Amyloidosis is a rare disorder found in about 5-9 cases per million people each year. Its symptoms are not specific, which often leads to wrong diagnoses. This delay can be harmful. Amyloidosis symptoms are often mistaken for other issues. Learn the amazing facts to ensure a perfect and fast medical diagnosis today. Amyloidosis symptoms are often mistaken for other issues. Learn the amazing facts to ensure a perfect and fast medical diagnosis today.
At Liv Hospital, we use the latest medical methods and knowledge to better diagnose amyloidosis. Knowing what amyloidosis can look like is key for doctors to make the right choices.
By diving into the details of amyloidosis, we can get better at diagnosing and treating it. This helps patients get better faster. It also shows how important it is to have thorough medical care for rare diseases.
Key Takeaways
- Amyloidosis is a rare disorder with nonspecific symptoms.
- Misdiagnosis is common due to its ability to mimic other conditions.
- Liv Hospital uses advanced protocols for accurate diagnosis.
- Understanding clinical mimics is key for timely management.
- Comprehensive care is essential for improving patient outcomes.
Understanding Amyloidosis: A Rare but Serious Condition

Amyloidosis is a group of diseases caused by abnormal amyloid proteins. These proteins build up in tissues, causing damage and organ problems. This buildup disrupts the normal function of organs and tissues.
Definition and Prevalence of Amyloidosis
Amyloidosis is a rare condition where amyloid proteins accumulate. It affects about 5-9 people per million each year. Amyloidosis can harm organs like the kidneys, heart, and nervous system, leading to many symptoms.
The Process of Amyloid Protein Deposition
The buildup of amyloid proteins starts with misfolded proteins. These proteins then form insoluble fibrils. These fibrils damage tissues and disrupt organ function.
Several factors contribute to amyloid deposition:
- Genetic mutations that lead to abnormal proteins
- Chronic diseases that cause ongoing inflammation
- Age-related changes that affect protein folding and clearance
Understanding amyloidosis is key to finding better treatments. Knowing what causes it helps doctors manage the disease better. This can slow down how fast it progresses.
Types of Amyloidosis and Their Distinct Features
It’s important to know the different types of amyloidosis for accurate diagnosis and treatment. Amyloidosis is not just one disease. It includes several conditions where amyloid proteins build up in tissues.
AL (Primary) Amyloidosis
AL amyloidosis, or primary amyloidosis, happens when the bone marrow makes abnormal light chain proteins. These proteins can harm various organs. Key features include:
- Association with plasma cell dyscrasias
- Multi-organ involvement
- Variable clinical presentation
AA (Secondary) Amyloidosis
AA amyloidosis is linked to chronic inflammation or infections. It’s caused by serum amyloid A protein, an acute-phase reactant. Common underlying conditions include:
- Chronic infections (e.g., tuberculosis)
- Inflammatory diseases (e.g., rheumatoid arthritis)
- Chronic inflammatory bowel disease
Hereditary Amyloidosis
Hereditary amyloidosis comes from genetic mutations. It affects the production of abnormal transthyretin (TTR) or other proteins. Notable aspects include:
- Autosomal dominant inheritance
- Variable age of onset
- Often involves the peripheral nerves and heart
Wild-type ATTR Amyloidosis
Wild-type ATTR amyloidosis affects older males without a known genetic mutation. It’s characterized by the buildup of wild-type transthyretin amyloid in the heart and other tissues. Key characteristics include:
- Predominantly affects older males
- Cardiac involvement is common
- Slowly progressive
Knowing the different types of amyloidosis is key for proper diagnosis and treatment. We will look at their clinical signs and diagnostic challenges in the next sections.
Amyloidosis Symptoms: Recognizing the Warning Signs
The symptoms of amyloidosis are often hard to spot, making it tough to diagnose. It’s important to catch these signs early to help patients.
General Systemic Manifestations
Amyloidosis can show up in many ways, not always clearly. Symptoms include:
- Weight loss: Losing weight without trying is common, showing the body’s struggle.
- Fatigue: Feeling tired or weak is common, as organs are affected.
- Swelling: Swelling in legs and feet can happen due to kidney or heart issues.
Organ-Specific Symptoms
When amyloid proteins build up in organs, specific symptoms appear:
- Cardiac Involvement: Shortness of breath and heart problems are signs of heart amyloidosis.
- Renal Involvement: Too much protein in the urine and kidney failure are signs of kidney amyloidosis.
- Neurological Symptoms: Numbness, tingling, and pain in hands and feet can be signs of nerve involvement.
Progressive Nature of the Disease
Amyloidosis gets worse over time if not treated. How fast it progresses varies by person and organ affected. Early treatment can greatly improve life quality and chances of recovery.
It’s key to watch for amyloidosis signs to offer timely care. Knowing the symptoms helps doctors make better decisions and improve patient results.
The Diagnostic Challenge: Why Amyloidosis Is Frequently Misdiagnosed

Diagnosing amyloidosis is hard because its symptoms are not clear and it’s rare. The symptoms can look like many other diseases. This makes it hard to get a correct diagnosis.
Non-specific Symptom Presentation
Amyloidosis symptoms are not clear and can look like many other diseases. For example, feeling tired, losing weight, and swelling can be signs of many things. So, patients often get tested for many diseases before amyloidosis is thought of.
Because the symptoms are not clear, patients see many doctors before they get a diagnosis. This can make things worse for the patient.
Rarity of the Condition
Amyloidosis is rare, which makes it hard to diagnose. Doctors might not know much about it because they rarely see it. Studies show that up to 34% of patients thought to have AL amyloidosis actually have something else.
- Because amyloidosis is rare, doctors might not know how to diagnose it.
- This lack of knowledge can cause delays in diagnosis and wrong treatment.
Limitations in Diagnostic Testing
Testing for amyloidosis has its own problems. The best test, a tissue biopsy with Congo red staining, is invasive. Also, not all tests are perfect, and some can give false negatives.
We need to understand these challenges when dealing with unclear symptoms. Knowing how hard it is to diagnose amyloidosis helps us improve our diagnosis and treatment.
Heart Failure and Cardiomyopathies: Common Cardiac Misdiagnoses
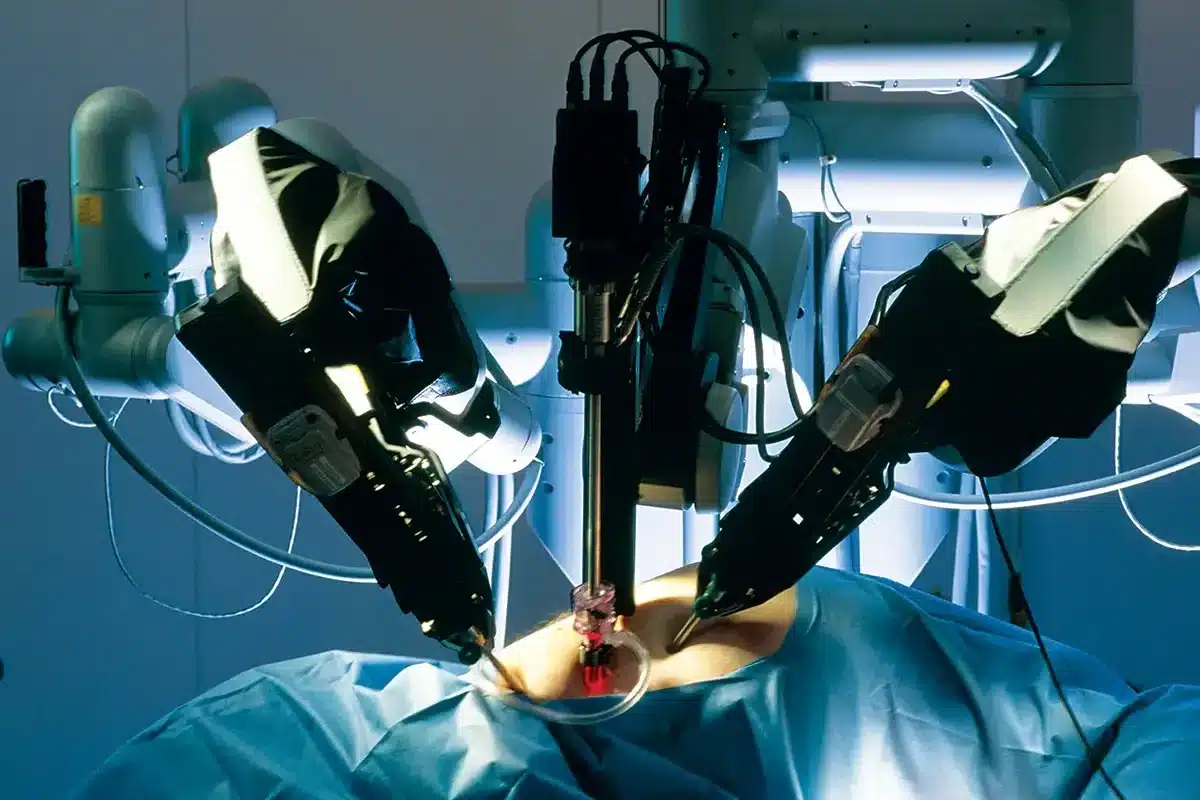
<SEP-14228_image_2>
Cardiac amyloidosis can be tricky to diagnose because it shares symptoms with other heart issues. It happens when amyloid proteins build up in the heart, causing it to work poorly. Getting the right diagnosis is key for the right treatment.
Restrictive Cardiomyopathy vs. Cardiac Amyloidosis
Restrictive cardiomyopathy and cardiac amyloidosis look similar because they both affect the heart’s ability to relax. But, cardiac amyloidosis is special because it involves amyloid proteins in the heart. Endomyocardial biopsy is the best way to tell them apart, even though new tests are being used too.
A study by the European Society of Cardiology found that cardiac amyloidosis is often missed or misdiagnosed.
Hypertensive Heart Disease Similarities
Hypertensive heart disease can look like cardiac amyloidosis because both can cause the heart to thicken and work poorly. But, hypertensive heart disease comes from high blood pressure, while cardiac amyloidosis is caused by amyloid proteins.
Differentiating Cardiac Amyloidosis from Other Heart Conditions
To tell cardiac amyloidosis apart from other heart problems, we need to look at many things. Cardiac MRI and echocardiography help see how the heart is doing. Tests like troponin and NT-proBNP also give clues about heart damage.
By knowing what makes cardiac amyloidosis unique and using the latest tests, we can get better at diagnosing it. This helps us give the right care to those with this complex condition.
Kidney Disorders Commonly Confused with Amyloidosis
Kidney involvement in amyloidosis can look like other kidney problems. This makes it hard to tell them apart. Amyloidosis shows symptoms that are similar to many kidney diseases.
Nephrotic Syndrome and Proteinuria
<SEP-14228_image_3>
Nephrotic syndrome is a common sign of amyloidosis. It shows up as a lot of protein in the urine, low albumin in the blood, and swelling. These signs can also point to other kidney diseases.
Seeing a lot of protein in the urine often leads doctors to think of nephrotic syndrome first. But, in amyloidosis, it’s because amyloid fibrils block the kidneys.
Chronic Kidney Disease Presentation
Amyloidosis can also look like chronic kidney disease (CKD). It shows signs like a low GFR, high blood pressure, and imbalanced electrolytes. Amyloidosis can slowly damage the kidneys, just like CKD does.
Glomerulonephritis and Amyloidosis Overlap
Glomerulonephritis, or inflammation of the glomeruli, can be confused with amyloidosis. Both can cause blood and protein in the urine. But, amyloidosis is caused by amyloid proteins, not inflammation.
|
Condition |
Key Features |
Differential Diagnostic Considerations |
|---|---|---|
|
Amyloidosis |
Amyloid fibril deposition, proteinuria, nephrotic syndrome |
Nephrotic syndrome, chronic kidney disease |
|
Nephrotic Syndrome |
Significant proteinuria, hypoalbuminemia, edema |
Amyloidosis, other glomerular diseases |
|
Chronic Kidney Disease |
Progressive decline in GFR, hypertension, electrolyte imbalances |
Amyloidosis, diabetic nephropathy, hypertensive nephrosclerosis |
It’s important to know the differences between amyloidosis and other kidney diseases. This helps doctors make the right diagnosis and treatment plan. A detailed diagnosis, including biopsies and scans, is often needed to tell them apart.
Neurological Conditions That Mimic Amyloidosis
Neurological symptoms of amyloidosis can look like other diseases, making it hard to diagnose. Amyloidosis causes nerve damage by depositing amyloid proteins. This leads to different types of neuropathies.
Peripheral Neuropathies and Sensory Disturbances
Peripheral neuropathy is a common symptom of amyloidosis. It causes numbness, tingling, and pain in the hands and feet. These symptoms can be confused with other neuropathies, like diabetic neuropathy.
Autonomic Nervous System Dysfunction
Amyloidosis can also harm the autonomic nervous system. This leads to symptoms like low blood pressure, stomach problems, and bladder issues. These symptoms can be similar to other conditions.
Diabetes-Related Neuropathy vs. Amyloid Neuropathy
Diabetes-related neuropathy and amyloid neuropathy share similar symptoms. But, they have different causes and treatments. A detailed evaluation, including a nerve biopsy, is needed for a correct diagnosis.
|
Characteristics |
Amyloid Neuropathy |
Diabetes-Related Neuropathy |
|---|---|---|
|
Primary Cause |
Amyloid protein deposition |
Chronic hyperglycemia |
|
Typical Symptoms |
Numbness, tingling, pain |
Numbness, tingling, pain, burning sensation |
|
Autonomic Involvement |
Common |
Common |
|
Diagnostic Clues |
Bone marrow biopsy, genetic testing |
Blood glucose levels, nerve conduction studies |
It’s important to know the differences between amyloid neuropathy and diabetes-related neuropathy. This helps in making the right diagnosis and treatment plan. When a patient has unclear neuropathy, amyloidosis should be considered.
Gastrointestinal Disorders Sharing Symptoms with Amyloidosis
Amyloidosis can make diagnosing digestive issues tricky because its symptoms are similar to other conditions. It affects the GI tract, causing symptoms like abdominal pain, diarrhea, and constipation. These are also seen in other digestive problems.
Irritable Bowel Syndrome and Chronic Digestive Issues
People with amyloidosis may have symptoms like abdominal pain, diarrhea, and constipation. These are also signs of irritable bowel syndrome (IBS). This similarity can lead to wrong diagnoses. Diagnostic tests such as endoscopy and biopsy help tell amyloidosis apart from IBS.
Inflammatory Bowel Disease Similarities
Amyloidosis can also look like inflammatory bowel disease (IBD). This includes Crohn’s disease and ulcerative colitis. Symptoms like weight loss, diarrhea, and abdominal pain are common in both. A thorough medical history and diagnostic testing are key to telling these conditions apart.
Malabsorption Syndromes and Weight Loss
Gastrointestinal amyloidosis can cause malabsorption, leading to weight loss and nutritional deficiencies. These symptoms can be confused with other conditions like celiac disease or pancreatic insufficiency. A detailed evaluation, including imaging studies and nutritional assessments, is needed for accurate diagnosis.
In conclusion, amyloidosis’ GI symptoms can be mistaken for other digestive disorders. This makes a detailed diagnostic process vital. By understanding the similarities and differences, doctors can improve diagnosis and treatment.
Multiple Myeloma: A Complex Relationship with Amyloidosis
Diagnosing amyloidosis is tricky because it’s linked to multiple myeloma, a plasma cell disorder. These two conditions share traits and lab findings. This makes it hard to tell them apart.
Overlapping Laboratory Findings
Both multiple myeloma and AL amyloidosis involve abnormal proteins. In multiple myeloma, there’s too much of a certain protein. AL amyloidosis causes amyloid to build up in tissues. Tests like SPEP and UPEP show these proteins, making diagnosis tough.
Coexistence of Multiple Myeloma and AL Amyloidosis
It’s common for multiple myeloma and AL amyloidosis to happen together. This is because they both come from abnormal plasma cells. Doctors need to look closely at both conditions to treat them right.
Key Distinguishing Features Between the Conditions
Even though they’re similar, multiple myeloma and AL amyloidosis have differences. Multiple myeloma causes bone damage, anemia, and high calcium levels. AL amyloidosis, on the other hand, affects organs like the heart and kidneys. Doctors use imaging and biopsies to figure out which one it is.
Rheumatological Diseases Mistaken for Amyloidosis
Amyloidosis symptoms can look like those of rheumatological diseases, leading to wrong diagnoses. Amyloidosis is a rare disease where amyloid proteins build up in the body’s tissues. This buildup causes symptoms that can be mistaken for rheumatological diseases, making it hard to diagnose.
Rheumatoid Arthritis and Inflammatory Markers
Rheumatoid arthritis (RA) is a chronic disease that mainly affects the joints. Both RA and amyloidosis can cause symptoms like fatigue, weight loss, and high inflammatory markers. The presence of markers like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) can be high in both, making diagnosis tricky.
|
Condition |
Common Symptoms |
Inflammatory Markers |
|---|---|---|
|
Rheumatoid Arthritis |
Joint pain, swelling, fatigue |
Elevated CRP, ESR |
|
Amyloidosis |
Organ dysfunction, fatigue, weight loss |
May have elevated CRP, ESR |
Connective Tissue Disorders with Similar Presentations
Conditions like systemic lupus erythematosus (SLE) and Sjögren’s syndrome can also show symptoms similar to amyloidosis. These include multi-organ involvement and various autoantibodies. A detailed diagnostic process is needed to tell them apart from amyloidosis.
Distinguishing Inflammatory Arthropathies from Amyloidosis
To correctly diagnose amyloidosis and tell it apart from rheumatological diseases, a thorough evaluation is key. This includes a detailed medical history, physical exam, lab tests (like Congo red staining), and genetic tests for hereditary amyloidosis.
Understanding the similarities and differences between amyloidosis and rheumatological diseases helps healthcare providers make accurate diagnoses. This ensures the right treatment is given.
Diagnostic Delays: Statistics and Impact on Patient Outcomes
Diagnostic delays in amyloidosis are a big problem. They affect how well patients do and how well treatments work. The symptoms of amyloidosis can look like other diseases, leading to wrong diagnoses and delays.
Average Time from Symptom Onset to Accurate Diagnosis
It can take over a year to correctly diagnose amyloidosis after symptoms start. This is because early symptoms are not clear and amyloidosis is rare. It’s hard for doctors to think of amyloidosis right away.
A study in a well-known medical journal found an average delay of 14 months for an accurate diagnosis. During this time, patients went through many tests and visits. This shows how hard it is to diagnose amyloidosis.
Consequences of Misdiagnosis on Disease Progression
Misdiagnosis and delayed diagnosis can have serious effects. They can make the disease worse and treatments less effective. These delays can cause:
- More damage to organs because amyloid is not treated
- The disease gets worse, making treatments less helpful
- Patients get treatments for the wrong conditions
As from a leading medical institution said, “Early diagnosis is key in amyloidosis. It helps prevent organ damage and improves patient results.”
Patient Experiences with the Diagnostic Journey
Patients with amyloidosis often face a tough and upsetting journey to get diagnosed. A survey showed many patients got wrong diagnoses before getting the right one.
|
Diagnostic Journey Aspect |
Patient Experience |
|---|---|
|
Number of Healthcare Visits |
Average of 5 visits before accurate diagnosis |
|
Time to Diagnosis |
Median delay of 14 months |
|
Misdiagnoses |
Multiple misdiagnoses common |
It’s important to understand how diagnostic delays affect patients. We need to work on making diagnosis better for amyloidosis. By raising awareness and pushing for early detection, we can help patients get better care sooner.
Advanced Diagnostic Techniques for Amyloidosis
Advanced diagnostic techniques are key in identifying amyloidosis. Diagnosing this complex condition needs a mix of methods.
Tissue Biopsies and Congo Red Staining
Tissue biopsies are vital in diagnosing amyloidosis. A tissue sample is taken, usually from fat, bone marrow, or an affected organ. It’s then stained with Congo red.
This staining shows amyloid fibrils under polarized light, looking like apple-green birefringence.
The biopsy site choice is important. For heart amyloidosis, an endomyocardial biopsy might be used. But, a fat pad aspiration biopsy is often the first choice.
Modern Imaging Methods for Amyloid Detection
Modern imaging has improved diagnosing and monitoring amyloidosis. Cardiac MRI is great for checking the heart. It shows both shape and function.
99mTc-PYP/DPD/HMDP scintigraphy is also useful, mainly for ATTR amyloidosis.
|
Imaging Technique |
Application in Amyloidosis |
|---|---|
|
Cardiac MRI |
Assesses cardiac morphology and function, useful in diagnosing cardiac amyloidosis. |
|
99mTc-PYP/DPD/HMDP Scintigraphy |
Specifically useful for diagnosing transthyretin (ATTR) amyloidosis. |
|
PET/CT with amyloid tracers |
Emerging technique for detecting amyloid deposits in various organs. |
Genetic Testing for Hereditary Amyloidosis Forms
Genetic testing is vital for hereditary amyloidosis. It finds specific mutations, like in the TTR gene for ATTRv amyloidosis. Genetic counseling is also key, helping patients understand their genetic status.
By using tissue biopsies, imaging, and genetic testing, we can diagnose amyloidosis more accurately. This leads to better treatment plans.
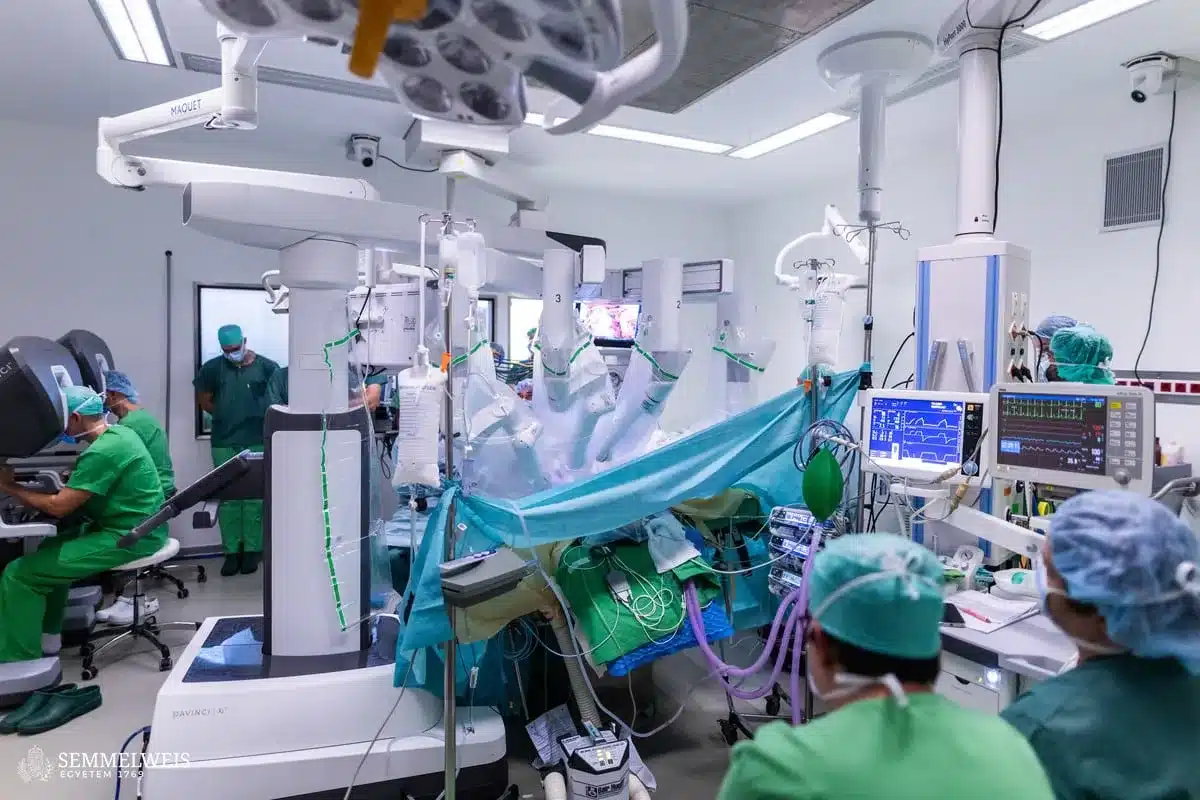
Multidisciplinary Approach to Accurate Diagnosis
Diagnosing amyloidosis needs a team effort. Many experts must work together. This teamwork is key to finding the right diagnosis for this complex disease.
The Role of Specialist Collaboration
Many specialists are needed to diagnose amyloidosis. This includes cardiologists, nephrologists, neurologists, and hematologists. Working together, they make sure no part of the disease is missed. This leads to a more accurate diagnosis.
|
Specialist |
Role in Diagnosis |
|---|---|
|
Cardiologist |
Checks the heart with echocardiography and other tests. |
|
Nephrologist |
Looks at kidney function and checks for proteinuria or kidney failure. |
|
Neurologist |
Looks for signs of neuropathy and checks neurological symptoms. |
|
Hematologist |
Looks for blood disorders, like multiple myeloma. |
Comprehensive Evaluation Protocols
Diagnosing amyloidosis needs a detailed plan. This includes a full medical history, physical exam, lab tests, and imaging. Advanced tests like genetic testing and tissue biopsies are also key. These help confirm the diagnosis.
Case Study: Successful Diagnostic Approaches
A 55-year-old patient had heart failure and kidney problems. Thanks to teamwork between cardiologists and nephrologists, along with detailed tests, they found AL amyloidosis. A bone marrow biopsy and cardiac MRI confirmed the diagnosis. This shows how important teamwork is in finding the right diagnosis.
When to Suspect Amyloidosis: Red Flags for Healthcare Providers
It’s vital to spot amyloidosis early. Certain signs should make healthcare providers look closer. Amyloidosis is tricky to diagnose because it shows up in many ways.
Key Symptom Combinations That Suggest Amyloidosis
Some symptoms together might point to amyloidosis. These include:
- Unexplained weight loss with fatigue
- Multi-organ problems without a clear reason
- Neuropathy or heart issues that don’t follow usual patterns
If patients show these signs, doctors should think about amyloidosis.
Risk Factors and Family History Considerations
Having a family history of amyloidosis or certain genes raises the risk. Also, conditions like multiple myeloma or chronic inflammation can lead to amyloidosis. Knowing these risk factors helps in catching it early.
Unexplained Multi-Organ Dysfunction
Amyloidosis often hits many organs at once. This creates a complex situation. If organs like the kidneys, heart, or gut don’t work right without a clear reason, doctors should think of amyloidosis. They should then do the right tests.
Conclusion: Improving Awareness and Timely Diagnosis of Amyloidosis
Amyloidosis is a complex and often misdiagnosed condition. Improving awareness and getting a timely diagnosis is key for better patient outcomes. We’ve talked about the different types of amyloidosis, their unique features, and the challenges in diagnosing this rare disease.
It’s vital to keep researching amyloidosis. This research helps us understand the disease better and find effective ways to diagnose and treat it. By raising awareness among healthcare providers and the public, we can cut down on diagnostic delays and improve care for patients.
Getting a diagnosis early is important in managing amyloidosis. It lets us start treatment sooner. We need to work together to create detailed evaluation plans and encourage specialists to collaborate. This ensures accurate diagnosis and effective management of this complex condition.
By boosting awareness and pushing forward with amyloidosis research, we can make big improvements in patient outcomes. We aim to provide top-notch healthcare to those dealing with this rare but serious condition.
FAQ
What is amyloidosis?
Amyloidosis is a rare condition where amyloid proteins build up in the body’s tissues. This buildup disrupts normal tissue function. It leads to various symptoms and health issues.
What are the different types of amyloidosis?
There are several types of amyloidosis. These include AL (primary) amyloidosis, AA (secondary) amyloidosis, hereditary amyloidosis, and wild-type ATTR amyloidosis. Each type has its own symptoms and treatment needs.
What are the symptoms of amyloidosis?
Symptoms of amyloidosis vary widely. They can include general symptoms like weight loss and fatigue. Specific symptoms depend on the organs affected, such as heart failure or kidney problems.
Why is amyloidosis often misdiagnosed?
Amyloidosis is often misdiagnosed. This is because its symptoms are not specific, it’s rare, and diagnostic tests have limitations. It’s hard for doctors to diagnose it quickly and accurately.
How is amyloidosis diagnosed?
Diagnosing amyloidosis requires advanced tests. These include tissue biopsies, modern imaging, and genetic testing for hereditary forms. These methods help identify the disease accurately.
What is the importance of a multidisciplinary approach in diagnosing amyloidosis?
A team approach is key for diagnosing amyloidosis. It involves specialists working together. This ensures a thorough evaluation and accurate diagnosis.
When should healthcare providers suspect amyloidosis?
Doctors should suspect amyloidosis in patients with specific symptoms and risk factors. They should also consider unexplained multi-organ dysfunction. This prompts further investigation.
What are the consequences of diagnostic delays in amyloidosis?
Delayed diagnosis in amyloidosis can worsen the disease. It affects patient outcomes and experiences. Improved awareness and timely diagnosis are essential.
How does amyloidosis affect different organs?
Amyloidosis can harm various organs. This includes the heart, kidneys, nervous system, and gastrointestinal tract. Each organ can show different symptoms and health issues.
What is the relationship between multiple myeloma and AL amyloidosis?
Multiple myeloma and AL amyloidosis are related but distinct. They share some laboratory findings. Accurate diagnosis requires careful evaluation.
How can amyloidosis be differentiated from other conditions?
Differentiating amyloidosis from other conditions requires understanding their similarities and differences. This includes conditions like restrictive cardiomyopathy and peripheral neuropathies. A thorough evaluation is necessary.
References
• PMC. Systemic AA amyloidosis: epidemiology, diagnosis, and management. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4218891/
• European Society of Cardiology (ESC). Cardiac amyloidosis: epidemiology, diagnosis and therapy. https://www.escardio.org/Journals/E-Journal-of-Cardiology-Practice/Volume-19/cardiac-amyloidosis-epidemiology-diagnosis-and-therapy
• NCBI Bookshelf. Amyloidosis. https://www.ncbi.nlm.nih.gov/books/NBK470285/ NCBI
• New England Journal of Medicine. [Title of article, NEJMra1806172]. https://www.nejm.org/doi/full/10.1056/NEJMra1806172
• Journal of Pediatric Hematology/Oncology (JPHO). Amyloidosis in Children: A Review of Clinical Features and Comparison with Adult Forms. https://journals.lww.com/jpho-online/Fulltext/2018/06000/Amyloidosis_in_Children__A_Review_of_Clinical.4.aspx