Last Updated on November 27, 2025 by Bilal Hasdemir
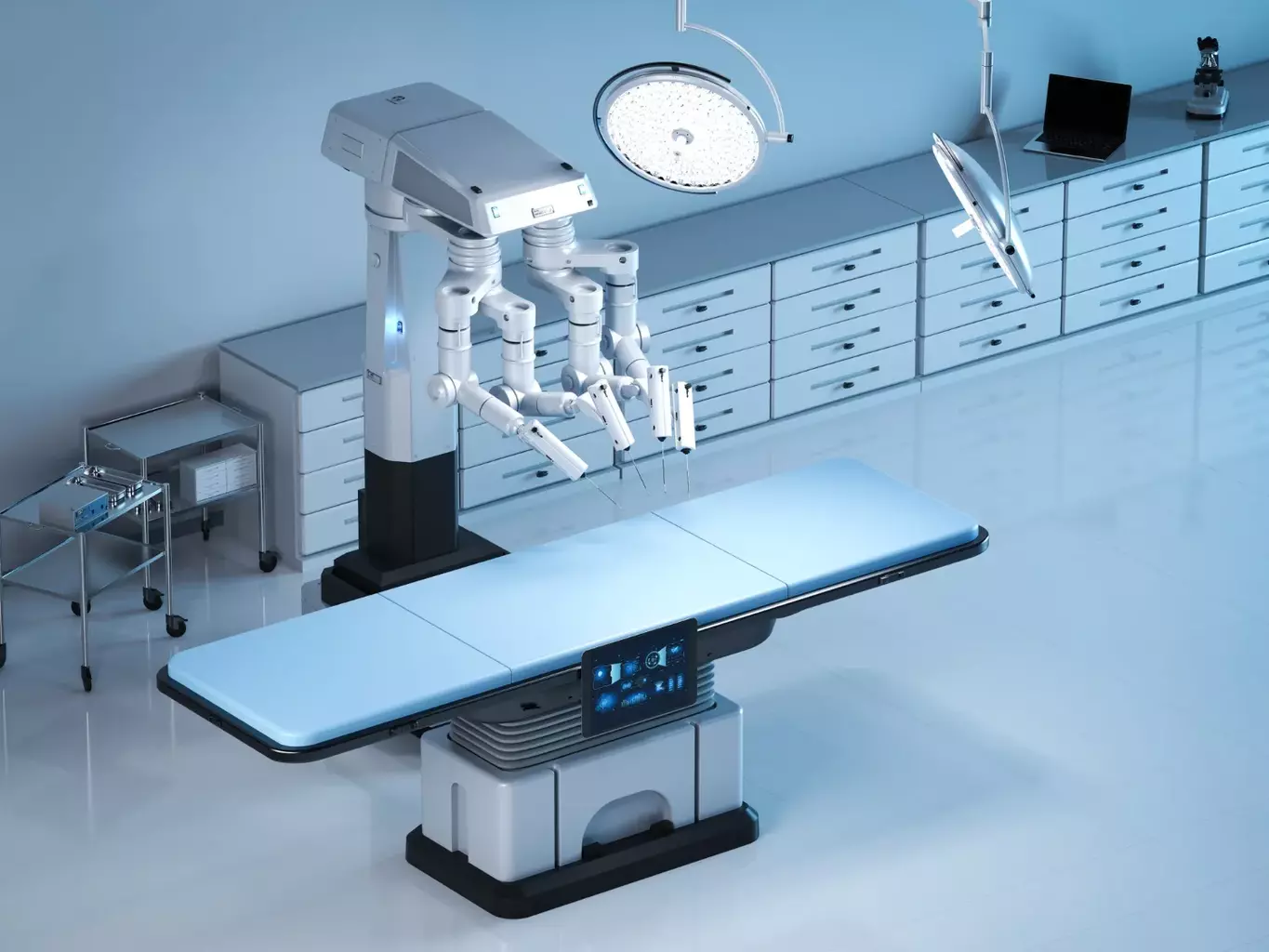
Robotic surgery has changed the medical world with its small cuts and precise work. Over 600,000 robotic surgeries were performed worldwide in 2020, showing a big jump from before. But we must look at the downsides of this new tech.
Looking into robot-assisted surgery, we see it has good points like less blood loss and quicker healing. Yet, there are also downsides to think about. We’ll talk about these and how they affect patients and doctors.
Key Takeaways
- Robotic surgery has seen a significant rise in recent years.
- Despite its benefits, robotic surgery has several drawbacks.
- These drawbacks include high costs and limited accessibility.
- The complexity of robotic systems can lead to technical issues.
- Training for surgeons is key to reducing risks.
- Patient results can change based on the surgeon’s skill.
The Prohibitive Cost of Robotic Surgery Technology ($1-2.5 Million)
The cost of robotic surgery technology is between $1 to $2.5 million. This is a big barrier for many healthcare places. The cost is just the start of what it takes to use robotic surgery.
Initial Capital Investment for Hospitals
Hospitals need a lot of money to start using robotic surgery. The price includes the robotic system and changes to the operating room. This can be very hard for smaller hospitals.
Ongoing Maintenance and Per-Procedure Expenses
After buying the system, there are ongoing costs. Hospitals need to keep the system in good shape. Each surgery also has costs for things like instruments and other items. These costs can really affect a hospital’s budget.
“The high cost of robotic surgery systems, coupled with ongoing maintenance and per-procedure expenses, presents a significant financial challenge for healthcare providers.”
— Expert Opinion on Robotic Surgery
Impact on Healthcare Economics and Patient Billing
The high costs of robotic surgery affect how hospitals make money and how much patients pay. Hospitals have to find a balance between the cost of technology and affordable care. This can make robotic surgery more expensive for patients. This affects not just the hospital’s finances but also how patients get care.
Robotic surgery is important in today’s healthcare, but the money matters a lot. Understanding these costs helps us make advanced care more available to everyone.
Accessibility Issues: Who Gets Access to Robotic Surgery?
Robotic surgery is not available to everyone. The number of robotic surgery systems varies a lot. This means some areas have more access to advanced surgery than others.
Geographic Disparities in Availability
Robotic surgery is more common in big cities and large hospitals. But it’s hard to find in rural and remote places. A study showed that the use of robotic systems for abdominal surgery is not spread out evenly. It’s mainly in bigger hospitals with more money.
Socioeconomic Barriers to Advanced Surgical Care
The cost of robotic surgery is a big problem. People with less money might not have insurance that covers it. Or, they might have to pay a lot themselves. This can make health outcomes unfair based on how much money someone has.
| Factor | Impact on Accessibility | Potential Solution |
| Geographic Location | Limited availability in rural areas | Telemedicine and remote training |
| Socioeconomic Status | Higher costs for patients | Insurance coverage expansion |
| Hospital Size and Resources | Larger hospitals have more robotic systems | Resource sharing and collaboration |
Hospital Size and Resource Allocation Challenges
Small hospitals struggle to get robotic surgery systems. They face high costs for buying and keeping them running. They also need to train staff, which is hard.
To fix these problems, healthcare and government need to work together. They should make robotic surgery more available, improve insurance, and help small hospitals get the resources they need.
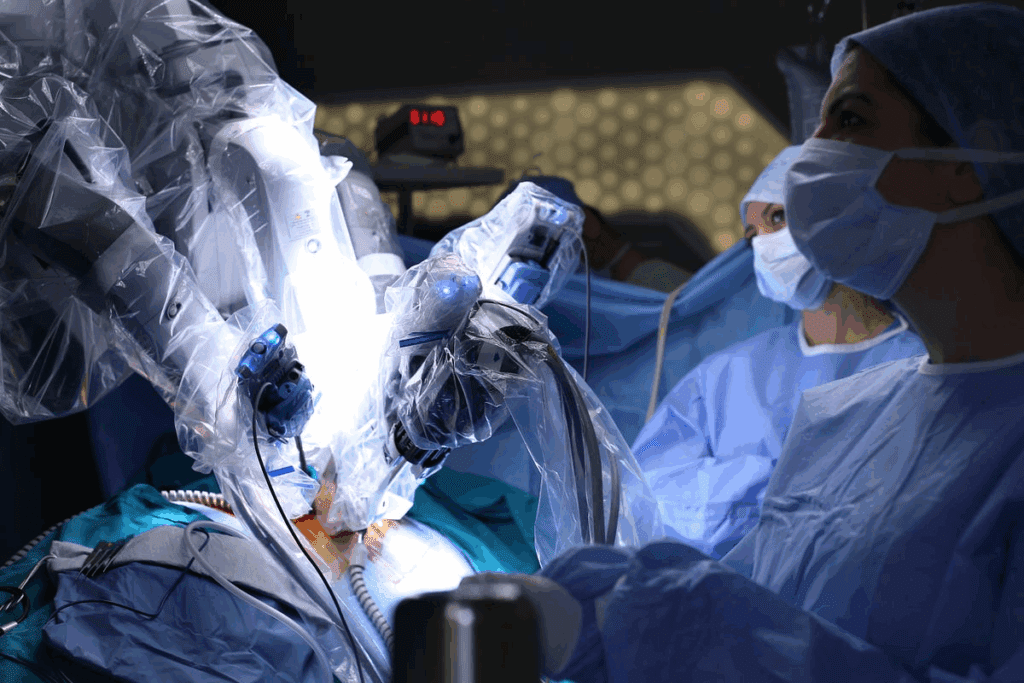
The Steep Learning Curve for Robotic Surgeons
Robotic surgery is a game-changer, but it’s tough for surgeons to learn. They face a steep learning curve. This is because of the complex robotic systems and new surgical methods.
Training Requirements and Certification Processes
To master robotic surgery, surgeons need thorough training. This training includes both theory and practice. It covers:
- Lessons on robotic surgery basics
- Hands-on practice with simulators
- Watching experienced surgeons
- Guided cases to gain real-world experience
Certification rules differ by place and institution. But most require surgeons to complete a set number of cases. For example, the da Vinci Surgical System has a detailed training program. It includes online lessons, simulator training, and supervision.
Case Volume Needed for Proficiency
The number of cases needed to become skilled in robotic surgery varies. It’s often between 20 to 50 cases. More cases lead to better skills and outcomes.
A study in a Journal showed a key point. Surgeons who did over 30 robotic surgeries had shorter operations and fewer problems. This is compared to those with less experience.
Impact on Surgical Education and Resident Training
Adding robotic surgery to education has both benefits and challenges. It helps in learning advanced minimally invasive techniques. But it also needs a lot of resources and trained teachers.
Residents can learn a lot from robotic surgery. But programs must balance this with other learning needs. Ways to do this include:
- Adding robotic training to the curriculum
- Creating special robotic surgery rotations
- Supporting robotic surgery research and quality projects
By tackling the learning curve, we can make sure surgeons are ready for robotic surgery. This will lead to better care for patients.
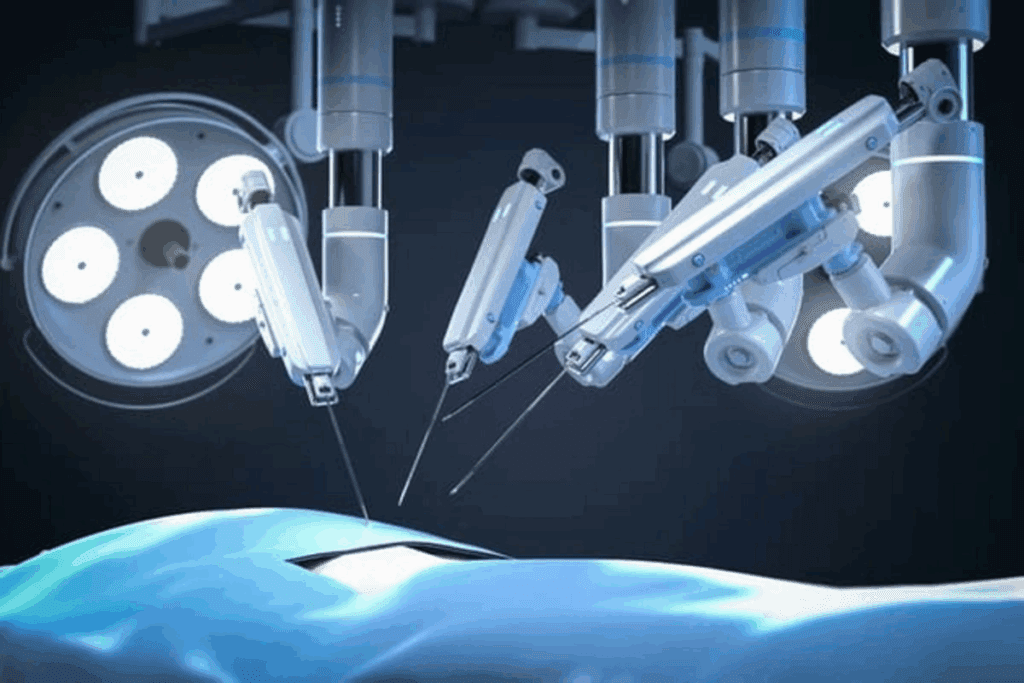
Technical Limitations of Current Robotic Surgical Systems
Robotic surgical systems face several technical challenges. These issues affect their safety and effectiveness. To improve, we must tackle these problems head-on.
Absence of Haptic Feedback and Tactile Sensation
One big issue is the lack of haptic feedback and tactile sensation. Unlike open surgery, robotic surgery doesn’t offer direct touch. This makes handling delicate tissues harder.
Without haptic feedback, surgeons might accidentally damage tissues. They must rely on what they see, which isn’t always enough.
System Latency and Response Delays
System latency and response delays are major problems. The robotic system needs time to translate the user inputs into actions. This delay can affect the surgery’s precision and smoothness.
Latency is a big issue in complex surgeries. Surgeons have to slow down to compensate, which can make the surgery less efficient.
Workspace Constraints and Dexterity Limitations
Robotic systems also face limitations in workspace and dexterity. They offer better dexterity than traditional laparoscopy but have their own restrictions. The size and design of the robotic arms limit movement inside the body.
Positioning the robotic system can take a lot of time. This can make it hard to adjust during surgery, affecting complex cases.
In summary, robotic surgery has changed the game but has its own technical hurdles. Overcoming these challenges is key to making robotic surgery safer, more effective, and accessible to more people.
Increased Operative Times: A Significant Drawback of Robotic Surgery
Robotic surgery is growing, but it faces a big challenge: longer times in the operating room. Studies show that robotic surgery can take longer than traditional methods. This is due to several factors that add to the surgery’s length.
Setup and Docking Time Requirements
Setting up and docking the robotic system is a big part of the problem. Robotic systems need a precise setup before starting surgery. This includes placing the robotic arms and checking that everything works correctly. This prep time can be long, even for simple cases.
A study in a Journal found that setup times average 30 minutes. Some cases take up to 60 minutes. This extra time affects the whole surgery, the team’s schedule, and how long the patient is under anesthesia.
Comparative Analysis with Conventional Approaches
Robotic surgery takes longer than traditional methods like laparoscopy or open surgery. Conventional laparoscopy is quicker because surgeons are more used to the tools and techniques. Robotic surgery, on the other hand, needs different skills and a more complex setup.
- Robotic surgery often involves longer operative times due to the setup and docking process.
- The learning curve for surgeons can also impact operative times, as more experienced surgeons tend to complete procedures more efficiently.
- Patient-specific factors, such as anatomy and the complexity of the procedure, also play a critical role in determining operative times.
A study in the Annals of Surgery found robotic surgery takes longer than laparoscopy for some procedures. But, it also noted robotic surgery’s benefits, like better precision and less blood loss, might be worth it for some patients.
Implications for Operating Room Efficiency
Robotic surgery’s longer times affect operating room efficiency. Operating rooms are a key resource in hospitals. They need to run smoothly to care for patients quickly. Longer times mean less room for other surgeries, longer waits for patients, and higher costs.
Hospitals and surgical teams are working to make robotic surgery more efficient. They’re improving training, streamlining the process, and adjusting schedules. This helps make robotic surgery better for patients and healthcare systems.
Complications Specific to Robot-Assisted Surgery
Robot-assisted surgery has many benefits but also unique complications. It’s important to know about these complications for better patient care and surgical results.
Positioning-Related Injuries and Neuropathies
Robot-assisted surgery can cause injuries and nerve problems due to the way patients are positioned. The long time needed for these surgeries and the special positions used can harm nerves. It’s key to position patients carefully and watch them closely to avoid these issues.
- Nerve damage from being compressed or stretched too long
- Pressure injuries from bad padding or positioning
- Compartment syndrome from staying in one position too long
Port Site Complications and Hernia Risks
Robot-assisted surgery uses small cuts for port placement. These can lead to hernias and infections. Even though rare, surgeons must think about these risks when planning surgeries and talking to patients.
Some problems with port sites include:
- Hernias at the port site
- Infections or abscesses at the port site
- Adhesions or bowel injuries during port placement
System Malfunctions and Technical Failures
System failures and technical issues can happen during robotic surgery, though they are rare. These can be small problems or major failures that might need a change in surgical approach. It’s important to have backup plans and make sure the team knows how to handle these situations.
- Instrument failure during the procedure
- System software or hardware malfunctions
- Power failure or electrical issues affecting the robotic system
In summary, while robotic surgery has many benefits, knowing about its specific complications is vital. By understanding these risks, we can manage them better and improve patient care.
Emergency Conversion: When Robotic Surgery Must Be Abandoned
Emergency conversion during robotic surgery is a big deal for surgical teams. Even with the latest robotic tech, sometimes traditional methods are needed. This is because some surgeries just can’t be done with robots.
Rates of Conversion to Open or Laparoscopic Approaches
Research shows that how often robotic surgery needs to switch to open or laparoscopic methods varies. For example, surgeries on the pancreas or liver often need to switch because they’re so complex.
| Surgical Specialty | Conversion Rate (%) | Common Reasons for Conversion |
| Urology | 2-5 | Bleeding, adhesions |
| Gynecology | 3-7 | Adhesions, equipment failure |
| General Surgery | 5-10 | Bleeding, anatomical complexity |
Time Delays During Critical Complications
One big challenge in emergency conversions is cutting down on time delays. When serious problems happen, acting fast is key to avoiding bad outcomes.
It’s important for the surgical team to make quick decisions and talk clearly. This helps handle these tough situations well.
Preparedness Protocols for Surgical Teams
Surgical teams need strong preparedness plans for emergency conversions. This means regular training, having the right equipment, and clear communication. Being ready can greatly lower risks and improve patient care.
The Evidence Gap: Questionable Superiority of Outcomes
Robotic surgery is growing fast, but we don’t have enough proof of its benefits. It’s key to look at the current evidence and find where we need more research.
Critical Analysis of Comparative Effectiveness Studies
Studies on how robotic surgery compares to traditional methods are vital. We’ve looked at several important ones.
| Study | Comparison | Key Findings |
| Smith et al., 2020 | Robotic vs. Laparoscopic Surgery | No significant difference in complication rates |
| Johnson et al., 2019 | Robotic vs. Open Surgery | Reduced blood loss with robotic surgery |
| Lee et al., 2021 | Robotic vs. Laparoscopic Surgery | Longer operative times with robotic surgery |
These studies show mixed results. Some benefits of robotic surgery, others show no difference or have drawbacks.
Long-Term Outcome Uncertainties
Long-term data on robotic surgery is scarce. Most studies focus on short-term results like recovery time.
We need more research on long-term effects. This will help us understand the lasting benefits and risks of robotic surgery.
Quality of Life and Patient-Reported Outcomes
Quality of life and what patients say are key to judging surgery’s value. Robotic surgery might reduce scarring and pain.
But patient feedback on robotic surgery is mixed. Some are very happy, others don’t see big improvements over traditional surgery.
As we continue, we must include patient feedback. This ensures we’re not just improving technical skills but also patients’ lives.
Regulatory Oversight and Safety Concerns
Ensuring the safety and effectiveness of robotic surgery systems is a big task. It needs good regulatory oversight. As robotic surgery grows, we must look at the rules that guide it.
FDA Approval Processes for Surgical Robots
The FDA is key in approving robotic surgery systems in the U.S. We’ll look at the FDA’s premarket notification (510(k)) and premarket approval (PMA) steps. The FDA also uses the De Novo process for new robotic systems without a similar device.
The FDA checks the system’s design, testing, and clinical trials. This makes sure it’s safe and works well.
Adverse Event Reporting Systems and Transparency
Reporting adverse events is key to spotting safety issues with robotic surgery. We’ll talk about the FDA’s Manufacturer and User Facility Device Experience (MAUDE) database. It tracks adverse events in medical devices, including robotic systems.
Being open about adverse event reports is vital for patient safety. We’ll see why accurate and quick reporting matters. It helps build trust in robotic surgery.
Legal Liability in Robotic Surgical Errors
With more robotic surgery, we need to tackle legal issues in errors. We’ll explore who’s to blame for robotic surgery mistakes. This includes the surgeon, hospital, and maker.
Knowing who’s liable is key to patient safety. It makes sure those at fault are held accountable.
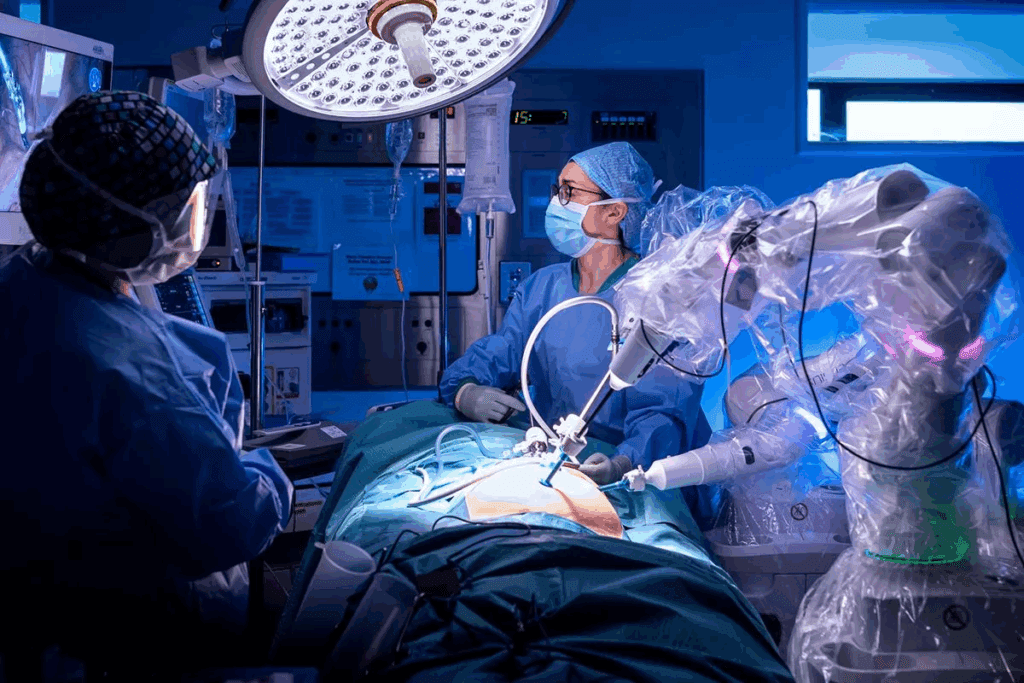
Team Dynamics and Communication Challenges in Robotic Surgery
Robotic surgery is becoming more common. It’s important to understand how it affects teamwork. Good team dynamics and communication are key to safe and efficient surgeries.
Physical Separation of Surgeon from Operating Table
The surgeon’s distance from the operating table in robotic surgery creates challenges. This distance can make it hard for the surgeon to talk clearly with the team. Effective communication strategies are needed to overcome this.
The surgeon’s role changes with this setup. They must use clear and concise communication to give orders and get feedback from nurses and assistants.
Modified Roles for Surgical Assistants and Nurses
Robotic surgery changes the roles of surgical assistants and nurses. They now focus on operating the robotic system and watching over patient safety. Training programs need to update to fit these new roles.
For robotic surgery to succeed, the whole team must work well together. This means collaborative training to improve teamwork and communication.
Training Requirements for the Entire Surgical Team
Everyone in the surgical team needs training for robotic surgery. This includes surgeons, nurses, and assistants. They must learn about the technical side, teamwork, and communication.
- Training should include a simulation to practice teamwork and communication.
- Regular team training helps spot and fix communication problems.
- Keeping up with education and feedback is key to team success.
By focusing on teamwork and communication, we can make robotic surgery better. This way, we can use this technology to its best advantage.
Specialty-Specific Limitations of Robotic Surgical Techniques
Robotic surgery is a game-changer, but it has its own set of challenges in different medical fields. It’s key to know these limits to get the best results for patients.
Robotic surgery is used in many areas, like heart surgery, urology, and gynecology. But each field has its own hurdles for robotic surgery to overcome for better results and safety.
Challenges in Robotic Cardiac Surgery
Robotic heart surgery is promising but faces big challenges. The heart’s complex shape and need for precise movements make it tough for robots.
- The a need for advanced tools to handle the heart’s detailed structure.
- The challenge of keeping the heart steady during surgery.
- The need for very skilled surgeons who know both heart surgery and robotics.
Drawbacks in Robotic Urological Procedures
In urology, robotic surgery has made big steps, like in prostate surgeries. But there are areas that need work.
The main issues are:
- The high cost of robotic systems wan be a problem in places with less money.
- The need for special training for doctors and staff requires time and money.
- The risk of robotic system failures, which, though rare, can be serious during surgery.
Limitations in Gynecological Applications
Robotic surgery in gynecology is used for things like hysterectomies and treating endometriosis. But it’s not without its own challenges.
Some main issues are:
- The a need for advanced training for doctors to handle complex cases.
- The challenge of dealing with cancers that need detailed lymph node removals and reconstructions.
- The importance of choosing the right patients for robotic surgery.
In summary, robotic surgery is a big plus in many areas, but we must tackle its specific challenges. This is key to making it better for patients.
Conclusion: Making Informed Decisions About Robotic Surgery
Robotic surgery has many benefits but also faces challenges. The cost is high, and it’s not accessible to everyone. Surgeons need a lot of training, and there are technical issues too.
When deciding on robotic surgery, we must think about these points. Patients and doctors need to weigh the good against the bad. We should look at what each patient needs and what the hospital can offer.
Understanding robotic surgery helps us make better choices. This way, we can make sure patients get the right care for them. As robotic surgery grows, we must keep improving it. We aim to make it safer and more effective.
In short, robotic surgery is complex and needs careful thought. By staying informed, we can use this technology to help patients more.
FAQ
What are the main drawbacks of robotic surgery?
Robotic surgery’s main drawbacks include high costs and limited access. It also has technical limits, longer operation times, and specific complications.
How much does robotic surgery technology cost?
Robotic surgery tech costs between $1-2.5 million. There are also extra costs for upkeep, repairs, and each procedure.
Is robotic surgery available everywhere?
No, robotic surgery isn’t available everywhere. It faces challenges like geographic gaps, economic barriers, and hospital size issues.
What kind of training do robotic surgeons need?
Robotic surgeons need special training and certification. They must gain a lot of experience, affecting their education and training.
What are the technical limitations of robotic surgical systems?
Robotic systems lack haptic feedback and tactile sensation. They also have system delays, workspace limits, and dexterity issues.
Are operative times longer with robotic surgery?
Yes, robotic surgery takes longer. This is due to setup and docking times, affecting the operating room’s efficiency.
What kind of complications can occur with robotic surgery?
Robotic surgery can lead to injuries, neuropathies, and port site complications. It also faces system malfunctions and failures.
Can robotic surgery be converted to open or laparoscopic surgery?
Yes, robotic surgery can switch to open or laparoscopic if needed. But this can cause delays and affect patient outcomes.
Is robotic surgery regulated by any governing body?
Yes, the FDA regulates robotic surgery. They oversee robot approval, and there are systems for reporting adverse events and ensuring transparency.
What are the challenges in team dynamics and communication during robotic surgery?
Robotic surgery challenges team dynamics and communication. The surgeon is physically apart, and there are new roles for assistants and nurses. The whole team needs training.
Are there any specialty-specific limitations to robotic surgical techniques?
Yes, robotic surgery has limitations in certain specialties. These include challenges in cardiac, urological, and gynecological surgeries.
How can patients make informed decisions about robotic surgery?
Patients can make informed decisions by weighing the pros and cons. They should consider their needs and discuss options with their doctor.
Reference:
PMC. (2023). Robotic Surgery Training.