Hematopoiesis is how blood cells are made. It happens mainly in the bone marrow and a bit in the spleen. At Liv Hospital, we know how important it is to understand the five key cell types made here.
These cells are key for oxygen transport, clot formation, and immune defense. Making these cells is vital for staying healthy and fighting off infections. To find out more about what starts hematopoiesis, check out our page on hematopoiesis triggers.

The hematopoietic system is key for making blood cells. It includes the bone marrow and spleen. These parts work together to create the blood cells we need for life.
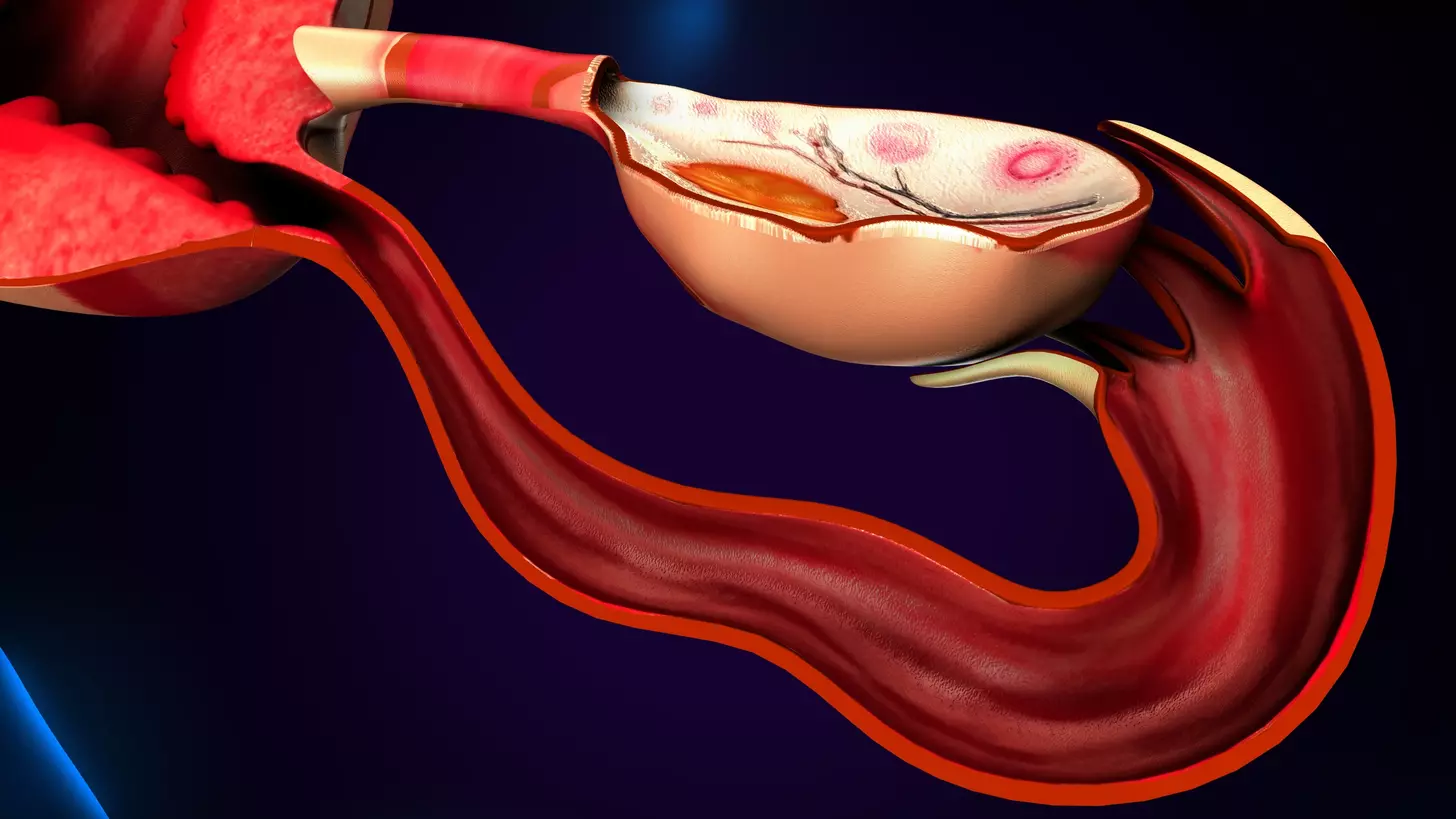
Bone marrow is where blood cells are made in adults. It fills the bones and has a special tissue called reticular tissue. This tissue helps blood cells grow.
The bone marrow is full of blood vessels. These vessels, like sinusoids, help new blood cells get into the blood. It’s a place where blood cells start their journey.
The bone marrow is full of different cells. There are stem cells, progenitor cells, and mature blood cells. They all need a special environment to grow. This environment includes stromal cells, growth factors, and extracellular matrix.
The spleen is important for the hematopoietic system. It filters the blood and stores lymphocytes. It has two main parts: the white pulp and the red pulp.
The white pulp is full of lymphocytes. It helps fight off infections. The red pulp filters the blood. It removes old or damaged red blood cells.
The spleen’s design helps it filter blood and watch for infections. It has venous sinuses for slow blood flow. This helps remove harmful things from the blood. The spleen also stores platelets and lymphocytes. It releases them when needed.

Hematopoietic stem cells are key to making blood cells. They can grow and change into every type of blood cell. This is vital for keeping our blood healthy.
These stem cells go through a complex process to become different blood cells. This is all thanks to molecular signals that guide them.
As they change, they lose their ability to grow back into stem cells. But they gain new functions. This leads to the creation of all the blood cells we need to stay healthy.
The environment around these stem cells plays a big role in how they work. The bone marrow is like a special home for them. It gives them the signals they need to keep going and to change into different cells.
We know how important the environment is for these stem cells. Scientists are working hard to understand how it all works.
The making of red blood cells, or erythropoiesis, happens in the red bone marrow. It’s a detailed process where stem cells turn into mature red blood cells. These cells then carry oxygen throughout the body.
Erythropoiesis is a complex process with many stages. It starts with stem cells choosing to become red blood cells. The red bone marrow has a special environment for this to happen.
As red blood cells grow, they lose their nucleus and get more hemoglobin. Hemoglobin is key for carrying oxygen. “The body controls how many red blood cells it makes based on oxygen levels,” says a key hormone called erythropoietin.
Mature red blood cells are shaped like a disk to carry oxygen well. Their shape and flexible membrane help them move through tiny spaces in the body.
These cells carry hemoglobin, which picks up oxygen in the lungs and releases it to the body’s tissues. “Red blood cells are amazing at delivering oxygen,” says a hematologist.
The spleen is important for keeping red blood cells healthy. It filters out old or damaged cells, making sure only good ones stay in the blood.
This helps keep the body healthy by preventing bad red blood cells from causing problems. “The spleen’s role in getting rid of old red blood cells is vital,” says a key point about how different parts of the body work together.
Platelets are key to our body’s healing and keeping blood vessels healthy. These small, irregularly-shaped cells stop too much bleeding when a vessel is hurt.
Platelets are made in the bone marrow through thrombopoiesis. It starts with megakaryocytes, large cells that split into platelets. Thrombopoietin, made by the liver and kidneys, helps these cells grow and mature.
“The production of platelets is a complex process that involves the coordinated effort of multiple cell types and regulatory factors,” showing how thrombopoiesis works.
Platelets don’t have a nucleus, making them flexible and good at their job. They have granules with proteins and molecules needed for clotting. When a blood vessel is injured, platelets stick to it, attract more, and release their contents to form a clot.
The spleen is important in the life of platelets, removing old or damaged ones. This keeps the platelets in the blood good and working right. About one-third of our platelets are in the spleen, ready to be used when needed.
Splenic sequestration helps control platelet numbers and makes sure they can stop bleeding well.
Granulocytes are key players in our immune system. They fight off different pathogens. These cells come from the bone marrow and help keep us safe from infections. We’ll look at the different types of granulocytes and what they do.
Neutrophils are the most common type of granulocyte. They are the body’s first defense against bacteria. They move quickly to where the infection is and eat the bacteria.
They also release enzymes and antimicrobial peptides. This helps get rid of the pathogens. Without enough neutrophils, we’re more likely to get sick.
Eosinophils fight parasites and help with allergic reactions. They release toxins that harm parasites. They also help with allergic diseases by causing inflammation.
Basophils are the least common granulocyte but important for allergies and inflammation. They release histamine, which makes blood vessels wider. This leads to symptoms like itching and swelling.
Basophils also help fight parasites, but how they do it is not fully understood.
Monocytes and macrophages are key players in fighting infections. They help get rid of harmful substances and play a big role in our immune system.
Monocytes start in the bone marrow. They come from stem cells that turn into monocyte progenitors. Studies show growth factors and cytokines are important in this process.
After they mature, monocytes move into the bloodstream. They stay there for a few days before they go into tissues.
Monocytes turn into macrophages in tissues. These tissue-resident phagocytes help keep tissues healthy and fight off pathogens. The tissue environment helps shape their role.
Macrophages are very flexible. They can engulf foreign particles, present antigens, and make cytokines and chemokines.
The spleen has special macrophages for filtering blood. Splenic macrophages in the red pulp and marginal zone are key to the immune response.
They clear out dead cells and debris. This helps keep tissues healthy and prevents inflammation.
| Macrophage Population | Location | Function |
|---|---|---|
| Red Pulp Macrophages | Red pulp of the spleen | Removal of aged or damaged red blood cells |
| Marginal Zone Macrophages | Marginal zone of the spleen | Capture of pathogens and antigens |
| Tissue-Resident Macrophages | Various tissues | Tissue homeostasis and immune response |
Monocytes and macrophages are essential for our immune system. They work together to fight infections and keep tissues healthy. Their development and functions are complex but vital for our health.
Lymphocytes are key to our body’s defense. They help us fight off infections and diseases. These cells are vital for our health.
B cells grow in the bone marrow. They go through a complex process to become ready to fight off infections. The bone marrow creates a special environment for B cell growth (NCBI).
B cells go through several stages in their development. They are tested at each stage to make sure they can fight off infections. This ensures they can recognize and attack foreign substances.
The spleen is important for B cell growth and activation. It helps B cells become ready to fight off infections. The spleen’s structure is perfect for this process.
When B cells meet antigens, they become active. They start to multiply and turn into cells that make antibodies. These antibodies help fight off infections.
T cells start in the bone marrow but mature in the thymus. T cell precursors move to the thymus for maturation.
In the thymus, T cells are tested to make sure they can fight off infections without attacking the body. This process is strict to prevent autoimmunity.
We know how important lymphocytes are for our immune system. They help us stay healthy by fighting off infections. Learning about them helps us understand and treat immune disorders.
Hematopoiesis is the process of making blood cells. It involves many cell types and organs, like the bone marrow and spleen. This complex process keeps our blood cell count healthy.
The process of making blood cells is tightly controlled. Key regulators include erythropoietin, thrombopoietin, and colony-stimulating factors. These help turn stem cells into different blood cells.
Keeping the right balance of blood cells is key to health. This balance lets our body respond to needs, like making more red blood cells when we’re anemic.
| Regulatory Factor | Function | Target Cell Lineage |
|---|---|---|
| Erythropoietin | Stimulates red blood cell production | Erythrocytes |
| Thrombopoietin | Promotes platelet production | Megakaryocytes/Platelets |
| Colony-Stimulating Factors (CSFs) | Enhances white blood cell production | Granulocytes, Monocytes |
In severe cases, like anemia, the spleen starts making blood again. This is called extramedullary hematopoiesis. This can cause the spleen to grow and change how it makes blood cells.
Extramedullary hematopoiesis shows how our body can adapt when making blood is disrupted. The spleen’s role in filtering blood makes it a good place for this to happen.
The bone marrow and spleen work together in making blood. This shows how complex and adaptable our blood-making system is. Knowing how this works helps us understand and treat blood-related disorders.
We see many clinical disorders that mess with blood cell making. Each one has its own reasons and effects. These issues can really change how blood cells are made and work, causing different problems.
Bone marrow failure syndromes, like aplastic anemia, stop the bone marrow from making blood cells. This can happen for many reasons, like autoimmunity, toxins, or viruses. Aplastic anemia means the bone marrow can’t make new blood cells, leading to a lack of all blood cell types. Treatment might include medicines or a bone marrow transplant.
Myeloproliferative neoplasms (MPNs) make too many mature blood cells. This includes polycythemia vera, essential thrombocythemia, and primary myelofibrosis. Myelodysplastic syndromes (MDS) make blood cells poorly, leading to low blood counts and a chance of leukemia. Managing these disorders means figuring out the risk and choosing the right treatment.
The spleen filters blood and stores red blood cells and platelets. Problems with the spleen, like hypersplenism, can cause too many blood cells to be destroyed. Hypersplenism means too many blood cells are trapped in the spleen, often because it’s too big. Treatment might fix the spleen problem or remove it.
In summary, disorders affecting blood cell making are complex and varied. Understanding them helps us diagnose and treat patients better. This improves their health and life quality.
Recent breakthroughs in hematology and immunology have changed how we see blood cell formation and immune function. These discoveries have not only deepened our understanding but have also led to new treatments for blood disorders.
The process of making blood cells is complex, involving many molecular steps. Recent studies have uncovered the roles of specific genes and pathways in guiding blood stem cells. For example, the RUNX1 gene is key in blood stem cell development. Knowing this can help in creating targeted treatments for blood cancers.
We’re starting to see the complexity of the blood system and how it’s controlled at a molecular level. This knowledge is vital for finding new treatments for blood diseases.
Transfusion medicine has seen big changes, like personalized transfusions. This means blood transfusions are tailored to each patient, improving results and reducing risks.
Genomic sequencing and precision medicine help match donor blood to recipients better, lowering the chance of bad reactions. Also, new ways of making blood products have made them safer and more available.
| Innovation | Description | Benefit |
|---|---|---|
| Personalized Transfusion Therapy | Tailoring blood transfusions to individual patient needs | Improved patient outcomes |
| Genomic Sequencing | Advanced matching of donor blood to recipients | Reduced risk of adverse reactions |
| Blood Component Manufacturing | Improved availability and safety of blood products | Enhanced patient safety |
Cellular therapies are a new hope for treating blood diseases. Chimeric Antigen Receptor (CAR) T-cell therapy has shown great success in fighting some blood cancers.
Other cell therapies, like gene-edited cells and stem cell transplants, are also on the rise. They promise to treat a wide range of blood conditions, from leukemia to sickle cell disease.
As we explore these new therapies, we’re hopeful about their impact on blood disease treatment. Cellular therapies could bring new hope to patients with hard-to-treat conditions.
Our team at Liv Hospital is committed to top-tier care for patients with hematological conditions. We use a collaborative approach. This means we work together with hematologists, specialists, nurses, and support staff.
Multidisciplinary care is key in our hematology department. We team up experts from different fields to make personalized treatment plans. This ensures our patients get all-around care, from start to finish.
Liv Hospital has the latest diagnostic tools and treatment facilities. This lets us offer advanced care for hematological disorders. Our diagnostic tools include advanced lab tests and imaging, helping us diagnose and monitor conditions accurately.
We use innovative treatment modalities like targeted therapies and stem cell transplantation. These are tailored to each patient’s needs. Our treatments are based on the latest research and guidelines, ensuring our patients get the best care.
At Liv Hospital, we’re dedicated to improving hematology through research and clinical trials. Our research aims to better understand hematological disorders and find new treatments. By joining clinical trials, we offer our patients access to new therapies.
Our focus on clinical excellence shows in our strict care standards and ongoing efforts to improve patient outcomes. We believe combining research with clinical practice can greatly benefit our patients.
Our approach at Liv Hospital includes a multidisciplinary team, advanced diagnostics and treatments, and research. We aim to provide the best care for patients with hematological disorders. We want to positively impact our patients’ lives, giving them hope and support every step of the way.
The bone marrow and spleen are key in making blood cells. They help keep our bodies healthy. These organs are vital for our immune system and overall health.
When these organs don’t work right, it can cause problems. This can make it hard for our bodies to fight off infections. Knowing how they work is important for treating diseases.
At Liv Hospital, we understand how important these organs are. We offer a wide range of treatments for blood-related issues. Our team uses the latest technology to help our patients.
Studying the bone marrow and spleen helps us learn more about keeping people healthy. More research will help us find better ways to prevent and treat diseases.
Blood cells are mostly made in the bone marrow. Some are also made in the spleen. The bone marrow is the spongy tissue inside bones like the hips and thighbones. It makes blood cells through a process called hematopoiesis.
The spleen filters the blood and stores lymphocytes. It can also make blood cells, mainly during fetal development. In adults, it can start making blood cells again under certain conditions, called extramedullary hematopoiesis.
Hematopoietic stem cells are in the bone marrow. They can turn into all blood cell types, like red and white blood cells, and platelets. They’re key for keeping the body’s blood cell supply and for renewing blood cells.
Red blood cells have a protein called hemoglobin. It grabs oxygen in the lungs and releases it to tissues. This way, oxygen gets to all parts of the body, helping cells work properly.
Platelets, or thrombocytes, are vital for blood clotting and stopping bleeding. When a blood vessel gets hurt, platelets gather and form a plug to stop the bleeding.
Granulocytes, a type of white blood cell, fight infections by eating foreign particles and microorganisms. Different granulocytes, like neutrophils and eosinophils, have unique roles in fighting infections.
The spleen filters the blood, removing old or damaged red blood cells. This keeps red blood cells healthy and prevents damaged cells from causing anemia or other problems.
Liv Hospital uses a team approach to hematological care. They use the latest diagnostic and treatment methods and research to improve care. This ensures patients get top-notch care for various blood disorders.
Disorders like bone marrow failure, myeloproliferative and myelodysplastic diseases, and splenic disorders can affect blood cell production. These can lead to issues like anemia, infections, and bleeding problems.
New advances include better understanding of blood cell production, improvements in transfusion medicine, and new cell therapies for blood disorders. These advancements are helping patients and expanding treatment options.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us