
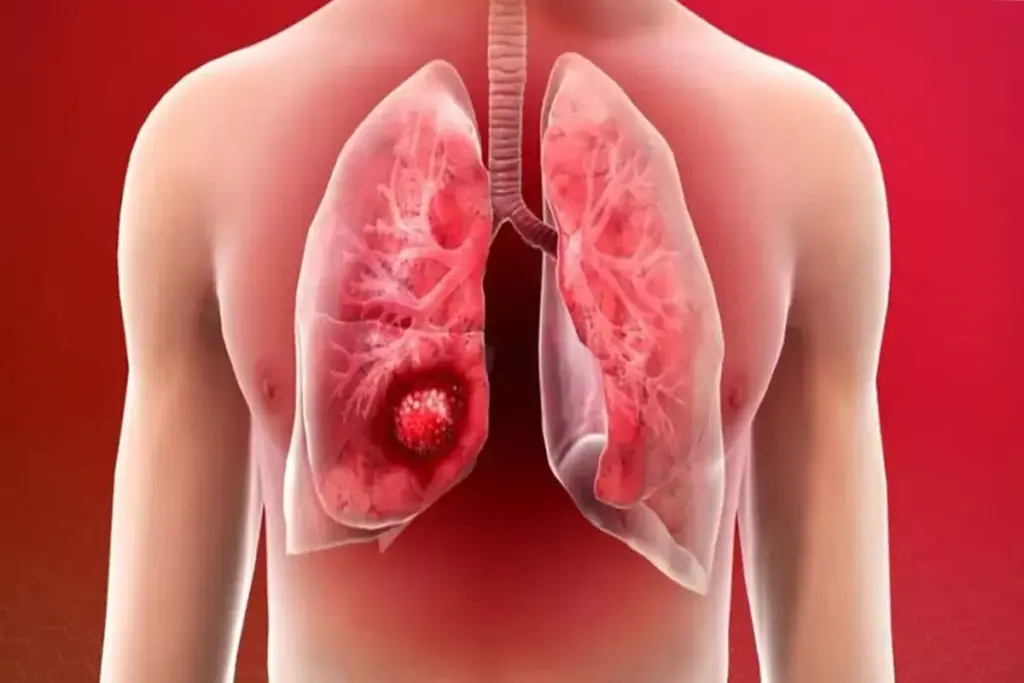
Lung cancer screening saves lives, mainly for those who have smoked a lot. Early detection is key. Annual scans with Low-Dose Computed Tomography (LDCT) can greatly improve chances of survival.
People with a big pack-year smoking history should think about starting screenings at 50. The United States Preventive Services Task Force (USPSTF) says to screen every year from 50 to 80 for those at high risk.
Spotting lung cancer early makes it easier to treat. This can lead to better survival rates and fewer complications. Screening is a powerful tool against lung cancer. Knowing when to start can help people protect their health.
Key Takeaways
- Lung cancer screening can save lives through early detection.
- Annual screenings using LDCT are recommended for those at high risk.
- The USPSTF recommends starting screening at age 50.
- Screening should continue until age 80 for those at high risk.
- A significant pack-year smoking history is a key risk factor for lung cancer.
- Early detection improves treatment outcomes and survival rates.
The Current Landscape of Lung Cancer Screening

Lung cancer is a major health issue worldwide, causing many deaths. It’s vital to know about lung cancer screening today.
Global Burden of Lung Cancer
Lung cancer is a top killer of cancer patients globally, with 1.8 million deaths each year. It’s often found too late, making treatment hard. The World Health Organization (WHO) says lung cancer causes nearly 1 in 5 cancer deaths worldwide.
|
Region |
Lung Cancer Incidence |
Lung Cancer Mortality |
|---|---|---|
|
Global |
2.2 million |
1.8 million |
|
North America |
234,000 |
185,000 |
|
Europe |
376,000 |
314,000 |
Importance of Early Detection
Finding lung cancer early is key to saving lives. Early detection means better treatment chances. Screening people at high risk, like long-term smokers, is important.
Common lung cancer symptoms include:
- persistent coughing
- chest pain or discomfort
- unexplained weight loss
- coughing up blood or rust-colored sputum
Knowing these symptoms and risk factors helps find and treat lung cancer early.
Understanding the USPSTF Screening Guidelines
The USPSTF guidelines help figure out who should get lung cancer screening. They look at age and how much someone has smoked. These rules help find people at high risk of lung cancer early.
Age 50 as the Starting Point
The USPSTF says lung cancer screening should start at age 50 for heavy smokers. This age is chosen because lung cancer risk goes up a lot after 50.
Starting screening at 50 helps find lung cancer early. This makes it easier to treat. It also helps lower death rates from lung cancer in those who get screened.
The 20 Pack-Year Smoking History Requirement
The USPSTF also looks at how much someone has smoked. A pack-year is how much someone has smoked over time. For example, smoking one pack a day for a year equals one pack-year.
To qualify, someone needs a smoking history of at least 20 pack-years. This means smoking one pack a day for 20 years or two packs a day for 10 years.
- A person smoking 1 pack/day for 20 years has 20 pack-years.
- A person smoking 2 packs/day for 10 years has 20 pack-years.
Knowing about pack-years is key to figuring out who should get screened for lung cancer. It helps follow the USPSTF guidelines.
American Cancer Society’s Updated Recommendations
The American Cancer Society has updated its lung cancer screening guidelines. These changes reflect new evidence and patient needs. They are important for both healthcare providers and patients, as they affect who should be screened and when.
Key Changes in 2023 Guidelines
The 2023 guidelines bring several key changes to improve lung cancer early detection. One major update is the expanded eligibility for screening. Now, more people can get screened based on the latest research and data.
These guidelines also stress the need for a personalized approach to screening. Age, smoking history, and health status are key factors in determining the best screening schedule for each person.
Elimination of the 15-Year Quit Time Requirement
A significant change in the 2023 guidelines is dropping the 15-year quit time rule for former smokers. Before, only those who had quit within 15 years were considered for screening. Now, more former smokers can get screened, even if they’ve quit longer ago.
This change shows our commitment to using evidence-based practices. It also recognizes that many former smokers are at risk of lung cancer, even after 15 years.
|
Guideline Component |
Previous Recommendation |
2023 Updated Recommendation |
|---|---|---|
|
Age to Start Screening |
50-74 years |
50-80 years |
|
Smoking History Requirement |
20 pack-years |
20 pack-years |
|
Quit Time for Former Smokers |
Within 15 years |
No quit time limit |
These updates show the American Cancer Society’s commitment to fighting lung cancer. By making screening more accessible and personalized, we aim to save more lives and improve outcomes for patients.
What Year Is It in Lung Cancer Screening Evolution?
Lung cancer screening has made big strides, with 2023 being a key year. It’s important to know how screening has changed over time. This helps us understand how to detect and treat lung cancer better.
Historical Development of Screening Protocols
The idea of lung cancer screening started decades ago. But, it wasn’t until the early 2000s that real progress was made. The National Lung Screening Trial (NLST) in the U.S. showed that low-dose CT scans can save lives. This study was a big step forward.
After the NLST, groups like the U.S. Preventive Services Task Force (USPSTF) and the American Cancer Society (ACS) updated guidelines. They looked at new evidence and how to better screen people. This includes figuring out the best age to start screening and using risk tools.
Current Year’s Standards Compared to Previous Decades
In 2023, lung cancer screening rules changed a lot. The ACS’s 2023 guidelines now let more people get screened. They lowered the age to start and dropped the need for a 15-year break from smoking for former smokers. These updates show we now understand lung cancer risk better.
Looking back, we see a move towards more tailored screening. Now, we use risk assessment tools and look at more than just smoking history. As we learn more about lung cancer, we’ll keep making these guidelines better to catch cancer early and help patients more.
Low-Dose Computed Tomography (LDCT): The Gold Standard
For those at high risk of lung cancer, LDCT screening is top choice. It spots cancer early and can save lives. Knowing how LDCT works and its benefits is key.
How LDCT Technology Works
LDCT scans are a special kind of CT scan. They use less radiation but keep image quality high. This is thanks to new scanner tech and smart image making.
The USPSTF says LDCT is best for lung cancer screening. It finds cancer early, when it’s easier to treat.
“LDCT for lung cancer screening cuts down on deaths,” it finds cancer early. This shows how important LDCT is for better patient care.
Radiation Exposure Considerations
LDCT scans do involve some radiation. But the dose is much lower than regular CT scans. It’s about 1.4 millisieverts (mSv), similar to yearly background radiation in the US.
But, the benefits of catching cancer early are big. A study found the risks from LDCT are small. For those at high risk, the benefits are clear.
Understanding LDCT and its radiation risks helps us see its value. We aim to guide on using LDCT for early detection and treatment.
Screening Guidelines for Current Smokers
The latest guidelines for lung cancer screening in current smokers highlight the need for annual assessments. As a current smoker, understanding these guidelines is key to potentially improving your lung cancer outcomes. We recommend that current smokers undergo regular screenings to facilitate early detection.
Annual Screening Recommendations
Current smokers are advised to undergo annual lung cancer screenings using Low-Dose Computed Tomography (LDCT). This recommendation is based on the significant benefits of early detection in improving survival rates. Annual screening helps in identifying lung cancer at an early stage when it is more treatable.
Additional Risk Factors to Consider
Besides smoking, there are other risk factors that may influence the need for lung cancer screening. These include exposure to carcinogens like asbestos, radon, and certain chemicals. Family history of lung cancer is another significant risk factor. We consider these factors when assessing an individual’s risk profile.
A detailed risk assessment helps in tailoring the screening approach. For instance, individuals with a history of smoking and exposure to asbestos may require more frequent screenings.
|
Risk Factor |
Description |
Screening Recommendation |
|---|---|---|
|
Current Smoker |
Individuals currently smoking |
Annual LDCT screening |
|
Exposure to Carcinogens |
Exposure to asbestos, radon, etc. |
Consider more frequent screenings |
|
Family History |
Family history of lung cancer |
Discuss with healthcare provider |
“Early detection of lung cancer through screening can significantly improve treatment outcomes. Current smokers should be aware of the guidelines and discuss their individual risk factors with their healthcare provider.”
— Expert in Pulmonology
Former Smokers: When and How Long to Screen
Lung cancer screening guidelines for former smokers have changed. Now, we know better when and how long to screen. These updates aim to find the right balance between benefits and risks.
Previous Guidelines and the 15-Year Quit Timeframe
Old guidelines said former smokers who quit in the last 15 years should get screened. This was because quitting didn’t immediately stop the risk of lung cancer.
The 15-year rule was key in deciding who should get screened. But, as more research came in, these guidelines have changed.
Current Screening Recommendations
Now, former smokers are judged on their own risk factors. This includes how long they’ve been smoke-free and their smoking history. The goal is to make screening more personal.
We look at more than just how long ago someone quit smoking. Other factors, like age and health history, also play a role in deciding if someone should get screened.
- The age at which screening starts and stops.
- The smoking history and quit time.
- Other risk factors that may influence screening decisions.
“The evolution of lung cancer screening guidelines reflects our growing understanding of the disease and our commitment to providing the best possible care for our patients.”
— Expert in Pulmonology
Why Screening Continues Until Age 80
There’s a good reason we keep screening for lung cancer until age 80. Studies show that about half of lung cancers are found in people 75 or older. This makes it clear that screening is key in this age group.
Incidence Rates in People 75 and Older
Lung cancer is a big concern for older adults. Research shows that the risk of lung cancer stays high for those 75 and older. A lot of lung cancer cases are found in this age group, showing the need for ongoing screening.
As we get older, the risk of lung cancer doesn’t go down. The buildup of risk factors like smoking history makes older people more likely to get lung cancer. Recent studies suggest that adults up to 80 who can have surgery might also benefit from screening. This supports extending screening guidelines to this age.
Fitness for Surgery Considerations
Whether someone should keep getting screened until 80 depends on their health for surgery. Those who can have surgery are more likely to benefit from early detection. This is a big part of deciding for older adults.
Doctors look at a patient’s overall health and any health problems they have. They check if someone is healthy enough for surgery. This helps make sure the benefits of screening outweigh the risks.
By screening until 80 for those who can have surgery, we might help more older adults with lung cancer. This approach helps give personalized care to people of all ages.
Common Lung Cancer Symptoms to Be Aware Of
Knowing the signs of lung cancer can help a lot. It often doesn’t show symptoms early on. So, it’s key for people at risk to get checked regularly.
Early Warning Signs
Look out for a cough that won’t go away, chest pain, and trouble breathing. These signs might seem small but are important. They could mean something serious if they keep happening or get worse.
Other early signs include:
- Coughing up blood or rust-colored sputum
- Shortness of breath or wheezing
- Recurring respiratory infections like bronchitis or pneumonia
- Loss of appetite or weight loss
- Fatigue or feeling weak
When Symptoms Warrant Immediate Attention
These symptoms might point to lung cancer, but they can also mean other things. But, if you have severe trouble breathing, chest pain, or cough up blood, get help right away.
“If you’re experiencing severe difficulty breathing, chest pain, or coughing up blood, don’t hesitate to seek emergency care.”
If you have lung cancer or are at high risk, stay close to your doctor. They can help watch your symptoms and change your treatment if needed.
Knowing the symptoms of lung cancer and when to get help is very important. Early detection and treatment can greatly improve care.
Risk-Benefit Analysis of Age-Based Screening
When thinking about the best age for lung cancer screening, we must look at both sides. We need to see how early detection helps and the risks of screening. This balance is key to making a good choice.
Potential Benefits of Early Detection
Screening for lung cancer early can greatly improve treatment results. Early detection means better treatment options and higher survival rates. The main benefits of age-based screening are:
- Lower death rates from catching cancer early
- Better chances of successful surgeries
- Less invasive treatment options
Studies show lung cancer screening has cut death rates in screened groups. Finding the right age for starting screening is vital to get these benefits.
Possible Harms and Considerations
Screening for lung cancer has big benefits, but there are downsides too. These include:
- Exposure to radiation from frequent scans
- False positives causing worry and more tests
- Overdiagnosis, where screening finds cancers that won’t harm
It’s important to weigh these risks against the benefits to keep screening safe and effective. Choosing the right age for screening helps balance risks and benefits for those at high risk of lung cancer.
In summary, the decision on age for lung cancer screening is complex. Knowing the benefits and risks helps us make smart choices. This way, we can improve outcomes and reduce risks.
Special Considerations for High-Risk Populations
Lung cancer screening needs special care for some groups. A single screening plan doesn’t work for everyone. This is true for those with extra risks, like age and smoking.
Risk Factors Beyond Age and Smoking
Many things can raise lung cancer risk. These include family history, exposure to harmful substances like asbestos or radon, and past lung diseases. For example, people with lung cancer in their family might need screening sooner. We also look at genetic mutations and environmental exposures to decide on the right screening plan.
Customized Screening Approaches
For those at high risk, we use special screening plans. This might mean starting screening earlier or doing it more often. We might also use new tools, like advanced imaging, to find cancer sooner. Tailoring screening to each person’s risk helps make lung cancer screening more effective.
- Find people at higher risk due to genetics, environment, or other factors.
- Make screening plans that fit each person’s risk.
- Use new technologies to find and diagnose cancer better.
By making lung cancer screening more personal, we can help those at high risk. This could lead to better health outcomes.
Insurance Coverage and Accessibility
Many people start their lung cancer screening journey by checking their insurance. It’s important to know what healthcare options are out there for those at risk of lung cancer.
Insurance plans for lung cancer screening differ, but many cover Low-Dose Computed Tomography (LDCT) scans. Understanding your insurance policy is key to getting this life-saving screening.
Medicare and Medicaid Coverage
Medicare and Medicaid are big in helping people get lung cancer screening. Medicare covers LDCT scans for those aged 50 to 77 who smoke or have quit recently. Medicaid’s coverage varies by state, but many states include lung cancer screening in their plans.
The Centers for Medicare & Medicaid Services say Medicare covers lung cancer screening with LDCT for those who meet the criteria. This makes lung cancer screening more accessible.
Private Insurance Policies
Private insurance also covers lung cancer screening, but details vary. This means annual LDCT scans for adults aged 50 to 80 with a 20 pack-year smoking history and who smoke or have quit recently.
It’s vital to review your private insurance policy to know what’s covered and the requirements for lung cancer screening. Policy details can vary significantly, so it’s best to check with your insurance provider.
In summary, there are many insurance options for lung cancer screening. But, knowing the details of your policy is essential to get this important health service. We suggest talking to your healthcare provider and insurance company to find the best option for you.
International Standards and Best Practices
Looking into lung cancer screening standards around the world shows a variety of methods. Each country uses its own guidelines based on local health data and risk levels. This is influenced by the healthcare system in each place.
European Guidelines Comparison
The European Union has set guidelines for lung cancer screening. These rules are followed by member states, but with some differences. For example, the European Society of Radiology and the European Respiratory Society recommend using low-dose CT scans for those at high risk.
When comparing European guidelines to those in the United States, we see both similarities and differences. Both agree on screening high-risk groups. But, the criteria for who is considered high-risk and how often to screen can differ.
Global Variations in Screening Ages
How old you need to be to start screening for lung cancer varies worldwide. Some countries start screening later, while others have stricter rules about smoking history. For example:
|
Country/Region |
Starting Age |
Smoking History Requirement |
Screening Interval |
|---|---|---|---|
|
United States |
50 |
20 pack-years |
Annual |
|
European Union |
55-74 |
30-40 pack-years |
Biennial or Annual |
|
Canada |
55-74 |
30 pack-years |
Annual |
|
Australia |
55-74 |
High-risk assessment |
Biennial |
This table shows how different regions have different guidelines for lung cancer screening. It points out the need for personalized care based on local health data and risk factors.
It’s important for healthcare providers to understand these differences. This helps them give the right advice and screening options to patients, whether they travel or live in different countries.
Liv Hospital’s Multidisciplinary Approach
At Liv Hospital, we lead in lung cancer diagnosis with our advanced strategy. We bring together many medical fields for complete care for our patients.
Our team includes experts in pulmonology, oncology, thoracic surgery, and radiology. They work together to create a treatment plan that fits each patient. This teamwork is key in fighting lung cancer, where quick detection and precise treatment are vital.
State-of-the-Art Screening Technology
We use Low-Dose Computed Tomography (LDCT) for screening. LDCT can spot lung cancer early, when it’s easier to treat. Our top-notch technology gives patients accurate diagnoses with less radiation.
- High-resolution imaging for precise diagnosis
- Advanced software for image analysis
- Minimal radiation exposure
Integrated Care Pathways
Our care paths make the patient journey smoother, from screening to follow-up. This way, patients get care that’s easy to follow, lessening the stress of cancer treatment.
Our commitment to integrated care means we listen to patients and their families. We tailor our services to meet their unique needs.
- Personalized care plans
- Multidisciplinary team meetings to discuss patient cases
- Support services for patients and their families
By using the latest technology and focusing on patients, Liv Hospital aims to better lung cancer outcomes. Our team is dedicated to top-notch care, backed by the latest medical science.
Conclusion: Making Informed Decisions About Lung Cancer Screening
Understanding lung cancer screening is key to our health. Knowing the guidelines helps us detect and treat lung cancer early. This is a proactive step towards better health.
Lung cancer screening has changed a lot. The United States Preventive Services Task Force (USPSTF) and the American Cancer Society have updated their advice. Low-dose computed tomography (LDCT) is now the top choice for screening. It helps find lung cancer early.
Today, guidelines say smokers and former smokers should get screened. Annual scans are suggested until you’re 80. Knowing the risks and benefits helps us make smart health choices. We can work with our doctors to create a screening plan that’s right for us.
It’s important to keep up with new information on lung cancer screening. By staying informed, we can manage our health better. This way, we make choices that fit our needs and risks, as of today.
FAQ
At what age should I start lung cancer screening?
The USPSTF says start at 50 if you’ve smoked for 20 years.
What is considered a 20 pack-year smoking history?
It means smoking one pack a day for 20 years or two packs a day for 10 years.
Are there any changes in the American Cancer Society’s guidelines for lung cancer screening?
Yes, they’ve updated their guidelines. Now, they focus on individual risk, not just quitting time.
How does Low-Dose Computed Tomography (LDCT) work for lung cancer screening?
LDCT uses low radiation to make detailed lung images. This helps find lung cancer early.
What are the common symptoms of lung cancer that I should be aware of?
Look out for coughing, chest pain, coughing up blood, and shortness of breath. If you notice these, see a doctor right away.
How long should I continue lung cancer screening?
Keep screening until you’re 80. This is because lung cancer is common in older adults.
Are there any special considerations for high-risk populations?
Yes, people with smoking history, exposure to harmful substances, or family lung cancer history may need special screening plans.
Is lung cancer screening covered by insurance?
Yes, many insurances, including Medicare and Medicaid, cover it. But, coverage can change based on your policy and situation.
How does Liv Hospital approach lung cancer screening and treatment?
Liv Hospital uses advanced technology and a team approach for complete care.
What are the benefits and harms of age-based lung cancer screening?
It can find cancer early and improve treatment chances. But, it might also lead to false positives, overdiagnosis, and radiation risks.
How do international guidelines compare for lung cancer screening?
Guidelines vary worldwide. But, they all stress the need for early detection and risk-based screening.
What is the current year and how has it impacted lung cancer screening guidelines?
As of now, guidelines keep getting updated. They reflect new research and screening tech advancements.
How many cigarettes are in a pack, and how is this used to calculate pack-year history?
A pack has 20 cigarettes. To calculate pack-years, multiply packs smoked daily by years smoked.
References
Binaytara Foundation. Understanding the lung cancer screening guidelines. https://binaytara.org/cancernews/article/understanding-the-lung-cancer-screening-guidelines
U.S. Preventive Services Task Force (USPSTF). Lung cancer screening — final recommendation statement. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening
ASCOpost. Lung cancer screening may benefit adults up to age 80 who are fit for surgery. https://ascopost.com/news/september-2025/lung-cancer-screening-may-benefit-adults-up-to-age-80-who-are-fit-for-surgery/
Office of Disease Prevention and Health Promotion. Lung cancer screening. https://odphp.health.gov/healthypeople/tools-action/browse-evidence-based-resources/lung-cancer-screening
JAMA Network Open. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2830087





