Colonoscopy is key for catching colorectal disease early. But, it’s not for everyone. At Liv Hospital, we focus on the risks and when it’s not safe. This is to keep our patients safe.
When should you get a colonoscopy? Learn amazing facts about scary risks and find powerful, vital ways to schedule your essential screening.
Specific health risks can make a colonoscopy risky. These include recent heart attacks, severe blood pressure issues, peritonitis, and recent colon surgery. People with these issues might face more dangers during or after the test.
Key Takeaways
- Colonoscopy is not recommended for patients with recent myocardial infarction or severe hemodynamic instability.
- Conditions like peritonitis and recent colon surgery are contraindications for colonoscopy.
- Patient safety is our top priority, and knowing the risks is key before a colonoscopy.
- Liv Hospital puts patient safety first in all medical procedures.
- Certain patients might need other screening methods because of health risks or contraindications.
Understanding Colonoscopy: Purpose and Procedure

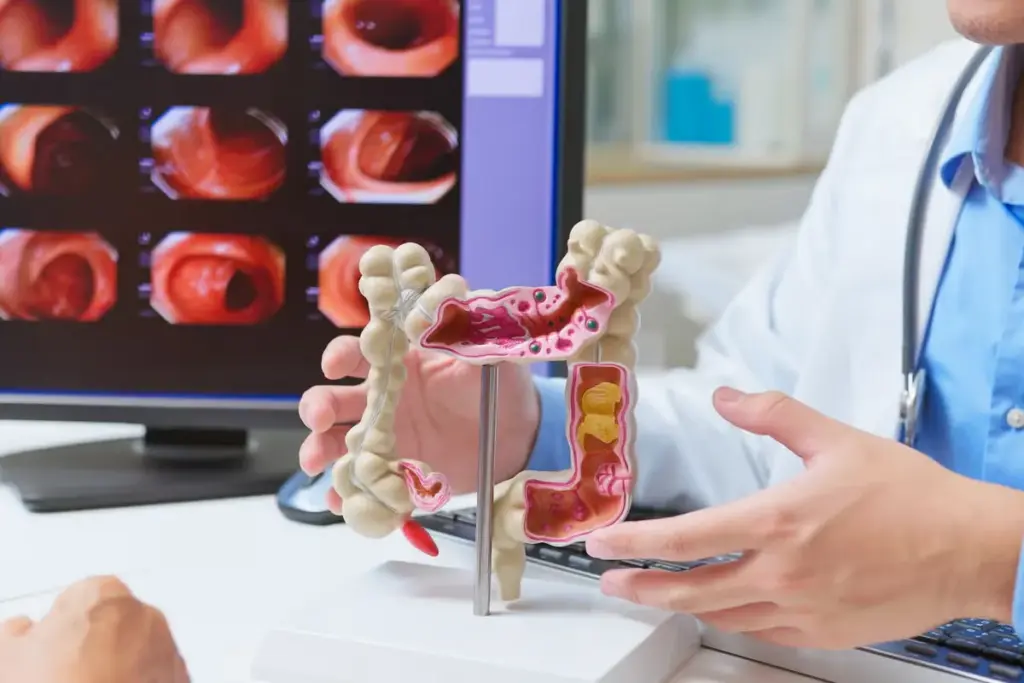
A colonoscopy lets doctors see inside the colon. It’s key for finding and stopping colorectal cancer. It also helps diagnose other gut problems.
What Is a Colonoscopy?
A colonoscopy uses a flexible tube with a camera and light. This tube, called a colonoscope, looks at the colon and rectum’s lining. Doctors can spot things like polyps, ulcers, or cancerous growths.
The colonoscope has tools for taking tissue samples or removing polyps. This helps stop colorectal cancer.
Standard Colonoscopy Procedure
The usual colonoscopy steps are:
- Preparation: Patients clean their bowel before the test.
- Sedation: The test is done under sedation to reduce pain.
- Insertion of the Colonoscope: The colonoscope goes in through the rectum and moves through the colon.
- Inspection: The doctor checks the colon and rectum for any issues.
- Biopsy or Polyp Removal: Tissue samples are taken or polyps are removed if needed.
Diagnostic and Preventive Benefits
Colonoscopy has big benefits. It finds colorectal cancer early, which helps with treatment. It also removes polyps to stop cancer before it starts.
Katie Couric emphasizes that regular screenings are essential for early detection of colon cancer. Colonoscopies help find problems before symptoms show up. This keeps the gut healthy.
|
Benefits |
Description |
|---|---|
|
Early Detection |
Finds colorectal cancer early, improving treatment chances. |
|
Polyp Removal |
Removes polyps that could turn into cancer, stopping it. |
|
Diagnostic Accuracy |
Gives a clear look at the colon and rectum, helping with accurate diagnosis. |
Absolute Contraindications for Colonoscopy
Some health issues make colonoscopy too risky. It’s key to know when to avoid it. Colonoscopy is a valuable tool but comes with risks. Knowing when to skip it is vital for safety.
Recent Myocardial Infarction
A recent heart attack is a big no for colonoscopy. The test’s stress and possible complications can lead to another heart issue. Doctors usually wait a while after a heart attack before doing a colonoscopy. This wait time depends on the patient’s risk and the heart attack’s severity.
Severe Hemodynamic Instability
Those with unstable blood pressure or serious circulatory problems shouldn’t get a colonoscopy. The sedation needed for the test can make things worse, leading to serious issues.
Peritonitis and Abdominal Emergencies
Peritonitis and other sudden abdominal problems are big no-gos for colonoscopy. These issues need quick medical help. A colonoscopy could make things worse or complicate treatment.
Recent Colon Surgery or Repair
Colonoscopy is not recommended after recent colon surgery or repair. It could mess with the healing, leading to problems like leaks or holes.
Here’s a quick rundown of when to avoid colonoscopy:
|
Condition |
Description |
Rationale for Contraindication |
|---|---|---|
|
Recent Myocardial Infarction |
A heart attack occurring recently |
Increased risk of another cardiac event due to procedural stress |
|
Severe Hemodynamic Instability |
Unstable blood pressure or critical circulatory issues |
Sedation and procedural stress can worsen hemodynamic instability |
|
Peritonitis and Abdominal Emergencies |
Inflammation of the peritoneum or acute abdominal conditions |
Colonoscopy could exacerbate the condition or complicate diagnosis and treatment |
|
Recent Colon Surgery or Repair |
Surgery or repair performed on the colon recently |
Risk of interfering with the healing process, potentially causing complications |
It’s important for doctors to weigh the risks and benefits of colonoscopy for each patient. This ensures the test is done safely and effectively.
When Should You Get a Colonoscopy? Standard Guidelines
Deciding when to have a colonoscopy depends on several things. These include your age, family history, and any symptoms you might have. Knowing these guidelines can help you make smart choices about your health.
Age-Based Recommendations
Experts say to start colonoscopy screenings at 45 for those at average risk of colorectal cancer. This age was picked because more young people are getting this cancer.
If you have a higher risk because of family history or other factors, you might need to start screenings earlier. We’ll look at these factors in more detail below.
Family History Considerations
A family history of colorectal cancer or certain genetic syndromes raises your risk. If a first-degree relative (like a parent, sibling, or child) has colorectal cancer, you might need to start screenings early.
- If a first-degree relative was diagnosed at 60 or older, start screenings at 45.
- If a first-degree relative was diagnosed between 45-59, start screenings 10 years before their diagnosis.
- If there are multiple first-degree relatives diagnosed or a known genetic syndrome, talk to a healthcare provider for advice.
Symptom-Based Indications
Certain symptoms can lead a healthcare provider to suggest a colonoscopy, no matter your age. These symptoms include:
- Persistent changes in bowel habits
- Rectal bleeding or blood in the stool
- Abdominal pain or cramping
- Unexplained weight loss
If you’re experiencing any of these symptoms, talk to your healthcare provider. They might suggest a colonoscopy or other tests.
Understanding these guidelines helps both you and your healthcare provider decide when to have a colonoscopy. It’s about finding the right balance between early detection and the risks of the procedure.
High-Risk Conditions That May Prevent Colonoscopy
Colonoscopy is a key tool for checking the health of the colon. But, some conditions make it too risky. We need to think carefully about each patient’s situation before deciding on colonoscopy.
Active Bowel Inflammation
Conditions like ulcerative colitis or Crohn’s disease can make colonoscopy risky. The inflamed bowel is more likely to tear during the procedure. We usually wait until the inflammation goes down before doing a colonoscopy.
Fulminant Colitis
Fulminant colitis is a serious form of colitis. It causes widespread inflammation and can be dangerous. Because of the high risk of tearing and the patient’s poor health, we often choose other tests instead.
Toxic Megacolon
Toxic megacolon is a serious condition that can happen with severe colitis. It makes the colon very big and can tear, leading to serious problems. Because of this, colonoscopy is usually not done in cases of toxic megacolon.
Severe Crohn’s Disease Flares
Severe Crohn’s disease can make colonoscopy difficult. The inflamed tissues are more likely to get hurt, and strictures or fistulas can make things worse. In these cases, we might look for other ways to diagnose the problem.
The following table summarizes the high-risk conditions and their implications for colonoscopy:
|
Condition |
Risks Associated with Colonoscopy |
Alternative Approaches |
|---|---|---|
|
Active Bowel Inflammation |
Increased risk of perforation, exacerbation of inflammation |
Delay colonoscopy until inflammation is controlled |
|
Fulminant Colitis |
High risk of perforation, worsening of systemic toxicity |
Use alternative diagnostic methods |
|
Toxic Megacolon |
High risk of perforation, life-threatening complications |
Avoid colonoscopy, consider emergency surgery if necessary |
|
Severe Crohn’s Disease Flares |
Increased risk of tissue injury, complications from strictures or fistulas |
Consider alternative diagnostic strategies during flares |
It’s important to know about these high-risk conditions. This helps us decide if colonoscopy is safe for each patient. We must balance the benefits against the risks and look for other ways to diagnose when needed.
Are Colonoscopies Safe? Understanding the Risks
Colonoscopies are usually safe, but there are risks to know before you get one. It’s important to understand these risks to make a good choice.
Perforation Risk
One big risk is a hole in the colon. This is rare, happening in 0.1% to 0.3% of cases. But, it can cause serious problems like infection and need for emergency surgery.
Risk factors for perforation include:
- Diverticulosis
- Previous abdominal surgery
- Colonic strictures or tumors
Bleeding Complications
Bleeding is another risk of colonoscopy. It can happen during or after the test. The chance of bleeding goes up with certain actions, like removing polyps.
Factors that increase the risk of bleeding include:
- Anticoagulant or antiplatelet therapy
- Large or numerous polyps
- Certain patient comorbidities
Adverse Reactions to Sedation
Many get sedation to relax during the test. Sedation is usually safe but can cause problems. These can range from mild breathing issues to serious allergic reactions.
Monitoring during the procedure is key to avoid these risks.
Post-Procedure Complications
After the test, you might feel pain, bloating, or other issues. Sometimes, you might face more serious problems like post-polypectomy syndrome.
Watch for signs of complications and get help if you notice:
- Severe abdominal pain
- Rectal bleeding
- Fever or chills
Is a Colonoscopy Considered a Surgical Procedure?
It’s important for patients to know if colonoscopy is a surgical procedure. Many people are unsure about this common test.
Invasive vs. Surgical Classification
Colonoscopy is not seen as a surgical procedure, even though it’s invasive. A flexible tube with a camera is used to see inside the colon. This is key because it affects how patients see the risks and recovery.
Key differences between colonoscopy and surgery include:
- No surgical incisions are made.
- The procedure is typically performed under sedation, not general anesthesia.
- Recovery times are generally shorter compared to surgical operations.
Anesthesia Considerations
Even though it’s not surgery, colonoscopy often uses sedation for comfort. The sedation level can vary, depending on the patient and the doctor.
Key considerations for anesthesia in colonoscopy include:
- Monitoring of vital signs during the procedure.
- Presence of an anesthesia professional or trained nurse.
- Adjusting sedation levels based on patient response.
Recovery Requirements
Recovery from colonoscopy is less intense than from surgery. But, patients should have someone to drive them home and avoid heavy tasks for a while.
Recovery guidelines typically include:
- Resting for the remainder of the day.
- Avoiding strenuous activities.
- Following specific dietary instructions provided by the healthcare provider.
Knowing that colonoscopy is not surgery but needs care and caution helps patients prepare better. This makes the experience and recovery easier to handle.
Colonoscopy Dangers: Mortality Rates and Serious Complications
It’s important for patients and doctors to know about colonoscopy dangers. This test helps find and prevent colorectal cancer. But, knowing the risks is key.
Overall Mortality Statistics
The death rate from colonoscopy is very low. Research shows it’s under 1 death per 100,000 tests. Yet, this number can change based on the patient’s health and the doctor’s skill.
Key statistics on colonoscopy mortality include:
- Mortality rate: Less than 1 per 100,000 procedures
- Major complication rate: Approximately 2.8 per 1,000 procedures
- Risk of death: Higher in patients with significant comorbidities
Risk Factors for Adverse Outcomes
Some things can make colonoscopy risks higher. These include:
- Advanced age
- Presence of comorbid conditions such as heart disease or diabetes
- History of previous colon surgery or repair
- Use of certain medications that may increase the risk of bleeding
Talking to your doctor about these risks is important. This helps understand your personal risk.
Comparing Risks to Benefits
When thinking about colonoscopy, weighing risks and benefits is key. For many, the benefits of finding and removing polyps are worth the risks. But, for those with serious health issues, the risks might be too high.
We must carefully assess the risk-benefit ratio for each patient. This means looking at their health, medical history, and what the test can offer.
Knowing about colonoscopy dangers helps patients and doctors make better choices. This is about deciding if the test is right for each person.
Patients with Severe Comorbidities: Special Considerations
When someone has severe health issues, deciding on a colonoscopy gets tricky. It’s all about finding the right balance. Each case is unique, needing a careful look at the pros and cons of the test.
Cardiovascular Disease
Heart problems make colonoscopy riskier. We look at the heart’s health, past heart attacks, and if there’s heart failure. Sometimes, a heart expert is needed before the test to make sure the heart is ready.
For heart patients, we focus on:
- Checking how serious the heart disease is
- Adjusting heart medicines before the test
- Watching the heart closely during and after the test
Respiratory Conditions
Those with serious lung issues, like COPD, need extra care before a colonoscopy. Sedation can make breathing harder, so we watch them closely.
|
Respiratory Condition |
Precautions |
|---|---|
|
COPD |
Do lung function tests before, manage sedation carefully |
|
Asthma |
Make sure asthma is well-controlled, avoid things that can trigger it |
Diabetes and Metabolic Disorders
Diabetes and other metabolic problems can affect colonoscopy safety and success. We must keep blood sugar levels stable before, during, and after the test to avoid problems.
Diabetic patients should:
- Change their medicines before the test
- Keep a close eye on blood sugar
- Plan for diet and medicine changes after the test
Immunocompromised Patients
People with weakened immune systems, like those with HIV/AIDS or on immunosuppressants, face higher risks with colonoscopy. We must think hard about the benefits and risks, like infections and bleeding.
Immunocompromised patients need:
- Antibiotics before the test in some cases
- Watch for signs of infection
- Adjust immunosuppressants as needed
Frailty and Advanced Age: When to Stop Having Colonoscopies
For older adults and those with serious health issues, the question of when to stop colonoscopies is key. As people get older, their health, life expectancy, and other health problems are important. These factors help decide if the benefits of colonoscopy screenings outweigh the risks.
Upper Age Limits in Guidelines
Medical guidelines suggest stopping colonoscopy screenings at certain ages. For example, for those at low risk, screenings might stop at 75. This is because life expectancy is shorter, and the benefits of screening lessen.
Life expectancy is a big factor. If someone’s life expectancy is less than 10 years, they might not get much benefit from screenings.
Frailty Assessment
Frailty is a condition where people are more vulnerable to stress and have less physical strength. Doctors use frailty assessments to see who might face more risks from colonoscopies.
- Tools like the Fried Frailty Index help doctors check a patient’s physical health.
- Those found to be frail might get alternative screening options or stop routine colonoscopies.
Life Expectancy Considerations
Knowing how long someone might live is important for making decisions. Tools like the Schonberg Index help predict how likely someone is to die soon.
“For older adults, understanding life expectancy can guide decisions about the continuation of preventive screenings like colonoscopy.”
— Lee et al., Journal of General Internal Medicine
Risk-Benefit Analysis for Elderly Patients
For older patients, weighing the risks and benefits of colonoscopy is vital. This means looking at the possible harms, like perforation or problems from sedation, against the chance of catching and preventing colon cancer.
Deciding to keep or stop colonoscopies should be tailored to each patient. It depends on their health, what they value, and their personal preferences.
Are Colonoscopies Necessary? Cases Where They May Be Avoided
Colonoscopies are key in preventive care, but not always needed. The choice to get a colonoscopy depends on your health and risk factors.
Younger Patients with IBS Without Alarm Features
Young people with Irritable Bowel Syndrome (IBS) without alarm signs like bleeding or weight loss might not need a colonoscopy right away. Guidelines suggest they can start with treatments based on their symptoms. But, if alarm signs show up, they need more tests.
Recent Normal Colonoscopy
If you’ve had a normal colonoscopy recently, you might not need another one for a while. Current guidelines say wait 10 years if you have no other risk factors. Your doctor might suggest a different wait time based on your health.
Terminal Illness Considerations
For those with terminal illnesses, weighing the benefits of a colonoscopy against its risks is important. Often, the focus turns to improving life quality, making a colonoscopy not always necessary.
Low-Risk Patients with Alternative Screening Options
Low-risk patients, like those without a family history of colorectal cancer, might have other screening choices. Fecal immunochemical testing (FIT) and other tests can be good alternatives to colonoscopy for a first check. The right choice depends on what you prefer, your risk, and what your doctor thinks.
In summary, colonoscopies are important for preventing and finding colorectal cancer, but not for everyone. Doctors can decide if a colonoscopy is needed based on your health and situation.
Alternatives to Colonoscopy for High-Risk Patients
For those at high risk, there are safer screening options than colonoscopy. These alternatives are better for people with health issues or who are older. They offer a gentler way to check for colorectal cancer.
Virtual Colonoscopy (CT Colonography)
Virtual colonoscopy, or CT colonography, is a safe imaging test. It uses CT scans to show the colon’s details. It’s great for those who can’t have a regular colonoscopy or prefer a less invasive method.
Benefits: It doesn’t need sedation, has fewer risks than traditional colonoscopy, and is okay for some patients who can’t have colonoscopy.
Fecal Immunochemical Testing (FIT)
FIT is a simple test that finds hidden blood in stool, an early cancer sign. It’s done yearly at home. This makes it easy for those who find colonoscopy hard to prepare for or uncomfortable.
Advantages: It’s easy to do, doesn’t need special diet, and avoids the dangers of invasive tests.
Flexible Sigmoidoscopy
Flexible sigmoidoscopy looks at the lower colon with a flexible tube and camera. It’s more invasive than FIT but less than a full colonoscopy. It’s for those needing a closer look at the lower colon but not ready for a full colonoscopy.
Considerations: It needs some bowel prep, less than colonoscopy, but doesn’t check the whole colon.
Stool DNA Testing
Stool DNA testing finds cancer cells or polyps in stool without invasive methods. It aims to catch colorectal cancer early. It’s more sensitive than FIT for finding big polyps.
Key Points: It’s a one-time test, no bowel prep needed, and can spot cancers and big polyps.
Consent Issues and Patient Refusal
Informed consent is key in colonoscopy prep. It makes sure patients know what’s coming. They learn about the procedure’s benefits, risks, and other options to decide if they want it.
Informed Consent Requirements
For a colonoscopy, informed consent covers a few important points. These include the procedure’s details, its benefits, possible risks, and other options. Patients must know they can say no at any time.
The consent talk should be easy for patients to understand. We should avoid using hard medical terms. It’s also important to let patients ask questions and clear up any doubts they have.
Patient Autonomy and Decision-Making
Patient autonomy is a big deal in medical ethics. It means patients have the right to choose their healthcare. In colonoscopy, this means they can accept or refuse based on their own choices and understanding.
To support patient autonomy, we need to make sure the consent process is complete. Patients should not feel pushed into a decision. We must check if they can make decisions on their own and if they’re not being influenced unfairly.
|
Key Elements of Informed Consent for Colonoscopy |
Description |
|---|---|
|
Nature of the Procedure |
Explanation of what a colonoscopy entails. |
|
Expected Benefits |
Discussion of how colonoscopy can help in diagnosis or treatment. |
|
Potential Risks and Complications |
Overview of possible risks, such as bleeding or perforation. |
|
Alternative Options |
Information on other diagnostic or therapeutic alternatives. |
Documentation of Refusal
If a patient chooses not to have a colonoscopy after being informed, we must document this. The record should show the patient’s understanding, their reasons for not wanting it, and that they were allowed to ask questions.
Recording a patient’s refusal respects their autonomy. It also protects healthcare providers from future legal issues or claims of negligence.
Preparing for a Colonoscopy: Contraindications to Preparation Methods
Getting ready for a colonoscopy is key, but some health issues can make usual prep methods risky. We must check each patient carefully before the test to spot any prep-related dangers.
Bowel Prep Contraindications
Prepping the bowel is vital for a good colonoscopy. Yet, some health problems can make usual prep methods unsafe. For example, those with severe bowel obstruction or bowel perforation should avoid standard prep to prevent making their condition worse.
Also, people with gastroparesis or other issues that slow down bowel movement might need special prep. It’s important to look at each patient’s health history and current condition to find the best prep plan.
Medication Interactions
When getting ready for a colonoscopy, drug interactions are a big deal. Some medicines, like anticoagulants and antiplatelet agents, might need to be stopped or changed to lower bleeding risks.
Also, those on meds that can cause dehydration or electrolyte imbalances, like some diuretics, need close watch during prep. We must check each patient’s meds for possible interactions and act on them.
Renal and Cardiac Considerations
People with renal impairment or cardiac conditions need special care before a colonoscopy. The prep can lead to dehydration and electrolyte problems, which are big worries for those with kidney or heart issues.
For those with serious kidney or heart problems, we might adjust the prep or keep a closer eye on them. This could mean using gentler bowel prep options or making sure they stay hydrated and balanced in electrolytes during prep.
Should I Get a Colonoscopy? Discussing Risks with Your Doctor
Before deciding on a colonoscopy, talk to your doctor about the risks. This talk is key to knowing the good and bad sides of the procedure.
Important Questions to Ask
When you talk to your doctor about a colonoscopy, ask important questions. This ensures you know all you need to make a good choice. Here are some questions to consider:
- What are the specific risks associated with my health condition?
- How will the procedure be performed, and what kind of sedation will be used?
- What are the chances of complications, and how will they be managed?
- Are there any alternative screening methods that might be more suitable for me?
Personalized Risk Assessment
A personalized risk assessment is vital. Your doctor will look at your health history, current health, and family history. This helps them give you a risk assessment that fits you.
This assessment will show you the good things about a colonoscopy, like catching cancer early. It will also talk about the possible risks and problems.
Shared Decision-Making Process
The shared decision-making process is a team effort. You and your doctor will talk about what you want and need. This helps make a decision that’s best for you.
By working together, you can make a choice about a colonoscopy that’s right for you. It’s based on medical facts and what you feel is best.
Talking to your doctor about the risks and benefits of a colonoscopy is a big step. Asking the right questions and understanding your risk helps you make a choice that fits your needs.
Conclusion: Making an Informed Decision About Colonoscopy
Deciding on a colonoscopy means knowing its purpose, risks, and benefits. We’ve looked at age guidelines, family history, and symptoms that suggest you might need one. These factors help decide if a colonoscopy is right for you.
Think about your own health risks, like heart problems or serious illnesses. If you’re at high risk, there are other tests like virtual colonoscopy or stool tests. These can be safer options for you.
Talking to your doctor is key. Share your health history, current health, and any worries you have. This way, you can understand when a colonoscopy is needed and what risks you might face.
Choosing to have a colonoscopy depends on your unique situation. Weighing the benefits against the risks is important. Being well-informed helps you make the best choice for your health. We’re here to support you in this decision.
FAQ
What is a colonoscopy and why is it performed?
A colonoscopy lets doctors see inside the colon and rectum. It helps find colon cancer, polyps, and other issues. It also lets doctors remove polyps and take tissue samples.
Are colonoscopies safe?
Colonoscopies are usually safe when done by skilled doctors. But, like any procedure, there are risks. These include perforation, bleeding, and reactions to sedation.
Is a colonoscopy considered a surgical procedure?
Though not surgery, a colonoscopy is an invasive test. It needs sedation and uses a flexible tube with a camera in the colon.
When should I get a colonoscopy?
The age for a colonoscopy varies based on risk and family history. For most, screening starts at 45 if at average risk.
What are the contraindications for a colonoscopy?
Colonoscopy is not recommended for those with recent heart attacks, severe heart issues, peritonitis, or recent colon surgery.
Can I have a colonoscopy if I have a severe medical condition?
People with serious health issues need a careful check to see if a colonoscopy is right for them.
How often should I have a colonoscopy?
How often you need a colonoscopy depends on your risk, past results, and any polyps or issues found.
Are there alternatives to colonoscopy for colon cancer screening?
Yes, you can choose from virtual colonoscopy, fecal tests, flexible sigmoidoscopy, or stool DNA tests.
Can I refuse a colonoscopy?
Yes, you can choose not to have a colonoscopy after knowing the risks and benefits. You must give informed consent first.
What are the risks associated with colonoscopy preparation?
When getting ready for a colonoscopy, consider bowel prep issues, drug interactions, and heart and kidney health.
At what age can you stop having colonoscopies?
Stopping colonoscopies depends on your health, how long you might live, and your risk factors. For older adults, consider frailty and life expectancy.
Is a colonoscopy dangerous for older adults?
Older adults might face more risks from colonoscopy due to health issues and frailty. It’s important to weigh the risks and benefits.
Should I discuss the risks and benefits of colonoscopy with my doctor?
Yes, talking about the risks and benefits with your doctor is key to making a well-informed choice about the procedure
.
References
American Academy of Family Physicians. (n.d.). Colonoscopy: Position paper. Retrieved from https://www.aafp.org/about/policies/all/colonoscopy-position-paper.html










