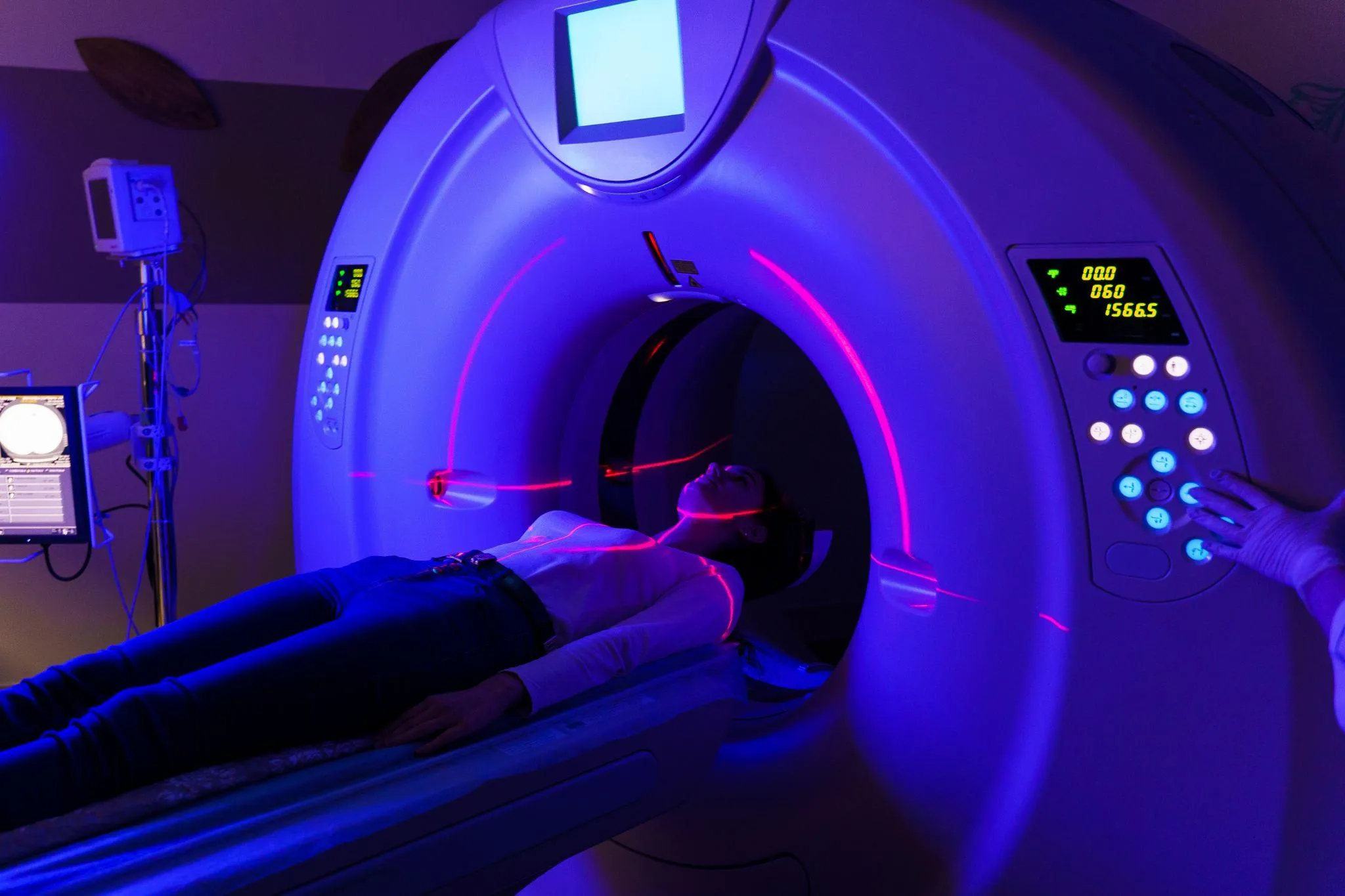
<SEP-14226_image_4>
We are going to explore Alzheimer’s disease, a condition that accounts for the majority of dementia cases. It is a progressive neurological disorder that causes brain cells to degenerate and die. This leads to a decline in thinking, behavioral, and social skills.
This decline is significant because it affects memory, cognitive functions, and the ability to perform daily tasks. Alzheimer’s disease accounts for 60–80% of dementia cases, making it the most common form of dementia among older adults.
The Discovery and Naming of Alzheimer’s Disease
Alzheimer’s disease was first identified in 1906 by Alois Alzheimer, a German psychiatrist and neuropathologist. He described the condition after examining the brain tissue of a woman who had died of an unusual mental illness. The examination revealed abnormal clumps and tangled bundles of fibers in her brain, which are now known as amyloid plaques and neurofibrillary tangles, respectively.
These hallmark features of Alzheimer’s disease are critical in understanding its pathology. The discovery and subsequent research into Alzheimer’s have significantly advanced our understanding of dementia and its various forms.
How Alzheimer’s Affects the Brain
Alzheimer’s disease affects the brain in several ways, leading to the manifestation of various symptoms associated with dementia. The progression of Alzheimer’s involves the accumulation of amyloid beta plaques and tau tangles in the brain, which disrupts the normal functioning of brain cells.
- The hippocampus, a region critical for memory formation, is often affected early in the disease.
- As the disease progresses, other areas of the brain are impacted, leading to a wide range of cognitive and behavioral symptoms.
- Symptoms can include memory loss, confusion, difficulty with communication, problem-solving, and judgment.
Understanding how Alzheimer’s affects the brain is key for developing effective treatments and management strategies for Alzheimer’s disease symptoms. Research continues to uncover the complexities of this disease, bringing hope for improved care and support for those affected.
The Key Difference Between Alzheimer’s and Dementia
It’s important to know the difference between Alzheimer’s disease and dementia. They are not the same, even though people often mix them up. Each has its own place in the world of brain health.
<SEP-14226_image_5>
Relationship: Category vs. Specific Condition
Dementia is a term that covers a range of symptoms. These include memory loss and trouble with communication and problem-solving. It’s not a single disease but a group of symptoms caused by different things.
Alzheimer’s disease, though, is a specific condition. It’s the main reason for dementia, causing 60-80% of cases.
Key characteristics of dementia include:
<SEP-14226_image_6>
- Memory loss
- Difficulty with communication and language
- Problem-solving challenges
- Impaired judgment and decision-making
Alzheimer’s disease is marked by amyloid beta plaques and tau tangles in the brain. These cause damage and death to brain cells. It gets worse over time.
Why This Distinction Matters for Diagnosis and Treatment
Knowing if someone has dementia or Alzheimer’s is key. It helps doctors find the right cause of symptoms. It also guides treatment plans, as different causes need different approaches.
“Accurate diagnosis is the foundation of effective care for individuals with cognitive impairments.” This shows why it’s important to tell dementia and Alzheimer’s apart.
This difference also affects how we care for patients. Knowing the exact diagnosis helps families and caregivers. They can then provide the right support.
The main reasons this distinction matters include:
- Accurate diagnosis
- Targeted treatment approaches
- Better patient and caregiver support
Types of Dementia Beyond Alzheimer’s
Dementia is not just Alzheimer’s disease. It also includes vascular dementia and Lewy body dementia, among others. Knowing about these different types is key to giving the right care and support.
<SEP-14226_image_7>
Dementia is a syndrome, not a single disease. It leads to a decline in cognitive function. This includes memory loss, trouble with communication, and problem-solving. Each type of dementia has its own causes, symptoms, and how fast it progresses.
Vascular Dementia
Vascular dementia is the second most common dementia after Alzheimer’s. It happens when blood flow to the brain is reduced, often due to a stroke. Symptoms include trouble with planning, decision-making, and memory.
Key characteristics of vascular dementia:
- Caused by reduced blood flow to the brain
- Often associated with stroke or small vessel disease
- Symptoms can vary depending on the area of the brain affected
Lewy Body Dementia
Lewy body dementia is marked by abnormal protein clumps in the brain. Symptoms include visual hallucinations, changes in cognitive function, and Parkinson’s-like motor symptoms.
Key characteristics of Lewy body dementia:
- Presence of Lewy bodies in the brain
- Visual hallucinations and fluctuating cognitive function
- Parkinson’s-like motor symptoms
Frontotemporal Dementia
Frontotemporal dementia involves the degeneration of the frontal and temporal lobes. Symptoms include changes in personality, behavior, and language.
Key characteristics of frontotemporal dementia:
- Affects the frontal and temporal lobes
- Changes in personality, behavior, and language
- Often occurs at a younger age than Alzheimer’s
Mixed Dementia
Mixed dementia is when someone has more than one type of dementia, like Alzheimer’s and vascular dementia. Symptoms can be a mix of those from each dementia.
Key characteristics of mixed dementia:
- Presence of more than one type of dementia
- Combination of symptoms from individual dementias
- Can be challenging to diagnose
|
Type of Dementia |
Key Characteristics |
Common Symptoms |
|---|---|---|
|
Vascular Dementia |
Caused by reduced blood flow to the brain |
Difficulty with planning, decision-making, memory |
|
Lewy Body Dementia |
Presence of Lewy bodies in the brain |
Visual hallucinations, fluctuating cognitive function, Parkinson’s-like motor symptoms |
|
Frontotemporal Dementia |
Affects the frontal and temporal lobes |
Changes in personality, behavior, language |
|
Mixed Dementia |
Presence of more than one type of dementia |
Combination of symptoms from individual dementias |
Comparing Symptoms: How Alzheimer’s Differs from Other Dementias
It’s important to know how Alzheimer’s symptoms differ from other dementias. Both affect memory and thinking, but they show up and get worse in different ways.
<SEP-14226_image_8>
Early Warning Signs of Alzheimer’s
Alzheimer’s starts with small signs that can be missed. Early signs include memory loss, like forgetting new info or important dates. People might also struggle with solving problems or making good choices.
They might feel sad or change how they act. They might also pull back from seeing friends or family.
These signs start off small but get worse over time. They can really change how someone lives their day-to-day life.
Symptom Patterns in Other Forms of Dementia
Other dementias, like vascular dementia, Lewy body dementia, and frontotemporal dementia, have their own signs. For example:
- Vascular dementia happens when the brain doesn’t get enough blood. It makes it hard to plan or make decisions.
- Lewy body dementia causes ups and downs in thinking, seeing things that aren’t there, and acting like someone with Parkinson’s disease.
- Frontotemporal dementia messes with the brain’s front and sides. It changes how someone acts, talks, and thinks.
Knowing these different signs is key to figuring out what kind of dementia someone has. It helps doctors give the right treatment.
Risk Factors and Causes
It’s important to know the risk factors for dementia and Alzheimer’s to catch them early. We see that some risks are the same, but there are also differences.
Common Risk Factors for All Dementias
Many risk factors are the same for different types of dementia. Age is the biggest risk, with more chances of getting dementia after 65. Other common risks include:
- Family history of dementia
- Genetic predispositions, like certain gene variants
- Lifestyle choices, like not being active, smoking, and eating poorly
- Other health issues, like diabetes, high blood pressure, and heart disease
We can often change these factors through lifestyle changes and medical care.
Specific Risk Factors for Alzheimer’s Disease
Alzheimer’s has some unique risk factors. These include:
- The APOE-e4 gene variant, linked to higher Alzheimer’s risk
- Severe head injuries, if you lost consciousness
- Heart disease risk factors, like high blood pressure and obesity
Studies also show that less education and not doing mentally challenging activities can increase Alzheimer’s risk.
|
Risk Factor |
Dementia |
Alzheimer’s Disease |
|---|---|---|
|
Age |
Significant risk factor |
Significant risk factor |
|
Family History |
Common risk factor |
Common risk factor |
|
APOE-e4 Gene Variant |
Less specific |
Significant risk factor |
|
Lifestyle Factors |
Common risk factor |
Common risk factor |
Knowing these risk factors helps us spot who’s at higher risk. We can then try to lower their chance of getting dementia or Alzheimer’s.
Diagnosis: Identifying Alzheimer’s vs. Other Dementias
Understanding how to diagnose Alzheimer’s and other dementias is key for good care. Accurate diagnosis is vital for the right treatment and support.
The Diagnostic Process
The process to diagnose Alzheimer’s and other dementias is detailed. It includes a medical history, physical exam, and various tests. This approach helps rule out other causes and pinpoint the dementia type.
First, we take a detailed medical history and do a physical exam. We look for any health issues that might cause cognitive decline. We also talk to the patient and their family to learn about symptoms and daily life.
Cognitive Assessments and Neurological Exams
Cognitive assessments are a big part of diagnosing. They check memory, language, problem-solving, and judgment. We use tests like the Mini-Mental State Examination (MMSE) to see how well the brain is working.
Neurological exams check the nervous system for any problems. They look at reflexes, muscle strength, and coordination.
Brain Imaging and Biomarkers
Brain imaging, like MRI and PET scans, is very important. These tests show the brain’s structure and function. They help find any signs of Alzheimer’s or other dementias.
Biomarkers, like beta-amyloid and tau proteins, also help diagnose Alzheimer’s. We can measure these through cerebrospinal fluid analysis or PET scans.
The table below shows the main ways we diagnose Alzheimer’s and other dementias:
|
Diagnostic Approach |
Description |
|---|---|
|
Medical History and Physical Examination |
Identifies underlying medical conditions that could be contributing to cognitive decline. |
|
Cognitive Assessments |
Evaluates cognitive function, including memory, language, and problem-solving. |
|
Neurological Exams |
Assesses abnormalities in the nervous system that could be contributing to cognitive decline. |
|
Brain Imaging (MRI, PET) |
Visualizes the brain’s structure and function to identify abnormalities. |
|
Biomarkers (Beta-amyloid, Tau) |
Supports the diagnosis of Alzheimer’s disease through measurement of specific proteins. |
Treatment Approaches for Different Types of Dementia
Managing dementia and Alzheimer’s needs a personalized plan. Knowing the difference between Alzheimer’s and dementia is key. This helps choose the right treatment.
Medications for Alzheimer’s Disease
For Alzheimer’s, several medicines help manage symptoms. These include:
- Cholinesterase inhibitors (e.g., donepezil, rivastigmine) to improve cognitive function.
- Memantine to slow down symptoms in moderate to severe Alzheimer’s.
- Combination therapy using both cholinesterase inhibitors and memantine for better results.
These medicines can improve cognitive and functional symptoms. They help patients live better lives.
Treatments for Other Forms of Dementia
Other dementia types need different treatments. For example:
|
Type of Dementia |
Treatment Approach |
|---|---|
|
Vascular Dementia |
Managing risk factors like hypertension and diabetes with lifestyle changes. |
|
Lewy Body Dementia |
Using cholinesterase inhibitors; avoiding antipsychotic drugs due to sensitivity. |
|
Frontotemporal Dementia |
Speech therapy and behavioral management; no specific medication is approved yet. |
It’s important to know the specific dementia type for the best treatment. We also use non-pharmacological methods. These include cognitive training, exercise, and caregiver support, which help many dementia types.
With a complete treatment plan, we can better the lives of patients with dementia.
The Progression: How Alzheimer’s and Other Dementias Advance
It’s important to know how Alzheimer’s and other dementias get worse. This knowledge helps patients, caregivers, and doctors. We’ll look at how Alzheimer’s and other dementias change over time. This includes the stages of Alzheimer’s and how other dementias progress differently.
Stages of Alzheimer’s Disease
Alzheimer’s disease goes through several stages. Each stage shows different levels of thinking and doing things problems.
- Early-stage Alzheimer’s: Symptoms include memory loss, getting confused, and trouble with talking.
- Moderate Alzheimer’s: Patients may get more confused, have trouble solving problems, and feel mood swings.
- Late-stage Alzheimer’s: At the end, people need constant care. They can’t respond to their surroundings or do daily tasks.
Progression Patterns in Other Dementias
Other dementias, like vascular dementia, Lewy body dementia, and frontotemporal dementia, also get worse but at different speeds. They show different symptoms too.
- Vascular Dementia: It gets worse in steps, with big drops in thinking skills after strokes or mini-strokes.
- Lewy Body Dementia: It’s marked by ups and downs in thinking, seeing things that aren’t there, and acting like Parkinson’s.
- Frontotemporal Dementia: It mainly changes personality, behavior, and how someone talks.
Research keeps going, and we learn more about how these diseases get worse. Studies show that Alzheimer’s and other dementias damage and kill brain cells. By understanding this, we can create better help and support for those affected.
Prevalence and Statistics: The Growing Impact
Alzheimer’s disease and dementia are big health issues. They are expected to get worse as more people get older. We need to act fast to tackle this problem.
In the U.S., over 6 million people have Alzheimer’s. This number could hit 13.8 million by 2050. Worldwide, about 50 million people live with dementia.
Current Numbers and Future Projections in the United States
Alzheimer’s is a big worry in the U.S. Here are some facts:
- More than 6 million Americans have Alzheimer’s dementia.
- 1 in 3 seniors die with Alzheimer’s or another dementia.
- Alzheimer’s is the 6th leading cause of death in the U.S.
- The cost for healthcare, long-term care, and hospice for Alzheimer’s and other dementias is $355 billion in 2021.
As more people get older, these numbers will go up. By 2050, there could be 13.8 million people aged 65 and older with Alzheimer’s.
Global Burden and Demographic Patterns
Dementia is a big problem worldwide. Here are some key facts:
- About 50 million people worldwide have dementia.
- There are nearly 10 million new cases every year, with one new case every 3.2 seconds.
- The cost of dementia globally is over $1 trillion a year.
The biggest risk for dementia is age. As more people get older, dementia will become even more common. This is true, but even more so in low- and middle-income countries.
We must keep working on research, care, and support for Alzheimer’s and dementia. Knowing the numbers helps us prepare for the future. We can work to lessen the impact of these diseases.
Economic and Social Burden of Dementia and Alzheimer’s
Dementia and Alzheimer’s have a big impact on people, families, and society. They affect more than just health, touching many areas of life. This includes healthcare costs, the burden on caregivers, and social effects.
Healthcare Costs and Economic Impact
In 2019, dementia cost the world $1.3 trillion USD. This number is expected to grow as more people get older. The costs come from medical care, lost work time, and unpaid care from family and friends.
Here’s a table showing the different parts of the economic burden:
|
Cost Component |
Estimated Cost (USD) |
Percentage of Total Cost |
|---|---|---|
|
Direct Medical Costs |
$215 billion |
16.5% |
|
Informal Care Costs |
$470 billion |
36.2% |
|
Direct Social Care Costs |
$150 billion |
11.5% |
|
Lost Productivity |
$645 billion |
49.6% |
Caregiver Burden and Social Implications
Dementia and Alzheimer’s also have a big social impact, mainly on caregivers. Caregivers do more than just take care of the person. They also provide emotional support and sometimes help with money matters. This can lead to burnout and a lower quality of life for caregivers.
The effects are not just on the person with dementia but also on their loved ones and communities. We need better support systems. These should help both those with dementia and their caregivers.
Understanding the economic and social effects of dementia and Alzheimer’s is key. We need to invest in research and improve healthcare and social services. Supporting caregivers and families is also important.
Research Frontiers: Advances in Understanding and Treating Dementia
Research on dementia and Alzheimer’s is moving forward fast. New ways to treat these diseases are being found. This progress is thanks to advanced research and new treatment methods.
Emerging Therapies for Alzheimer’s Disease
New treatments for Alzheimer’s are being looked into. These include immunotherapies and gene therapies. They aim to tackle the root causes of the disease.
Immunotherapy uses antibodies to fight amyloid-beta plaques. Clinical trials are underway to see if these treatments work and are safe.
Innovative Approaches for Other Dementias
Research is also focusing on other types of dementia. For vascular dementia, managing heart health is key.
Studies on Lewy body dementia are exploring alpha-synuclein pathology. This could lead to new treatments.
Prevention Strategies: Reducing Risk for All Types of Dementia
To lower dementia risk, we need to change our lifestyle and manage health issues. Understanding dementia and Alzheimer’s helps us see how important prevention is.
Lifestyle Modifications and Brain Health
Changing our lifestyle can greatly improve brain health and lower dementia risk. Here are some key changes:
- Regular Physical Activity: Exercise helps keep our minds sharp.
- Healthy Diet: Eating lots of fruits, veggies, and whole grains, like the Mediterranean diet, can help.
- Cognitive Stimulation: Doing brain games and puzzles can build up our brain’s strength.
- Social Engagement: Staying connected and active socially is good for our brain.
By making these lifestyle changes, we can take steps to protect our brains from dementia.
Managing Comorbid Conditions
It’s also key to manage other health issues to lower dementia risk. Problems like diabetes, high blood pressure, and heart disease can harm our brain if not controlled.
|
Comorbid Condition |
Management Strategy |
Impact on Dementia Risk |
|---|---|---|
|
Diabetes |
Monitoring blood sugar levels, medication adherence |
Reduces risk of cognitive decline |
|
Hypertension |
Lifestyle changes, medication |
Lowers risk of vascular dementia |
|
Heart Disease |
Medication, lifestyle modifications, surgical interventions |
Reduces overall cardiovascular risk, potentially lowering dementia risk |
By managing these health issues well, we can lower our chance of getting dementia.
Conclusion: Understanding the Distinction for Better Care
Knowing the difference between dementia and Alzheimer’s is key for correct diagnosis and care planning. Dementia is a wide term for many cognitive disorders. Alzheimer’s disease is a specific type of dementia. This difference helps healthcare providers create better treatment plans and support for those affected.
With over 7 million Americans living with Alzheimer’s, the need to understand this difference is huge. This number is expected to rise to nearly 13 million by 2050. For more facts and figures, visit the Alzheimer’s Association website. By knowing the unique traits of each condition, we can improve the lives of those affected.
FAQ
What is the main difference between Alzheimer’s disease and dementia?
Alzheimer’s disease is a type of dementia. Dementia is a broader term. It includes memory loss, confusion, and trouble with communication and problem-solving.
Is Alzheimer’s disease the same as dementia?
No, they are not the same. Alzheimer’s is a specific condition that causes dementia symptoms. But not all dementia is Alzheimer’s.
What are the common symptoms of dementia?
Symptoms include memory loss, confusion, and trouble with communication. You might also see changes in mood and behavior.
What are the risk factors for developing Alzheimer’s disease and other dementias?
Risk factors include age and genetics. Lifestyle factors like not being active and smoking also play a role. Certain medical conditions, like diabetes, are also risks.
How is Alzheimer’s disease diagnosed?
Doctors use cognitive tests, neurological exams, and brain imaging. They also do lab tests to rule out other causes.
Are there different types of dementia?
Yes, there are several types. These include Alzheimer’s disease, vascular dementia, and Lewy body dementia. Frontotemporal dementia and mixed dementia are also types.
Can dementia be prevented?
While prevention is not guaranteed, making lifestyle changes can help. Managing health conditions is also important.
What are the current treatment options for Alzheimer’s disease and other dementias?
Treatments include medications and non-pharmacological interventions. Lifestyle changes are also part of the treatment plan.
How does Alzheimer’s disease progress?
It progresses through stages, from mild cognitive impairment to severe dementia. The rate of progression varies among individuals.
What is the economic and social burden of dementia and Alzheimer’s disease?
The burden includes healthcare costs and caregiver burden. It also affects families and society, leading to broader social implications.
What is the economic and social burden of dementia and Alzheimer’s disease?
The burden includes healthcare costs and caregiver burden. It also affects families and society, leading to broader social implications.
What is degenerate in the context of Alzheimer’s and dementia?
“Degenerate” means the progressive deterioration of cognitive and functional abilities. It leads to a decline in overall health and well-being.
References
• Alzheimer’s Association. 2025 Alzheimer’s disease facts and figures (executive summary). https://www.alz.org/getmedia/c05f7ba4-9aea-4cb0-8898-5e8bff3f0930/executive-summary-2025-alzheimers-disease-facts-and-figures.pdf
• Alzheimer’s Association. Alzheimer’s Disease Facts and Figures. https://www.alz.org/alzheimers-dementia/facts-figures
• JAMA Network Open. Maximizing Early Dementia Detection Through Medicare Annual Wellness Visits. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2834750
• Alzheimer’s & Dementia (PMC). 2025 Alzheimer’s disease facts and figures. https://pmc.ncbi.nlm.nih.gov/articles/PMC12040760/
• World Health Organization (WHO). Dementia. https://www.who.int/news-room/fact-sheets/detail/dementia