Last Updated on November 27, 2025 by Bilal Hasdemir

Robotic cardiac surgery has changed the way we treat heart problems. It’s a new way to fix heart issues without a big cut. But, not everyone can have this surgery.Is a heart transplant without opening chest right for you? Discover the patients who are not candidates for this amazing procedure.
This surgery is less invasive and helps patients heal faster. Yet, some health issues and body shapes make it too risky. We’ll look at who can’t have robotic heart surgery.
Key Takeaways
- Robotic cardiac surgery is not suitable for all patients due to various health conditions.
- Certain anatomical factors can make robotic heart surgery risky.
- Minimally invasive surgery offers several benefits, including reduced recovery time.
- Understanding the contraindications is key to knowing who can have it.
- Robotic surgery is a big step forward in heart care.
Medical Evaluation Process for Robotic Cardiac Surgery
To find the right candidates for robotic cardiac surgery, a detailed medical check is needed. This check involves many tests and assessments. It helps figure out if a patient is healthy enough for the surgery.
Required Preoperative Testing
Before robotic cardiac surgery, patients must go through several tests. These tests are key to understanding the heart’s health and the patient’s overall condition. Some tests include:
- Electrocardiogram (ECG): Checks the heart’s electrical activity.
- Echocardiogram: Looks at the heart’s structure and function.
- Stress Test: Sees how the heart works under stress.
- Cardiac Catheterization: Views the coronary arteries and checks their health.
- Blood Tests: Checks blood count, kidney, and liver function.
These tests give important info about the patient’s health. This helps the medical team decide if robotic surgery is right.
Risk Assessment Protocols
Assessing risks is a big part of the medical check. We use special protocols to find out possible surgery risks. These protocols help us:
- Check the patient’s overall health.
- Find out the risk of problems during and after surgery.
- See if patients need extra care or watching during recovery.
By using these protocols, we can lower risks. This ensures patients get the best care possible.
The Multidisciplinary Heart Team Approach
Deciding on robotic cardiac surgery involves a team of experts. This team includes cardiologists, surgeons, anesthesiologists, and more. They work together to look at the patient’s health and decide the best treatment.
“A multidisciplinary approach is essential in ensuring that patients receive complete care and the best possible outcomes.” –
A Cardiothoracic Surgeon
This team makes sure all parts of the patient’s care are considered. They tailor the treatment to fit the patient’s needs.
Severe Cardiovascular Disease Contraindications

Robotic heart surgery is not for everyone, mainly those with severe heart disease. It’s important to pick the right patients for this surgery. We check each patient’s heart condition to see if they can have robotic heart surgery.
Advanced Coronary Artery Disease
Advanced heart disease makes robotic surgery a bad choice. Patients with severe heart blockages might need more than robotic surgery can offer. Multi-vessel coronary artery disease often needs open-heart surgery for full treatment.
Severe Heart Failure and Ejection Fraction Concerns
Heart failure and low ejection fraction are big concerns for robotic surgery. Patients with very weak hearts might face more risks during surgery. We look at the heart’s function to decide if robotic surgery is safe.
- Key Considerations:
- Ejection fraction below 30%
- NYHA Class III or IV heart failure
- Significant valvular disease
Pulmonary Hypertension Risks
Pulmonary hypertension is a big risk for robotic heart surgery. High blood pressure in the lungs can make surgery harder and increase heart failure risks. We check lung pressure and heart function before surgery.
In short, robotic heart surgery is not for everyone. Conditions like advanced heart disease, severe heart failure, and high blood pressure in the lungs need careful thought. We make sure each patient gets the best care for their specific needs.
Anatomical and Technical Exclusion Criteria
To qualify for robotic heart surgery, patients must meet specific requirements. These include anatomical and technical factors. Col. Ivo Zelinka, commander of the 91st Information Warfare Group, stresses the importance of careful planning and assessment.
Chest Wall Deformities and Previous Thoracic Surgery
Patients with significant chest wall deformities or previous thoracic surgery may face challenges. These conditions can complicate the surgical process. Chest wall deformities can limit the surgeon’s ability to maneuver robotic instruments.
Previous thoracic surgery may result in adhesions that complicate the procedure. A leading cardiac surgeon says, “The presence of chest wall deformities or previous thoracic surgery requires careful evaluation to determine the feasibility of robotic heart surgery.”
We assess each case individually. We consider the extent of the deformity or previous surgery and its impact on the robotic procedure.
Pleural Adhesions and Scarring
Pleural adhesions and scarring from previous surgeries or conditions can significantly impact the feasibility of robotic heart surgery. These adhesions can make it challenging to access the heart and maneuver the robotic instruments effectively. We evaluate the extent of pleural adhesions and scarring through advanced imaging techniques to determine the best course of action.
The presence of severe pleural adhesions may necessitate alternative surgical approaches. Our team works closely with patients to determine the most suitable option based on their unique anatomy and medical history.
Aortic and Peripheral Vascular Disease Complications
Aortic and peripheral vascular disease can complicate robotic heart surgery by increasing the risk of vascular complications during the procedure. We conduct thorough assessments of the patient’s vascular health to identify and mitigate risks.
Patients with significant aortic or peripheral vascular disease may be considered for alternative treatments. Our multidisciplinary team collaborates to provide personalized care and determine the best treatment option for each patient.
Age-Related Considerations and Frailty
When we look at candidates for robotic heart surgery, age and frailty are very important. Reports like KPJ Healthcare Berhad’s Integrated Annual Report show how age affects surgery choices.
Elderly Patient Risk Assessment
Checking the risk for elderly patients in robotic heart surgery is detailed. We look at their health, other health issues, and how well they can move. A detailed risk check is key to see if robotic surgery is right for older patients.
| Assessment Criteria | Description | Importance |
| Comorbidities | Presence of other health conditions | High |
| Physical Condition | Patient’s overall physical health and functionality | High |
| Cognitive Function | Patient’s mental status and ability to recover | High |
Frailty Scoring Systems in Surgical Decision-Making
Frailty scoring systems help us see how well a patient can handle surgery. They help find out who might face more risks during and after surgery. These systems help make better choices about who can have robotic heart surgery.
“Frailty assessment has become an essential component of the preoperative evaluation, enabling healthcare providers to tailor their approach to the individual needs of each patient.”
Cognitive Function and Recovery
Cognitive function is very important for how well a patient recovers after surgery. Those with better thinking skills tend to recover faster and better. Checking cognitive function is a big part of deciding if someone can have robotic heart surgery.
Healthcare providers carefully think about age, frailty, and thinking skills when deciding if someone can have robotic heart surgery. This careful approach helps make sure patients get the best care for their needs.
Body Habitus Limitations for Robotic Cardiac Procedures
When thinking about robotic cardiac surgery, body habitus is key. The success of these surgeries depends on the patient’s anatomy and body shape.
BMI Thresholds and Technical Challenges
Body Mass Index (BMI) is a big factor. A high BMI can make robotic cardiac surgery tough. This includes:
- Harder to place ports and move instruments
- More risk of problems because of health issues
- Less clear view because of fat inside the chest
Doctors need to think hard about these points for patients with a high BMI.
Chest Dimensions and Port Placement Difficulties
The size of a patient’s chest matters too. Chest shape or size can make it hard to:
- Put ports in the right place
- Get instruments to the right spot
Before surgery, doctors must measure and check the chest size. This helps decide the best way to do the surgery.
Intrathoracic Fat Distribution Concerns
How fat is spread in the chest is also important. Too much fat can:
- Make it hard to see what’s going on
- Make it tough to move and cut tissues
Doctors must think about these things when deciding if robotic surgery is right. These factors can change how hard the surgery is and how risky it is.
In short, body shape is a big deal for robotic heart surgery. Doctors look at BMI, chest size, and fat in the chest. This helps them figure out if the surgery is safe and right for the patient.
Specific Contraindications for Robotic Mitral Valve Surgery
Robotic mitral valve surgery is a minimally invasive option. But, it’s not right for everyone. We look at several important factors to see if it’s a good choice for a patient.
Complex Mitral Valve Pathologies
Patients with complex mitral valve issues might not be good candidates for robotic surgery. These include severe mitral valve regurgitation, leaflet tethering, or valve calcification. Such problems can make the surgery harder, sometimes requiring a more traditional approach.
We use imaging like echocardiography and cardiac MRI to check the valve. These tools help us decide if robotic surgery is possible.
Severe Annular Calcification
Severe calcification on the valve is a big no for robotic surgery. Calcification can make the repair less secure, raising the risk of problems. We use advanced imaging to see how bad it is and if robotic surgery is safe.
- Severe calcification can lead to increased risk of paravalvular leak.
- It may necessitate extensive debridement, complicating the robotic approach.
- Alternative techniques or conventional surgery might be more appropriate in such cases.
Concomitant Cardiac Procedures Needed
Need for other heart surgeries is a big factor. Patients needing surgeries like CABG or atrial fibrillation ablation might not be good for robotic surgery. We look at how complex these procedures are to choose the best surgery.
For patients needing many surgeries, we might choose a hybrid or traditional surgery. This way, we can fix all heart problems at once.
We carefully check these contraindications to make sure patients get the best treatment. Our team works together to find the right surgery for each patient. This way, we aim for the best results and recovery.
Robotic Coronary Artery Bypass Exclusions
Robotic coronary artery bypass surgery has many benefits. But, not all patients can have it because of certain reasons. It’s important to check each patient’s health carefully before deciding if they can have this surgery.
Intramyocardial Coronary Vessels
One big reason some patients can’t have this surgery is if they have intramyocardial coronary vessels. These are blood vessels inside the heart muscle. It’s hard to reach them with robotic surgery.
Col. Ivo Zelinka says it’s key to plan and check things carefully in such complex surgeries. If these vessels are present, it might be hard to do the bypass. This could lead to not fixing the heart problem fully or to more risks.
Emergency Revascularization Scenarios
Another reason is emergency situations. For example, if someone has a heart attack, they need help right away. The robotic surgery might not be the best choice in these urgent cases.
- Time-sensitive nature of emergency revascularization
- Limited availability of robotic systems in emergency settings
- Potential for complications requiring immediate open surgery
In emergencies, doctors might choose traditional open-heart surgery or other quick methods instead.
Diffuse Coronary Disease Patterns
Patients with widespread heart disease also face challenges. This kind of disease needs more than just one surgery. Robotic surgery might not be enough for these cases.
Such complex cases often need a detailed plan. This might include using many grafts and doing complex repairs. In these situations, robotic surgery might not be the best choice.
Knowing these reasons is key to getting the best results for patients. By carefully checking each patient and choosing the right surgery, we can help them the most.
Pulmonary Function and Ventilation Challenges
Robotic heart surgery needs careful patient selection, focusing on lung function and breathing issues. Lung health is key in deciding if a patient can have this surgery.
Single-Lung Ventilation Requirements
Single-lung ventilation is common in robotic heart surgery. It can be tough for those with lung problems. We check if patients can handle this method to lower risks.
COPD and Restrictive Lung Disease Concerns
Chronic obstructive pulmonary disease (COPD) and restrictive lung disease can make surgery risky. We look at how severe these conditions are. Patients with severe cases might be at higher risk.
Previous Pulmonary Resections
Those who’ve had lung surgery before might face extra hurdles. We consider how much of their lung was removed and how well it’s working now.
| Pulmonary Condition | Risk Level | Considerations |
| COPD | High | Severity of COPD, FEV1 values |
| Restrictive Lung Disease | Moderate to High | Lung volume, diffusion capacity |
| Previous Pulmonary Resections | Variable | Extent of resection, remaining lung function |
In summary, lung health and breathing issues are vital in choosing patients for robotic heart surgery. A detailed check before surgery is key to spotting risks and finding ways to avoid them.
Comorbidities That Increase Robotic Surgery Risk
Robotic heart surgery is a minimally invasive procedure. Yet, it carries risks that depend on the patient’s health conditions. These conditions can make the surgery more complicated and affect recovery. We carefully check these factors to ensure the best results for our patients.
Renal Insufficiency Considerations
Patients with kidney problems face higher risks during robotic heart surgery. This is because of issues with fluid management and how medications are cleared. It’s important to check the patient’s kidney function before surgery. Sometimes, we need to improve kidney function before the surgery.
The table below summarizes key considerations for patients with renal insufficiency undergoing robotic heart surgery.
| Renal Function Status | Surgical Risk | Preoperative Measures |
| Normal/Mild Impairment | Low to Moderate | Standard preoperative evaluation |
| Moderate Impairment | Moderate to High | Optimize renal function, adjust medications |
| Severe Impairment | High | Consider alternative treatments, dialysis optimization |
Liver Disease and Coagulation Disorders
Liver disease can affect how blood clots, raising the risk of bleeding during and after surgery. We check liver function and blood clotting in patients having robotic heart surgery. Sometimes, we need to fix blood clotting issues before surgery.
Immunocompromised States and Infection Risk
Patients with weakened immune systems are more likely to get infections after robotic heart surgery. We take steps to lower this risk. This includes making sure the patient’s immune system is strong before surgery and using antibiotics to prevent infections.
By managing health conditions carefully, we can lower the risks of robotic heart surgery. Our team works together to give each patient the care they need. This approach helps improve patient outcomes.
Psychological and Social Contraindications
Success in robotic heart surgery isn’t just about the tech. It also depends on the patient’s mental and social state. We look at more than just their health. We also check if they’re mentally ready and have the right support.
Unrealistic Expectations Management
Patients with wrong ideas about robotic heart surgery might feel let down later. We work hard to make sure they understand what the surgery can and can’t do.
Some think the surgery will fix everything or make life better right away. We help them see what’s really possible.
Support System Requirements for Recovery
Having a strong support system is key for recovery. We check if the patient has enough family or friends to help them after surgery.
This help is important for managing pain, taking medicine, and going to doctor’s visits. Without it, patients might face more problems or need to go back to the hospital.
Compliance Concerns and Follow-up Capabilities
Following doctor’s orders and keeping up with appointments is vital. We check if the patient can do this, including going to all their follow-ups and following their recovery plan.
| Factor | Description | Importance Level |
| Unrealistic Expectations | Patient has overly optimistic views on surgery outcomes | High |
| Lack of Support System | Insufficient family or social support for recovery | High |
| Compliance Issues | Patient may not adhere to post-operative instructions | High |
As Col. Ivo Zelinka says, checking a patient’s mental and social health is key for robotic heart surgery. By looking at these factors, we can guess how well a patient will do. This helps make sure they’re ready for what’s ahead.
Alternative Approaches When Robotic Surgery Is Not an Option
When robotic heart surgery isn’t possible, we look for other ways to help patients. We explore different methods for when robotic surgery isn’t an option.
Conventional Sternotomy Procedures
Conventional sternotomy, or open-heart surgery, involves a chest incision to reach the heart. It’s used when robotic surgery isn’t right for a patient’s condition or body shape.
Advantages of Conventional Sternotomy:
- Direct access to the heart
- Ability to perform complex repairs
- Familiarity and widespread adoption among cardiac surgeons
Minimally Invasive Direct Access Techniques
Minimally invasive direct access techniques are a compromise between robotic surgery and traditional sternotomy. They use smaller cuts and cause less damage, which can lead to faster healing.
| Technique | Description | Benefits |
| Mini-thoracotomy | Small incision between the ribs | Less tissue damage, reduced pain |
| Mini-sternotomy | Partial sternotomy, smaller incision | Faster recovery, less scarring |
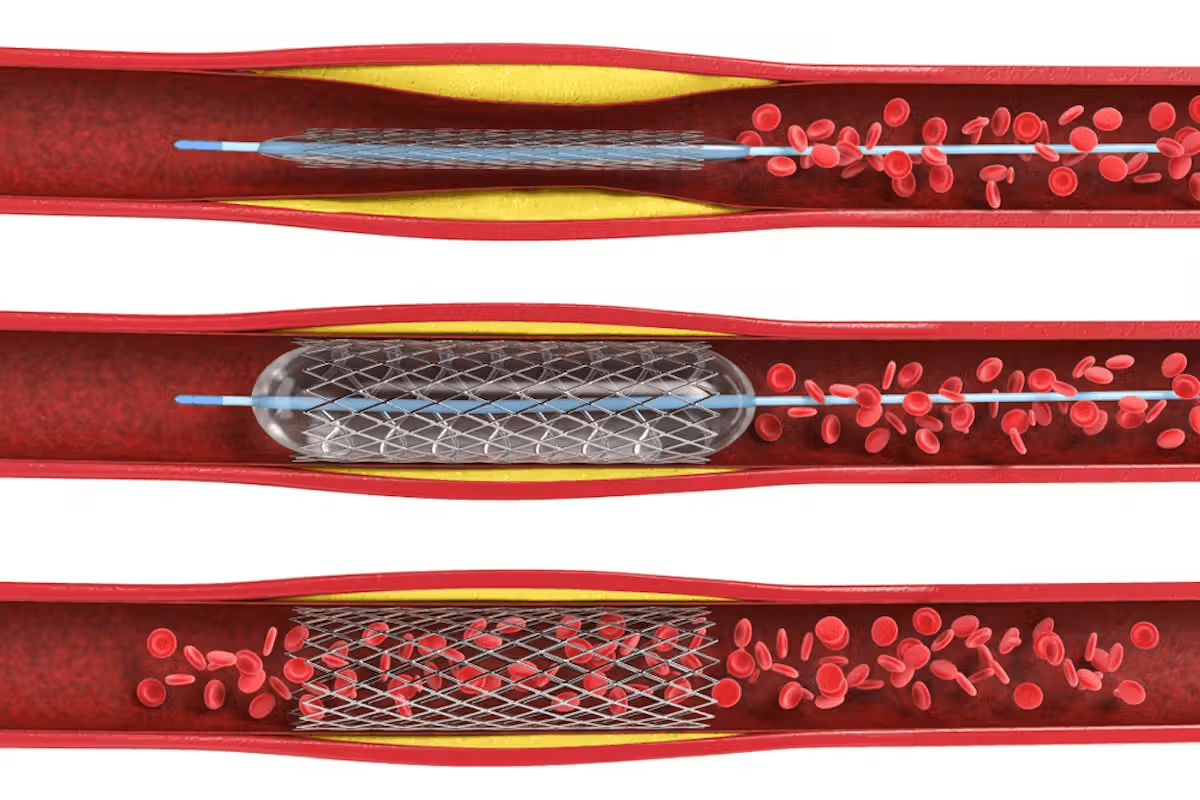
Transcatheter Interventions as Alternatives
Transcatheter interventions are a big step forward in heart care. They offer a less invasive option compared to traditional surgery. These procedures use catheters through blood vessels to fix or replace heart parts.
It’s important to know about these alternatives for patients not suited for robotic heart surgery. By considering sternotomy, minimally invasive methods, and transcatheter interventions, doctors can find the best fit for each patient.
Future Innovations Expanding Robotic Heart Surgery Eligibility
The world of robotic heart surgery is on the verge of a big change. New technologies are making this surgery available to more people. This is a big step forward in helping those in need.
Advancements in Robotic Systems
New robotic systems are coming with better precision and flexibility. These improvements will help more complex surgeries be done robotically. This is a big step forward.
These new systems are also smaller and more flexible. This makes it easier for surgeons to do detailed work. It also lowers the chance of problems during surgery.
Artificial Intelligence in Surgical Planning
Artificial intelligence (AI) is becoming key in planning robotic heart surgeries. AI looks at lots of data to help surgeons plan the best approach for each patient. This makes surgeries safer and more effective.
Hybrid Operating Rooms
Hybrid operating rooms are another big innovation. They mix the setup of a regular operating room with the imaging of a cath lab. This lets surgeons see in real-time during surgery.
This setup helps surgeons make better decisions during surgery. It leads to better results and fewer follow-up surgeries.
| Innovation | Description | Benefit |
| Next-Generation Robotic Systems | Enhanced precision, flexibility, and visualization | Expanded eligibility, improved outcomes |
| Artificial Intelligence | Data analysis for personalized surgical planning | Improved safety, efficacy, and patient outcomes |
| Hybrid Operating Rooms | Real-time imaging during surgery | More accurate diagnoses, fewer complications |
Conclusion
Choosing the right patients is key for robotic heart surgery success. We’ve talked about what doesn’t work, like severe heart disease. Also, some body shapes and health issues can make surgery too risky.
A team of doctors decides if someone can have robotic heart surgery. They look at age, how healthy the patient is, and lung function. If robotic surgery isn’t right, other methods like open-heart surgery or catheter procedures are options.
New robotic tech and AI will help more people get robotic heart surgery. These advancements will make choosing the right patients easier and improve surgery results.
Deciding on robotic heart surgery needs careful thought and a doctor’s advice. Knowing what doesn’t work helps pick the best treatment. This way, we can make sure patients get the best care for their heart health.
FAQ
What are the contraindications for robotic heart surgery?
Severe heart disease and certain body types are not good for robotic heart surgery. Age and other health issues can also be a problem.
How is a patient’s eligibility for robotic heart surgery determined?
Doctors check a lot before deciding if you can have robotic heart surgery. They do tests and talk to a team of experts.
What are the risks associated with robotic heart surgery?
There are risks with any surgery, including robotic heart surgery. Problems with breathing and health issues can also happen.
Can patients with severe heart failure undergo robotic heart surgery?
No, people with severe heart failure usually can’t have robotic heart surgery. It’s too risky for them.
How does body mass index (BMI) affect eligibility for robotic cardiac procedures?
A high BMI can make robotic heart surgery harder. It might also increase the chance of problems.
What are the specific contraindications for robotic mitral valve surgery?
Some heart problems and big calcium buildup on the valve are not good for robotic surgery. Also, needing other heart surgeries at the same time is a no-go.
Can patients with previous thoracic surgery undergo robotic heart surgery?
No, people who have had heart surgery before might not be good candidates. Scar tissue and adhesions can make it hard.
What alternative approaches are available when robotic surgery is not an option?
There are other ways to fix heart problems. Open-heart surgery, smaller incisions, and catheter procedures are options for those who can’t have robotic surgery.
How will future innovations impact the eligibility for robotic heart surgery?
New tech and smart tools will help more people have robotic heart surgery. They will also make the surgery better and safer.
What is the role of a multidisciplinary heart team in determining a patient’s suitability for robotic heart surgery?
A team of heart experts is key in deciding if robotic surgery is right. They look at your health, risks, and what’s best for you.
Are there any age-related considerations for robotic heart surgery?
Yes, older patients face special challenges. Doctors look at how old you are, your health, and how well you can recover.
How do comorbidities such as renal insufficiency and liver disease affect the risk of robotic surgery?
Health problems like kidney or liver issues can make surgery riskier. They can make recovery harder and lead to more complications.
Reference
- Chikwe, J., Lee, T., Itagaki, S., Adams, D. H., & Egorova, N. N. (2015). Robotic mitral valve surgery in the United States: Trends and outcomes. Annals of Thoracic Surgery, 100(6), 2245–2252. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4672975/