Last Updated on November 3, 2025 by mcelik

Understanding the Side Effects of Prostate Removal
Prostate surgery is a common treatment for prostate cancer, but many men worry about what comes after — especially the side effects of prostate removal. While some discomfort and pain are normal, studies show that these can be effectively managed with proper care and medication.
Facing surgery can be emotionally challenging. One patient shared, “I didn’t want to step on faith, but I was like, God, I want to be able to walk.” His words reflect both the emotional and physical struggles patients often face during recovery.
At Liv Hospital, we focus on easing these challenges by providing personalized care and guiding patients toward a smooth, confident recovery.
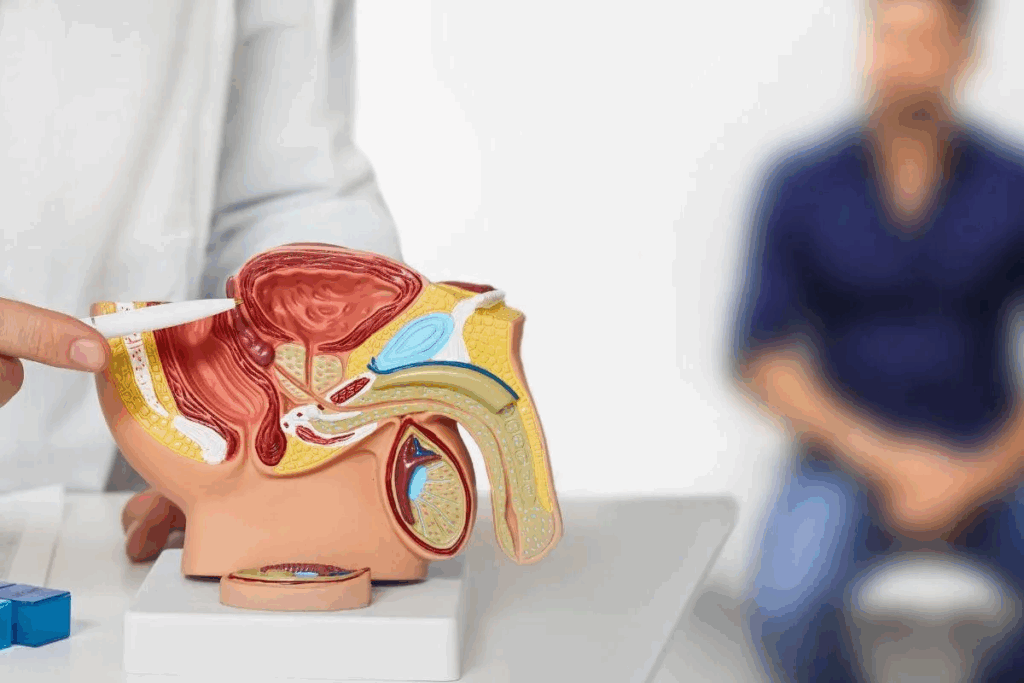
Prostate surgery includes many methods, each with its own advantages and challenges. Knowing these differences helps patients choose the best treatment for them.
Open radical prostatectomy is a traditional surgery. It involves one big cut in the belly to reach the prostate. This method has been used for years and removes the prostate and nearby tissues.
Though effective, it can lead to longer healing times and bigger scars. This is compared to newer, less invasive methods.
Laparoscopic radical prostatectomy is a newer, less invasive surgery. It uses small cuts and special tools to remove the prostate. This method causes less blood loss, less pain, and faster healing.
But it needs skilled surgeons and might not work for everyone.
Robotic-assisted prostatectomy is a high-tech version of laparoscopic surgery. It uses a robotic system for better vision and tools. This allows for more precise surgery and possibly better results.
Patients like O’Phelan, who chose this method, often have less pain and heal faster.
TURP is a surgery for urinary problems caused by an enlarged prostate. It doesn’t remove the prostate but cuts away tissue blocking urine flow. This surgery goes through the urethra, avoiding big cuts.
It’s often suggested for patients with benign prostatic hyperplasia (BPH).
Each surgery has its own uses, benefits, and risks. The right choice depends on the patient’s health, cancer stage, and the surgeon’s skill. By knowing the different prostate surgeries, patients can make informed decisions that fit their needs.

Before prostate surgery, talk to your doctor about pain management. Knowing what pain you might feel and how it will be handled can make your recovery better.
During pre-surgical talks, ask about pain relief options. Your doctor can tell you what to expect based on your surgery and health.
It’s important to know what pain you might feel after surgery. Everyone feels pain differently. Talking about the usual pain levels for your surgery can help you prepare.
There are steps you can take before surgery to feel less pain. Physical therapy can help strengthen your muscles. Also, follow your doctor’s advice on medication, diet, and other pre-surgery tips.
The length of your hospital stay depends on your surgery type. For example, robotic-assisted prostatectomy might mean a shorter stay than open radical prostatectomy. Knowing how long you’ll stay can help you plan your recovery.
The first 24-48 hours after prostate surgery are very important. During this time, patients are watched closely for any problems. Managing pain is a top priority.
Pain levels can differ a lot among patients after prostate surgery. Some might feel only mild discomfort, while others might have more pain. Effective pain management is essential for a comfortable recovery.
We use a mix of medicines and other methods to manage pain during this key time. Patients get pain relief medicine, and the amount is adjusted for their needs.
Pain after prostate surgery can be felt in different parts of the body. Common areas include the abdomen, lower back, and the perineal region. Understanding the sources of pain helps in managing them better.
The type of surgery can affect where and how much pain is felt. For example, patients who have open radical prostatectomy might feel more abdominal pain than those who have robotic-assisted surgery.
Discomfort from the catheter is common after prostate surgery. Patients might feel a need to urinate urgently or discomfort in the urethra. Catheter-related discomfort is usually managed with medicine and by making sure the catheter is correctly placed.
Several factors can change how much pain patients feel after prostate surgery. These include the surgery type, how much pain a person can handle, and if there are any complications.
By knowing these factors and working with healthcare providers, patients can manage their pain better. This improves their recovery experience.
After prostate surgery, patients need to know their pain management options. Good pain management helps them recover faster and feel better. It lets them get back to their daily activities sooner and with less discomfort.
Many medications help manage pain after prostate surgery. Opioids are often used for severe pain, but doctors watch their use closely to avoid addiction. For milder pain, non-opioid analgesics like acetaminophen or NSAIDs are recommended.
“Pain management is not just about medication; it’s about finding a balance that works for you. We work with our patients to develop a personalized pain management plan that minimizes discomfort and promotes healing.
There are also non-medication ways to manage pain after prostate surgery. These include:
Managing pain at home needs some planning. Patients should:
While some pain is normal after prostate surgery, there are times to call the doctor. Severe pain, pain that gets worse, or pain with other symptoms like fever or trouble urinating needs medical attention.
“It’s always better to err on the side of caution when it comes to pain after surgery. We’re here to support our patients throughout their recovery journey.
Knowing what to expect after prostate surgery is key. Everyone recovers differently, but there are common steps most people go through.
The first week is usually the toughest. You might feel pain, swelling, and bruising where you had surgery. Managing pain well is important, and you can do this with medicine and rest.
It’s important to follow your doctor’s advice on pain relief. Tell them if your pain gets worse or is too much.
By the second to fourth week, things start to feel better. The pain lessens, and you can start doing more things. But remember to stay away from heavy lifting and hard activities for now.
In the first to third months, most people feel much better. You might feel some pain now and then, but it’s usually not too bad. You can use over-the-counter pain meds for it.
Even though most men feel better in a few months, some might not. If you’re feeling pain that won’t go away, talk to your doctor. They can check if everything is okay.
| Recovery Stage | Typical Pain Experience | Recommended Actions |
| First Week | Significant pain and discomfort | Follow prescribed pain management, and rest adequately |
| Weeks 2-4 | Gradual reduction in pain | Resume normal activities gradually, and avoid heavy lifting |
| 1-3 Months | Minimal pain, significant recovery | Continue with gentle exercises, monitor for any unusual pain |
It’s important for patients to know about the side effects of prostate removal. This surgery can cause different issues, some short-term and others long-term. Understanding these can help with recovery and managing expectations.
Urinary incontinence is a common side effect. It can range from a little leakage to not being able to control your bladder. Pelvic floor exercises, like Kegel exercises, can help improve urinary continence over time. How long it takes to get better varies, with some seeing improvement in a few months and others taking longer.
Erectile dysfunction (ED) is another possible side effect. Some men might not be able to get an erection at all, while others might have a weaker one. Nerve-sparing techniques during surgery can help preserve sexual function. But how well these techniques work depends on the patient’s age and the surgeon’s skill.
The surgery can also change how you ejaculate and orgasm. You might have dry orgasms because of the removal of the prostate and seminal vesicles. These changes can be hard to get used to, but many men find a way to adapt over time.
The effects of prostate removal can also affect your mind. They can impact your self-esteem, body image, and quality of life. Support from healthcare providers, counselors, or support groups can be invaluable in coping with these changes. It’s key to talk about your feelings and concerns with your healthcare team for the right guidance and support.
| Side Effect | Potential Impact | Management Strategies |
| Urinary Incontinence | Loss of bladder control | Pelvic floor exercises, lifestyle adjustments |
| Erectile Dysfunction | Reduced or lost erectile function | Nerve-sparing surgery, medication, and counseling |
| Changes in Ejaculation | Dry orgasms, altered sensations | Counseling, support groups |
Knowing where pain happens after prostate surgery is key to managing it. Pain can show up in different spots. Finding out where it comes from helps to ease the discomfort.
Many people feel pain in their abdomen after surgery. This pain comes from the cut made during surgery. It can be mild or quite strong and is often treated with medicine. Good wound care and following the doctor’s orders can lessen the pain.
“Incision site pain usually gets better as the wound heals,” a study on post-prostatectomy pain found. “But some people might keep feeling pain, and they should see a doctor again.”
Perineal pain is felt in the area between the scrotum and anus. It’s caused by the surgery. Swelling here is common, too,o and can be helped with cold packs and elevating the area. Perineal pain can be quite uncomfortable and affect daily life.
Discomfort in the testicles and groin can happen because these areas are close to the surgery site. This pain might come from swelling, bruising, or irritated nerves. Wearing supportive clothes and moving gently can help with this pain.
Buttock and rectal pain are less common but can happen. It might be from irritated nerves or pain that feels like it’s coming from the surgery area. This pain needs careful checking to make sure there’s no infection or abscess. Seeing a doctor right away is important if the pain is bad or if you have other symptoms like fever or trouble peeing.
“It’s essential for patients to communicate their pain experiences to their healthcare providers to ensure appropriate management and minimize the risk of complications.”
It’s important to know that complications after prostate surgery can make pain worse. Prostate surgery is usually safe, but there are risks. Patients should be aware of these.
Infection is a possible complication after prostate surgery. Look out for fever, chills, and redness or swelling around the incision. It’s key to watch for these signs and get medical help right away if you see them.
Common infection signs to watch for include:
Bleeding and hematoma formation can cause a lot of pain. A hematoma is blood outside of blood vessels. It can put pressure on nerves and tissues, causing discomfort.
Be aware of signs like increasing pain, swelling, or bruising around the surgical site. These could mean bleeding or a hematoma.
A lymphocele is a collection of lymphatic fluid that can occur after surgery. It can cause discomfort or pain, depending on its size. If it’s big enough, it can press on nearby structures.
Symptoms include a palpable mass, pain, or urinary issues. If you notice anything unusual, tell your healthcare provider.
Anastomotic stricture is a narrowing of the bladder and urethra. It can cause pain and urinary problems. Symptoms include weak urine flow, straining to urinate, or painful urination.
Early detection and treatment are key to managing these complications. It’s important to keep up with follow-up appointments with your healthcare provider.
Going back to normal after prostate surgery is a big step. It’s key to know how to handle pain. As you start doing daily things again, listen to your body and adjust as needed.
At first, sitting or walking might hurt because of the surgery. Here’s what to do:
Walk at a pace that feels right to you. Slowly increase how far and fast you walk as you get better.
Driving after surgery needs careful thought. We suggest:
Exercise is important for getting better. Here’s what to do:
When to start having sex again varies. Usually, we say:
Managing pain well when starting normal activities can make your recovery better. It can also improve your quality of life.
Removing the prostate gland starts a new chapter in life, full of challenges and health benefits. Patients must adjust to life without a prostate, facing physical and emotional changes.
After prostate removal, patients face many changes. Managing urine leakage is a big adjustment. Pelvic floor exercises, like Kegel exercises, help a lot.
Sexual function also changes. Erectile dysfunction and altered orgasms are common. But, with a doctor’s help, many find ways to manage these issues.
PSA monitoring is key after prostate removal. A high PSA level might mean cancer is back. Regular tests help catch problems early.
Knowing what PSA levels mean is important. A rising level might mean more tests, like scans, to check for cancer.
| PSA Level | Implication | Action |
| Undetectable | Low risk of recurrence | Regular monitoring |
| Detectable but stable | Potential for recurrence, monitoring required | Regular PSA tests, possibly additional imaging |
| Rising | Higher risk of recurrence | Further testing and potentially treatment |
Prostate removal surgery brings big changes, but many men see their quality of life improve. Managing side effects and living healthily are key to feeling good long-term.
Staying active, eating well, and seeing doctors regularly are important. This helps manage side effects and keeps you healthy.
It’s important to know the difference between permanent and temporary side effects. Some men face long-term issues, but others see these problems go away.
Talking to your doctor about what to expect is vital. Thanks to medical progress, many side effects can be managed well, improving life quality.
The type of surgery for prostate issues can greatly affect how much pain a patient feels after. It’s key to know how each method impacts recovery and pain levels.
Open radical prostatectomy needs a big cut, which can cause more pain than smaller cuts. Laparoscopic and robotic surgeries use smaller cuts. This means less damage to the body and often less pain.
Studies show people with smaller cuts feel less pain and need less medicine for it.
Robotic-assisted prostatectomy is a precise and flexible surgery. It leads to less pain and quicker healing than open surgery. The small cuts and less handling of tissues help make it less painful.
Transurethral Resection of the Prostate (TURP) is used for BPH, not cancer. It’s less invasive than a radical prostatectomy and causes less pain. But some pain can come from the catheter or urinary issues.
Many things can affect how comfortable a patient feels during recovery. These include their health, age, and any other health issues. The skill of the surgical team and post-op care also matter a lot.
Good pain management, with both medicine and other methods, is key to feeling better during recovery.
Recovering from prostate surgery is a unique journey for each patient. It’s filled with challenges and triumphs. By looking at real stories, we learn about the different ways people deal with pain and recovery.
Recovery paths after prostate surgery vary a lot. Some patients have little discomfort, while others face tough pain management. For example, some might use medicine and alternative therapies to manage pain.
We talked to several patients who had prostate surgery. Their stories show how important personalized care is. One patient managed pain with medicine, while another found relief through physical therapy and relaxation.
Managing post-prostatectomy pain needs a variety of approaches. Patients have found many strategies helpful, including:
These strategies help manage pain and improve overall well-being during recovery.
Some patients face unexpected pain challenges during recovery. For example, certain positions or activities might make pain worse. Knowing these challenges helps healthcare providers give better advice and support.
Comparing patient experiences shows that pain challenges vary. Factors like overall health, comorbidities, and surgical technique affect pain levels and types.
| Common Pain Challenges | Patient Experiences | Coping Strategies |
| Incision site pain | Sharp pain when moving or coughing | Medication, rest, and gentle stretching |
| Catheter-related discomfort | Discomfort or pain during urination | Catheter care, pain management medication |
| Generalized abdominal pain | Dull ache or cramping | Heat therapy, relaxation techniques |
Support is key for patients dealing with post-prostatectomy pain. Resources like support groups, online forums, and counseling services offer valuable help and emotional support.
We suggest patients look into these resources to find what works for them. Sharing experiences and advice helps patients support each other through recovery.
Managing your expectations is vital for a smooth recovery after prostate surgery. Knowing what pain and discomfort you might face helps you prepare and cope better.
We’ve looked at different types of pain and how to manage them after surgery. We’ve also talked about the various surgical methods and possible complications. Being informed helps patients handle their recovery better.
Good pain management is key to a comfortable recovery. Understanding what to expect and having a plan can reduce your pain. This way, you can enjoy a better quality of life after surgery.
Side effects include urinary incontinence and erectile dysfunction. You might also notice changes in ejaculation. Psychological impacts can also occur.
Recovery times vary. Most patients can get back to normal in a few weeks to months. It can take up to a year or more for full recovery.
Open prostatectomy uses a big incision. Laparoscopic and robotic prostatectomy use smaller incisions. Robotic surgery might offer more precision and less blood loss.
Pain management includes medication and non-pharmaceutical methods. Rest, ice, and pelvic floor exercises are common. Your healthcare provider will give you specific instructions.
Most people see pain decrease over time. But some may have ongoing pain. The chance and severity of long-term pain depend on the surgery and healing.
It’s best to wait a few weeks to months before starting sexual activity again. Always follow your healthcare provider’s advice.
Look out for severe pain, heavy bleeding, fever, and trouble urinating. If you see any of these, get medical help right away.
You might experience temporary or permanent urinary incontinence. Most people regain control with time and pelvic floor exercises.
PSA levels should be very low or undetectable after successful surgery. Monitoring PSA levels is important for follow-up care.
Some people may face long-term changes in urinary and sexual function. Psychological impacts can also occur. There are strategies to manage these changes.
Minimally invasive techniques like laparoscopic and robotic prostatectomy often have less pain. But everyone’s experience is different.
Robotic-assisted prostatectomy can lead to less blood loss and smaller incisions. It might also result in faster recovery times compared to open surgery.
Radiation therapy can make surgery more complicated. But, it’s not a complete no-go. The decision should be made with your healthcare provider.
Medical News Today. (2023). Long-term Pain after Prostatectomy and Its Treatment.
https://www.medicalnewstoday.com/articles/long-term-pain-after-prostatectomy
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us