Last Updated on November 27, 2025 by Bilal Hasdemir

At Liv Hospital, we know that radiation therapy is key in fighting cancer. It brings hope and healing to people all over the world. The success of radiation tumor treatment depends on many things. These include the cancer type and stage, and the patient’s health. Many patients often ask, what is the maximum number of radiation treatments they can safely receive — and this depends on their individual condition and treatment goals.
The number of radiation treatments needed varies for each patient. Our team of experts works with patients to find the best treatment plan. They consider the patient’s unique situation and the latest in cancer treatment radiation.
Key Takeaways
- The maximum number of radiation treatments is not universally fixed.
- Treatment depends on tumor type, disease stage, and patient health.
- Radiation therapy can cure cancer, prevent its return, or slow its growth.
- Personalized treatment plans are key to effective cancer care.
- Liv Hospital is dedicated to top-notch cancer treatment.
Understanding Radiation Therapy in Cancer Treatment

We use radiation therapy to fight cancer, targeting and destroying cancer cells. It’s a local treatment that focuses on a specific area of the body. This makes it very effective for many types of cancer.
Definition and Basic Principles
Radiation therapy uses high-energy particles or waves to harm cancer cells’ DNA. This stops them from growing or kills them. It can be given from outside the body with external beam radiation therapy or from inside with brachytherapy. Sometimes, it’s given all over the body with systemic radiation therapy.
The choice of how to give radiation therapy depends on the cancer type, stage, and the patient’s health. The goal is to hit the tumor hard while keeping healthy tissues safe. This is done with careful planning and advanced techniques.
Role in Modern Oncology
Radiation therapy is key in modern cancer treatment, used in about 50% of cases. It can be used alone or with other treatments like surgery and chemotherapy. Its flexibility makes it valuable in both treating and easing symptoms of cancer.
In treatments aiming for a cure, radiation therapy tries to get rid of the tumor. In palliative care, it helps manage symptoms like pain and breathing problems. This improves life quality for those with advanced cancer.
Understanding radiation therapy helps us see its importance in cancer care. As cancer treatment keeps improving, radiation therapy’s role is more vital than ever. It brings hope and healing to patients all over the world.
What Is the Maximum Number of Radiation Treatments?

The number of radiation treatments for cancer varies. It depends on the cancer’s size, location, type, and the patient’s health. Each case is unique.
Variability Based on Cancer Type
Different cancers react differently to radiation therapy. Some cancers need fewer treatments because they are more sensitive. Others require more intense therapy. We adjust targeted radiation therapy for each cancer type to get the best results.
Cancers like Hodgkin’s lymphoma and some leukemia types often get radiation therapy. The number of treatments depends on the cancer’s stage and spread.
Impact of Disease Stage on Treatment Quantity
The cancer’s stage at diagnosis affects treatment length. Early-stage cancers might need fewer treatments. But advanced cancers may require more therapy to control symptoms or shrink tumors.
We make a treatment plan for each patient. We balance treating the tumor with avoiding side effects.
Patient-Specific Factors Affecting Treatment Limits
Each patient’s health, age, and past treatments also matter. We look at these factors to find the best treatment plan. This ensures the benefits of radiation therapy are greater than the risks.
Some patients get up to 10 radiation therapy courses over the years. But most treatments happen in a single course over weeks. Our aim is to treat effectively while keeping side effects low and quality of life high.
Common Radiation Therapy Regimens
Radiation therapy plans are made just for each patient. They can last different lengths of time and happen at different rates. Every patient’s situation is different, so their treatment plans are too.
We look at many things when planning a treatment. This includes the cancer type and stage, and the patient’s health. This way, we can make the treatment work best and reduce side effects.
Single Course Treatments
Most treatments are done in one go, with sessions over weeks. This method works well for tumors that are in one place.
Standard Fractionation: Treatments usually happen every weekday for 5 to 8 weeks. This method gives a strong dose of radiation while letting normal tissues heal.
Multiple Course Scenarios
Some patients need more than one round of treatment. This might happen if the cancer comes back or if a new tumor appears.
Re-treatment Considerations: When thinking about a second treatment, we look at the first plan, how the tumor reacted, and the patient’s current health. This helps us figure out the best next steps.
Extended Treatment Timelines
Some treatments take longer because of the cancer’s complexity or spread.
The table below shows some common treatment plans and their details:
| Treatment Type | Duration | Frequency |
| Single Course | 5 to 8 weeks | Daily, Mon-Fri |
| Multiple Courses | Varies | Dependent on initial treatment and recurrence |
| Extended Timeline | Several months | Intermittent or continuous |
Knowing about different treatment plans helps us tailor them to each patient. Our aim is to give the best treatment and keep the patient’s quality of life high.
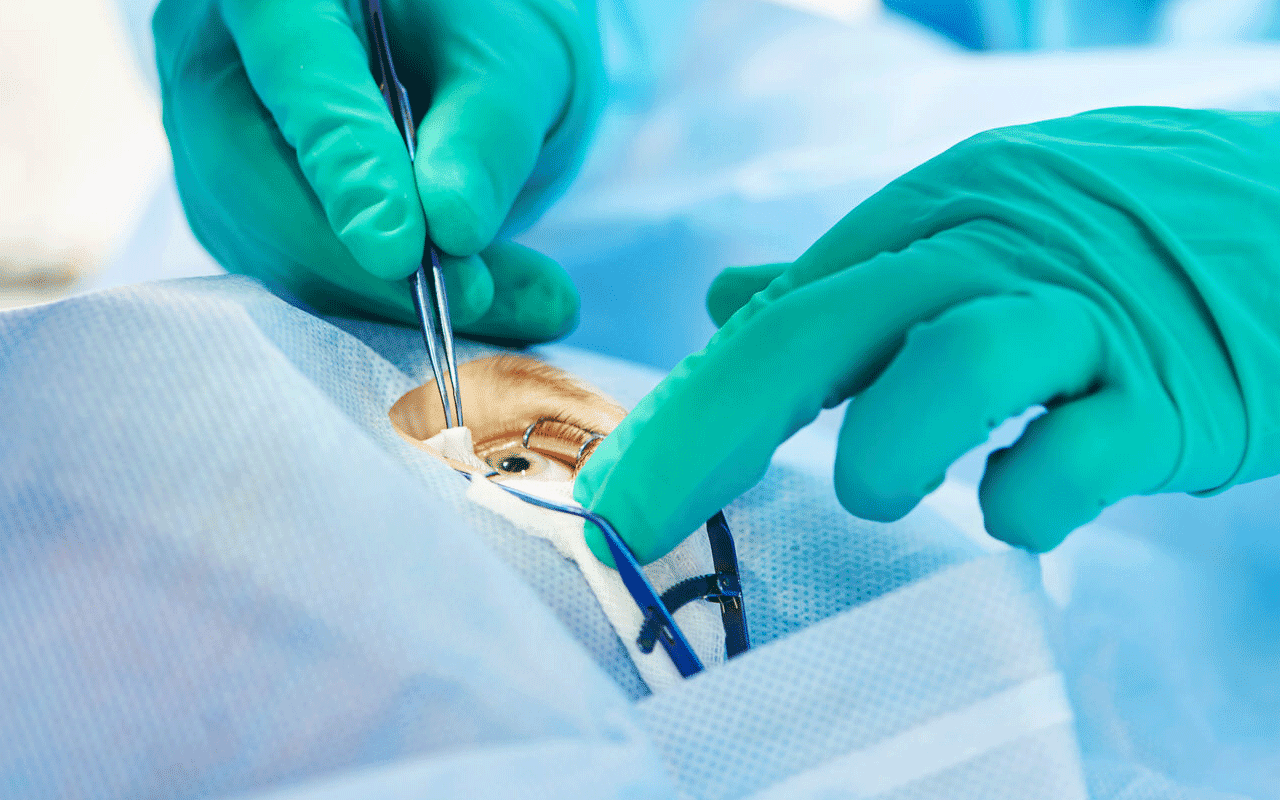
Types of Radiation Delivery Methods
Cancer treatment through radiation uses several methods. Each has its own benefits and uses. We choose the best method for each patient to fight cancer effectively.
External Beam Radiation Therapy
External Beam Radiation Therapy (EBRT) is the most common method. It uses a machine to send high-energy rays at the tumor from outside. This method targets cancer cells well while protecting healthy tissue. EBRT treats many cancers, like those in the brain, breast, lung, and prostate.
Dr. Jane Smith, a top oncologist, says, “External Beam Radiation Therapy has changed cancer treatment. It’s non-invasive and very effective in targeting tumors.” This method is key in modern oncology, giving hope to many patients.
Internal Radiation (Brachytherapy)
Brachytherapy puts radioactive material inside or near the tumor. This method gives high doses of radiation to cancer cells while protecting healthy tissue. It’s used for cancers of the prostate, cervix, and breast.
- Permanent implants: Small radioactive seeds are left in place permanently.
- Temporary implants: Radioactive material is placed near the tumor for a specific period, then removed.
Systemic Radiation Treatments
Systemic radiation therapy uses radioactive substances given orally or by injection. These substances travel through the body, targeting cancer cells. This method is great for treating cancers that have spread. It includes radioactive iodine for thyroid cancer and radiopharmaceuticals for certain metastatic diseases.
We keep improving in radiation oncology, bringing new treatments that help patients more. By knowing the different radiation methods, we can make treatment plans that fit each patient’s needs.
The Science of Radiation Tumor Treatment
Radiation therapy targets cancer cells with precise radiation. This damages their DNA, stopping them from growing. It’s a key part of modern cancer treatment, helping many patients.
Mechanism of Action on Cancer Cells
Radiation therapy works by harming cancer cells’ DNA. This causes them to die or stop growing. It’s vital for controlling tumors and shrinking them.
Key aspects of how radiation therapy works on cancer cells include:
- DNA damage leading to cell death or inhibition of cell division
- Targeted approach to minimize damage to surrounding healthy tissues
- Ability to be used in conjunction with other cancer treatments, such as surgery and chemotherapy
Experts say, “Radiation therapy is a critical part of cancer treatment.” It helps many patients, showing its importance.
Radiation Dosimetry
Radiation dosimetry is key to delivering the right amount of radiation. It plans and delivers doses based on each patient’s needs. This ensures the tumor gets enough radiation while protecting healthy tissues.
The goals of radiation dosimetry include:
- Maximizing the dose to the tumor to achieve optimal tumor control
- Minimizing the dose to surrounding healthy tissues to reduce side effects
- Ensuring that the treatment is delivered accurately and reproducibly
This helps make radiation therapy more effective and improves patient results.
Treatment Planning and Protocols
Effective radiation therapy starts with careful treatment planning. Each plan is made just for the patient. This makes sure the treatment works well and is safe, protecting healthy tissues.
“The goal of radiation therapy is to deliver a precise dose of radiation to the tumor while sparing normal tissues,” says the importance of personalized treatment planning. We use advanced imaging and sophisticated systems to make this happen.
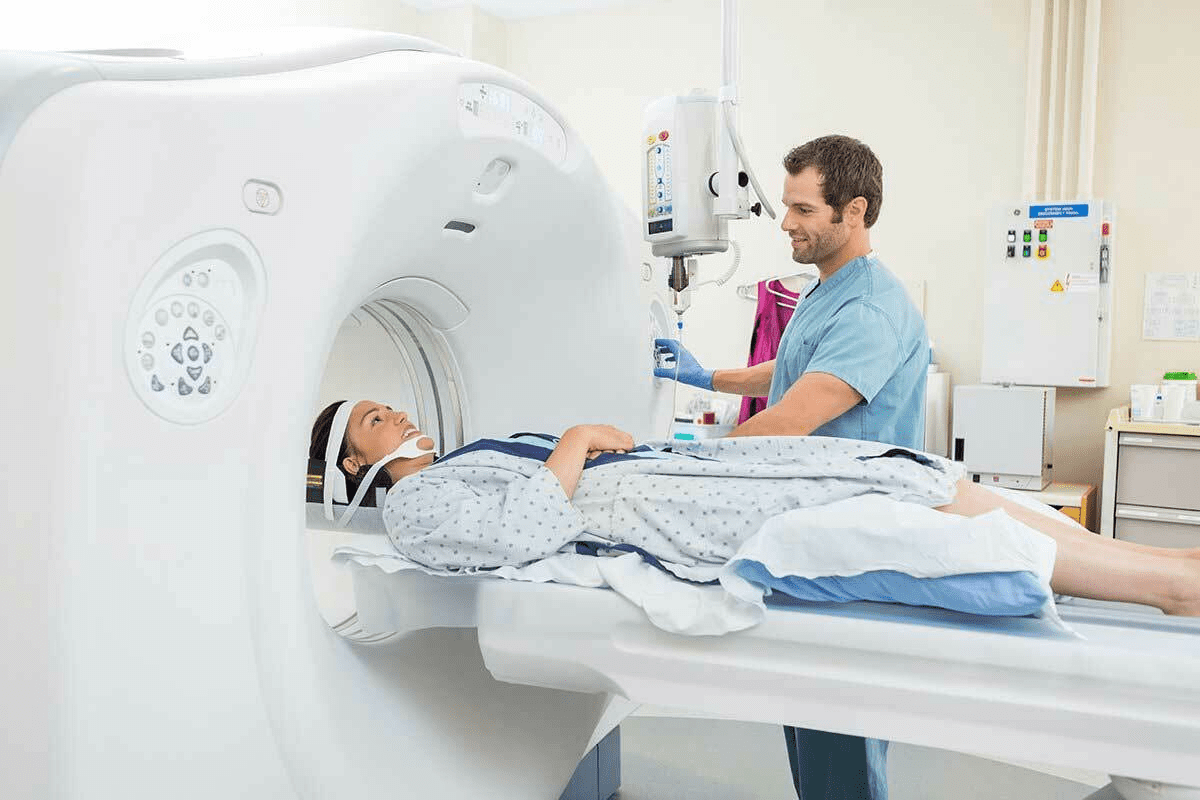
Initial Assessment and Imaging
The first step is a detailed check of the patient’s condition. We look at the tumor’s type, size, and where it is. We use CT, MRI, and PET scans to get detailed info.
These scans help us accurately pinpoint the tumor and avoid harming nearby tissues. The data we collect is key to figuring out the best radiation dose and how to deliver it.
Creating Personalized Treatment Plans
With the scan data, we make a treatment plan just for the patient. We pick the right radiation type, total dose, and how often to give it. We make sure the treatment hits the tumor right on target.
Our team of experts works together to plan the treatment. They balance treating the tumor with avoiding side effects. “Treatment regimens such as fractionation help minimize harm to normal tissue,” they say, showing the plan’s importance.
Monitoring and Adjusting Throughout Treatment
We keep a close eye on how the patient is doing during treatment. If needed, we will change the plan. This might mean adjusting the dose or how it’s given.
Being flexible with treatment plans helps us get better results and fewer side effects. We aim to give the best care possible. We want each patient to get a plan that fits their unique situation.
Fractionation Strategies in Radiation Therapy
Fractionation is key in radiation therapy. It helps deliver effective doses safely. By breaking the dose into smaller parts, we protect healthy tissues better.
Standard Fractionation Approaches
Standard fractionation gives a dose of 1.8 to 2 Gy per fraction, once a day, five days a week. It’s chosen for its good balance of fighting tumors and protecting normal tissues.
Top radiation oncologists say standard fractionation is a mainstay. It’s great because it fights tumors well while keeping normal tissues safe. The main benefits are:
- Less risk of late side effects
- Better tumor control
- Healthier normal tissues
Hypofractionation Benefits and Limitations
Hypofractionation gives higher doses in fewer fractions. It’s popular for some tumors because it might fight them better and is quicker for patients.
| Benefits | Limitations |
| Shorter treatment time | More risk of side effects |
| Could fight tumors better | Not for all tumors |
| Patients like it better | Needs careful aim to avoid healthy tissues |
Hyperfractionation Applications
Hyperfractionation gives many small fractions a day, with a lower dose each time. It tries to use the repair differences between tumors and healthy tissues.
“Hyperfractionation has shown promise in improving tumor control while reducing late toxicity, particular in head and neck cancers.”
The good things about hyperfractionation are:
- Better tumor control
- Less risk of late side effects
- Better treatment ratio
In conclusion, fractionation is vital in radiation therapy. It offers different ways to treat patients based on their needs and tumor types. Knowing the pros and cons of each method helps us give better care.
Curative vs. Palliative Radiation Approaches
Radiation therapy in cancer treatment falls into two main types: curative and palliative. Each type has its own goals and methods. Knowing the difference is key to good treatment planning and patient care.
Goals and Protocols for Curative Treatment
Curative radiation therapy aims to get rid of cancerous tumors. Its main goal is to cure the patient or extend their life significantly. It’s used when cancer is in one place and can be treated with radiation. The treatment involves:
- Targeting the tumor precisely to harm cancer cells more
- Using careful dosing to protect healthy tissues
- Delivering high doses over time through fractionation
Curative radiation can be used alone or with surgery and chemotherapy. The choice depends on the cancer type, stage, and the patient’s health.
Palliative Radiation Strategies
Palliative radiation therapy aims to ease symptoms and improve life quality for those with advanced cancer. Its main goal is to reduce pain, bleeding, and other distressing symptoms. Strategies include:
- Short radiation courses to quickly ease symptoms
- Targeted treatment to lessen side effects and increase symptom relief
- Flexible dosing to fit the patient’s condition and needs
Palliative radiation can greatly improve a patient’s quality of life. It helps them stay independent and comfortable during treatment.
Transitioning Between Treatment Goals
In some cases, treatment goals may change from curative to palliative or vice versa. Good communication between the patient and healthcare team is vital during these changes. This ensures the treatment plan meets the patient’s evolving needs and goals.
Understanding radiation therapy’s different approaches helps patients and healthcare providers create a treatment plan that fits the patient’s needs. Whether the goal is curative or palliative, the plan should align with the patient’s specific goals.
Managing Side Effects During Multiple Treatments
Radiation therapy is a key cancer treatment, but it can cause side effects. It’s important to manage these effects well. This helps improve patient outcomes.
Common Acute Side Effects
Side effects from radiation therapy vary by treatment area. They often include fatigue, skin reactions, and pain. Fatigue is a big issue, affecting daily life and quality of life.
To fight fatigue, patients should eat well, drink plenty of water, and do light exercises. Taking care of the skin is also key. Use mild soaps, avoid harsh chemicals, and wear loose clothes to reduce skin reactions.
| Side Effect | Management Strategy |
| Fatigue | Balanced diet, hydration, and gentle exercises |
| Skin Reactions | Mild soaps, avoid harsh chemicals, loose clothing |
| Localized Pain | Pain management medication, rest |
Long-term Considerations
Long-term side effects can happen months or years after treatment. These include fibrosis, secondary cancers, and organ problems. Regular check-ups with healthcare providers are key to managing these effects.
Advances in radiation therapy, like IMRT and proton therapy, reduce long-term side effects. They deliver precise radiation to tumors, protecting healthy tissues.
Supportive Care During Extended Treatment
Supportive care is vital for managing radiation therapy side effects. It includes nutrition advice, psychological support, and symptom management. We create personalized care plans to help patients cope with treatment.
By understanding and managing radiation therapy side effects, we can greatly improve patients’ quality of life. This is true for those undergoing multiple treatments.
Advances in Targeted Radiation Therapy
Targeted radiation therapy is key in modern cancer treatment. It offers better results and fewer side effects. We’ve seen big steps forward, making treatments more precise and effective for patients.
Intensity-Modulated Radiation Therapy (IMRT)
Intensity-Modulated Radiation Therapy (IMRT) shapes radiation beams to fit a tumor’s shape. This lets us give more radiation to the tumor and less to healthy tissues. IMRT is great for treating complex tumors, like those in the head and neck.
Stereotactic Body Radiation Therapy (SBRT)
Stereotactic Body Radiation Therapy (SBRT) uses focused radiation beams on specific body areas. It’s good for tumors that don’t respond well to usual radiation. SBRT has shown great results for tumors in the lung, liver, and spine.
Proton Therapy and Particle Radiation
Proton therapy uses protons instead of X-rays to treat tumors. It’s even more precise, reducing damage to nearby tissues. Proton therapy is best for tumors near the brain or spinal cord. We’re looking into how particle radiation, like proton therapy, can help our patients.
These new methods in targeted radiation therapy have changed cancer treatment. They give us better and more precise ways to fight cancer. As we keep improving, we’re dedicated to giving our patients the best care.
Conclusion: Balancing Maximum Effectiveness with Patient Well-being
The number of radiation treatments for cancer isn’t the same for everyone. It depends on the cancer type, its stage, and the patient’s health. Our aim is to make sure treatments work well while keeping patients safe and comfortable.
Healthcare teams use the latest in radiation therapy to make plans that fit each patient. This is key to getting the best results without harming the patient.
Success in radiation therapy comes from careful planning and using the newest technology. This way, we can make treatments better and improve patients’ lives.
FAQ
What is radiation therapy, and how does it work?
Radiation therapy is a cancer treatment. It uses high-energy particles or waves to damage cancer cells’ DNA. This stops their growth or kills them. It’s a key part of cancer treatment, used in about 50% of cases.
How is the maximum number of radiation treatments determined?
The number of radiation treatments varies for each patient. It depends on the cancer type, stage, and the patient’s health. Knowing these factors helps plan the right treatment.
What are the different methods of delivering radiation therapy?
There are several ways to deliver radiation therapy. These include external beam, brachytherapy, and systemic treatments. Each method is used based on the cancer’s type and location.
What is fractionation in radiation therapy?
Fractionation is a strategy in radiation therapy. It delivers effective doses while protecting healthy tissues. There are different approaches, each with its own benefits and limitations.
What is the difference between curative and palliative radiation therapy?
Curative treatments aim to remove the cancer. Palliative treatments focus on easing symptoms and improving life quality. Knowing the goals of each is key to effective treatment planning.
How are side effects managed during radiation therapy?
Managing side effects is vital in radiation therapy. Understanding common side effects and how to reduce them is important. Supportive care plays a big role in improving outcomes.
What are the recent advances in radiation therapy?
Recent advances include new techniques like IMRT, SBRT, and proton therapy. These allow for better targeting of tumors and less damage to healthy tissues.
How does radiation therapy impact cancer cells?
Radiation therapy damages cancer cells’ DNA, causing them to die or stop growing. Ensuring the right amount of radiation is delivered is critical.
What is the role of treatment planning in radiation therapy?
Treatment planning is essential in radiation therapy. It involves assessing the patient, creating personalized plans, and making adjustments as needed.
Can radiation therapy be used in combination with other cancer treatments?
Yes, radiation therapy can be used alone or with other treatments like surgery and chemotherapy. The choice depends on the cancer type and stage.
How does the type and stage of cancer affect radiation therapy?
The cancer type and stage greatly influence the treatment plan. Different cancers and stages require specific approaches.
What is targeted radiation therapy?
Targeted radiation therapy targets specific cancer cells or tumors. It aims to minimize damage to healthy tissues.
References
- Mehta, S. R. (2011). Radiotherapy: Basic concepts and recent advances. Cancer Radiotherapy, 15(5), 285-296. https://pmc.ncbi.nlm.nih.gov/articles/PMC4920949/