
When a man has his prostate removed, his body changes a lot. The prostate gland is key to the male reproductive system. Its removal can cause different side effects.
Prostate surgery might seem scary, but it’s important to know. Side effects like urinary problems and erectile dysfunction can be treated. They might even get better with time.
Learning about the effects of prostate removal helps us understand its impact. It also shows us the treatments available.
Key Takeaways
- Prostate removal can lead to urinary issues and erectile dysfunction.
- These side effects can often be managed with treatment.
- Symptoms may improve over time.
- Understanding the prostate’s role is crucial for men considering or undergoing prostate removal.
- Various treatment options are available to manage side effects.
Understanding the Prostate and Its Functions
The prostate gland is key to the male reproductive system. It plays a big role in both urine and sex functions. Knowing what the prostate does is important for understanding prostate removal.
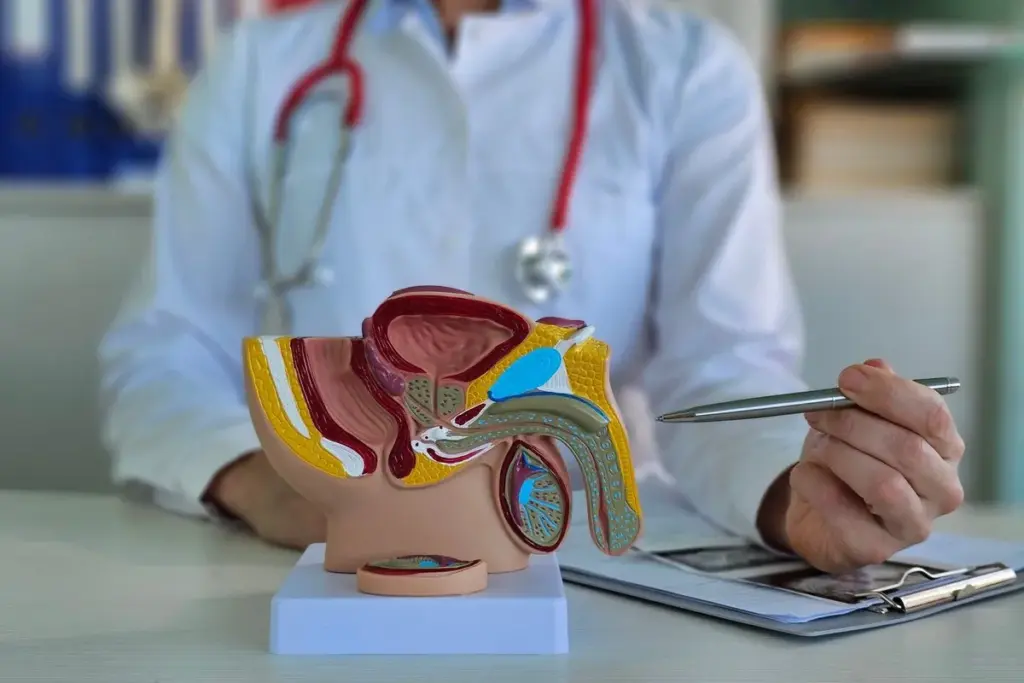
Anatomical Location and Structure
The prostate gland sits below the bladder and wraps around the urethra. It’s about the size of a walnut. It’s made of glandular tissue and muscle, helping with semen and urine control.
What Does Your Prostate Do?
The prostate makes seminal fluid, which feeds and protects sperm. This fluid is vital for fertility, helping sperm move during sex. The prostate’s muscles also help push semen out during ejaculation.
The Prostate’s Role in Male Reproductive Health
The prostate is more than just making seminal fluid. It helps create a good environment for sperm. Problems with the prostate can hurt fertility.
How the Prostate Affects Urinary Function
The prostate’s health affects urine flow. An enlarged prostate can block the urethra, causing weak flow and frequent urination. Knowing this helps diagnose and treat urinary problems linked to the prostate.
|
Prostate Function |
Description |
Impact on Health |
|---|---|---|
|
Seminal Fluid Production |
Produces fluid that nourishes and protects sperm |
Crucial for male fertility |
|
Urinary Control |
Surrounds the urethra, influencing urinary flow |
Affects urinary symptoms and comfort |
|
Ejaculatory Process |
Muscular component aids in propelling semen |
Essential for sexual function and fertility |
Reasons for Prostate Removal
Prostate removal surgery is needed for serious prostate issues. It’s a big step taken when other treatments don’t work or aren’t right.
Prostate Cancer as the Primary Indication
Prostate cancer is the top reason for prostate removal surgery. If you have prostate cancer, removing the prostate might be the first choice. This choice depends on the cancer’s stage and how fast it grows.
Advanced Benign Prostatic Hyperplasia (BPH)
Advanced BPH is another reason for prostate removal. BPH makes the prostate too big, causing bad urinary symptoms. If BPH is too severe and other treatments don’t help, surgery might be needed.
When Is Prostate Surgery Necessary?
Prostate surgery is needed when the prostate is badly affected by disease. This includes prostate cancer or severe BPH. The decision to operate depends on symptoms, quality of life, and overall health.
Alternatives to Complete Prostate Removal
There are other ways to treat prostate issues besides removing it. For prostate cancer, you might choose active surveillance, radiation, or focal therapy. For BPH, you could try medications or less invasive surgeries before removing the prostate.
It’s important to know why prostate removal is needed and what other options are available. We help patients make the best health choices based on their situation.
Types of Prostate Surgery Procedures
It’s important to know about the different prostate surgery types. Each procedure is designed to tackle specific prostate issues. This knowledge helps in making informed health decisions.
Radical Prostatectomy Explained
Radical prostatectomy removes the prostate gland, seminal vesicles, and surrounding tissue. It’s mainly for treating prostate cancer.
Simple Prostatectomy for Enlarged Prostate
Simple prostatectomy treats an enlarged prostate (BPH). It removes the inner prostate part blocking urine flow. It’s chosen when other BPH treatments don’t work.
Comparing Surgical Approaches and Success Rates
Prostatectomy uses open, laparoscopic, and robotic-assisted surgery. The choice depends on health, surgeon skill, and prostate condition. Success rates vary by procedure and case.
We look at recovery time, complication rates, and long-term results. Robotic-assisted surgery often means less blood loss and quicker recovery than open surgery.
The right prostate surgery depends on a thorough patient evaluation. It’s key to talk about each procedure’s benefits and risks with a healthcare provider.
Preparing for Prostate Removal Surgery
Getting ready for prostate removal surgery is a big step. It means understanding the surgery, making lifestyle changes, and getting mentally ready. We want to make sure you’re ready for the surgery and the recovery that follows.
Medical Evaluations and Pre-Surgical Tests
Before surgery, you’ll go through many medical tests. These tests check your health and look for any risks. You might have:
- Blood tests for infections or other health issues
- Imaging tests like MRI or CT scans to see the prostate and nearby tissues
- An electrocardiogram (ECG) to check your heart
- Urine tests for urinary tract infections
These tests help your doctors understand your situation. They plan the prostate removal surgery based on this information.
Lifestyle Adjustments Before Surgery
Changing your lifestyle before prostate cancer surgery can help your recovery. We suggest:
- Quitting smoking for better lung health and recovery
- Eating a healthy diet with lots of fruits, veggies, and whole grains
- Drinking plenty of water to stay hydrated
- Avoiding heavy lifting or hard activities
These changes can lower the risk of problems and improve your health.
Mental Preparation and Setting Realistic Expectations
Getting mentally ready for prostate removal is key. It’s important to know what to expect from the surgery and recovery. We recommend:
- Talking about your worries and fears with your doctor or a counselor
- Learning about the surgery’s possible results and side effects
- Setting achievable goals for your recovery and life after surgery
Being mentally prepared can greatly affect your recovery and happiness.
Questions to Ask Your Surgeon
Talking openly with your surgeon before surgery is crucial. You should ask questions like:
|
Category |
Questions |
|---|---|
|
Surgery Details |
What type of prostate removal surgery is best for me? What are the possible risks and complications? |
|
Recovery |
How long does recovery usually take? Are there special care instructions after surgery? |
|
Follow-up |
What kind of follow-up care will I need after surgery? How will my progress be checked? |
Asking these questions can make you feel more informed and ready for the surgery.
The Prostate Cancer Surgery Procedure
Radical prostatectomy is a detailed surgery for prostate cancer. It involves several key steps. These steps ensure the prostate gland and affected tissues are removed.
Anesthesia and Surgical Setup
The surgery starts with anesthesia to keep the patient comfortable. General anesthesia makes the patient unconscious. The patient is then positioned for the best access to the prostate gland.
Preparation is key for a successful surgery. This helps avoid risks and complications.
Step-by-Step Surgical Process
The surgery has several precise steps:
- Making an incision to access the prostate gland.
- Carefully dissecting the prostate from surrounding tissues.
- Removing the prostate gland and seminal vesicles.
- Reattaching the urethra to the bladder.
Nerve-Sparing Techniques
Nerve-sparing techniques are vital for preserving erectile function and urinary continence. Our surgeons use advanced techniques to identify and spare nerves around the prostate gland.
The choice to use nerve-sparing techniques depends on the cancer’s extent and the patient’s health. Preserving these nerves greatly impacts the patient’s recovery and quality of life post-surgery.
Duration and Immediate Post-Operative Care
The surgery’s duration varies, usually between 2 to 4 hours. After surgery, patients are closely monitored in the recovery room for any immediate complications.
|
Surgery Aspect |
Description |
Duration/Recovery |
|---|---|---|
|
Anesthesia |
General anesthesia for patient comfort |
Effects wear off post-surgery |
|
Surgical Process |
Removal of prostate and affected tissues |
2-4 hours |
|
Nerve-Sparing |
Techniques to preserve surrounding nerves |
Impacts recovery and quality of life |
Immediate post-operative care includes managing pain and monitoring for complications. Patients are also taught about post-surgery care and follow-up appointments.
Hospital Recovery After Prostate Removal
The time after prostate removal surgery is key. The recovery process focuses on effective pain management, re-establishing normal urinary functions, and regaining mobility. Knowing what to expect in the hospital is important.
Typical Hospital Stay Duration
How long you stay in the hospital can vary. It depends on your health and the surgery’s complexity. Usually, it’s 1 to 3 days.
Pain Management Protocols
Managing pain well is a big focus. We use medicines and other methods to keep you comfortable. Pain management protocols are made just for you.
One patient said, “The pain team really listened to me. I felt okay during my recovery.”
“I was surprised by how well-managed my pain was after surgery. The medical staff were very responsive to my needs.”
Catheter Use and Initial Urinary Management
A catheter is used right after surgery. It helps drain your bladder properly. We’ll talk about catheter use and how to manage your urine before your surgery.
|
Day |
Catheter Status |
Urinary Management |
|---|---|---|
|
1-2 |
In place |
Continuous drainage |
|
2-3 |
Removal considered |
Monitoring for urinary continence |
|
After discharge |
Removed |
Patient begins to regain urinary control |
First Steps Toward Mobility
Moving around early is good for you. Patients are encouraged to take their first steps with help from hospital staff, usually within 24 hours.
Knowing about the recovery process helps you prepare. Our team is here to support you during this important time.
Urinary Function Changes After Prostatectomy
Prostate removal surgery can cause various urinary problems. These can be short-term or last a long time. It’s important to know about these changes to manage your expectations and improve your outcome.
Temporary Urinary Incontinence: What to Expect
Many men experience temporary urinary incontinence after prostate surgery. They might leak urine when they cough, sneeze, or do physical activities. This usually gets better as the body heals.
Doing pelvic floor exercises, like Kegels, can help. These exercises strengthen the muscles that control urination. This can help reduce incontinence.
Long-term Urinary Control Issues
Some men may have long-term urinary problems after surgery. The extent of the surgery and how quickly you heal can affect this.
Talking to your healthcare provider about any ongoing issues is crucial. They can help find ways to manage these problems.
Rehabilitation Techniques for Urinary Function
Rehabilitation is key to getting back to normal urination. Techniques include:
- Pelvic floor physical therapy
- Biofeedback to improve bladder control
- Lifestyle changes, like what you eat
These methods can greatly improve your recovery. They can also lessen the severity of urinary incontinence.
Adaptive Products for Incontinence Management
There are many products to help manage incontinence. These include:
|
Product Type |
Description |
Benefit |
|---|---|---|
|
Absorbent Pads |
Disposable pads for leakage |
Discreet protection |
|
Catheter |
For urinary drainage |
Effective for severe incontinence |
|
Protective Underwear |
Special underwear for incontinence |
Comfort and confidence |
Choosing the right product depends on how severe your incontinence is and what you prefer.
Sexual Function After Prostate Removal
Prostate removal surgery can change a man’s sexual function a lot. It can lead to different effects that are hard to deal with. Understanding these changes and treatment options is key.
Erectile Dysfunction Following Surgery
Erectile dysfunction (ED) is a common side effect of prostate removal surgery. The risk and how bad it is can depend on many things. These include the surgery method, the patient’s age, and their sexual health before surgery. Using nerve-sparing techniques can help lower the risk of ED.
Dealing with ED can be tough, but there are ways to manage it. Treatments include medicines, vacuum devices, and implants. It’s important to talk to your doctor to find the best treatment for you.
Changes in Ejaculation and Orgasm
Prostate removal surgery can also change how men ejaculate and orgasm. Some men might have a condition called dry orgasm, where they don’t ejaculate much. This happens because the prostate and seminal vesicles, which make seminal fluid, are removed or changed.
The feeling of orgasm might also change. Some men might feel less intense orgasms, while others might not notice much of a difference. Knowing these changes can help men prepare and talk to their doctors about any worries.
Timeline for Sexual Recovery
How long it takes to recover sexually after prostate removal surgery varies. Things like age, health, and nerve damage during surgery can affect recovery. Most men will see some improvement in erectile function over time, especially with therapy.
It’s important to be patient and work with your doctor to track progress and adjust treatments as needed. Recovery is a slow process. Having realistic expectations can help men deal with the challenges they face.
Treatment Options for Sexual Dysfunction
There are many treatments for sexual dysfunction after prostate removal. These include:
- Medications like PDE5 inhibitors
- Vacuum erection devices
- Penile implants
- Counseling and sex therapy
Each treatment has its own benefits and drawbacks. It’s best to talk to your doctor to find the right treatment for you.
Physical Recovery Timeline After Prostate Surgery
The journey to recovery after prostate surgery has many stages. Each stage has its own challenges and milestones. Remember, everyone heals differently.
First Week After Surgery
The first week is key for a smooth recovery. You might feel pain, be tired, and have trouble with your urine. Always follow your doctor’s advice on pain, catheter care, and what activities to avoid.
Doctors usually tell patients to avoid heavy lifting and hard work. You might need to take time off work, depending on your job and health.
First Month of Recovery
In the first month, you might start to feel better. The catheter is often removed within a week. You’ll start to get back some control over your urine.
Some incontinence is common, but it gets better with time and exercises. You can start doing light exercises again, but check with your doctor first.
Three to Six Months After Surgery
Between three to six months, most men feel much better. This is when most of the recovery happens. Many regain full control over their urine and see big improvements in their life.
Some side effects like erectile dysfunction or incontinence might still be there. But they usually get better. Keep doing your exercises and see your doctor regularly.
Long-term Physical Adaptation
In the long run, most men adjust well to life after surgery. Some might still have side effects, but many see their quality of life improve.
|
Recovery Stage |
Typical Milestones |
Common Challenges |
|---|---|---|
|
First Week |
Initial recovery, pain management |
Discomfort, fatigue, urinary issues |
|
First Month |
Catheter removal, regaining urinary control |
Urinary incontinence, limited physical activity |
|
Three to Six Months |
Significant improvement, regaining urinary control |
Erectile dysfunction, urinary incontinence |
|
Long-term |
Adaptation to life after surgery |
Potential persistent side effects |
Keeping a healthy lifestyle is important. Eat well and exercise regularly. Regular check-ups with your doctor are also key to tracking your progress and solving any issues.
Psychological Impact of Prostate Removal
Removing the prostate gland can deeply affect a man’s mental health. This surgery, often for prostate cancer, brings emotional and psychological changes.
Body Image and Masculinity Concerns
Men may see changes in how they view their bodies and masculinity after surgery. The loss of the prostate can make them feel vulnerable or change their sense of self.
Some common worries include:
- Changes in urinary function and continence
- Impact on sexual function and intimacy
- Emotional adjustments to the loss of a part of their body
Depression and Anxiety After Surgery
Men often feel depressed and anxious after prostate removal surgery. The surgery’s stress and lifestyle changes can cause these feelings.
We know that:
- Depression can show as constant sadness or losing interest in things
- Anxiety can make people worry about the future, health, and relationships
Getting mental health support is very important during this time. Professional help can teach ways to handle these feelings and improve well-being.
Relationship Changes and Challenges
Prostate removal can also affect relationships, especially with partners. Changes in sexual function and intimacy can make it hard to keep a healthy relationship.
Being open and understanding is key. Couples might find it helpful to:
- Go to counseling to deal with emotional and physical changes
- Join support groups to share experiences and advice
Coping Strategies and Mental Health Support
There are ways to cope with the psychological effects of prostate removal. These include:
- Seeking professional mental health support
- Joining support groups
- Doing stress-reducing activities, like meditation or yoga
Keeping a positive outlook and seeking help when needed are key steps in facing the psychological challenges of prostate removal.
Life Expectancy After Prostate Removal
How long you live after having your prostate removed depends on several things. This includes the cancer’s stage when you’re diagnosed. Removing the prostate is a big surgery. It can change your life a lot.
Survival Rates for Prostate Cancer Patients
Thanks to new medical tech and treatments, more men are surviving prostate cancer. In the U.S., nearly all men with early-stage prostate cancer live for five years after diagnosis. This is according to the American Cancer Society.
We look at survival rates based on cancer stage:
|
Cancer Stage |
5-Year Survival Rate |
10-Year Survival Rate |
|---|---|---|
|
Localized |
100% |
98% |
|
Regional |
100% |
96% |
|
Distant |
31% |
17% |
Factors Affecting Long-term Outcomes
Many things can affect how well you do after prostate removal. These include your health, age, and the cancer’s stage and grade.
- Age and Overall Health: Older men or those with health issues might have different outcomes than younger, healthier men.
- Cancer Stage and Grade: How far the cancer has spread and how aggressive it is are key to long-term survival.
- Surgical Technique: The surgery method, like nerve-sparing, can affect recovery and long-term quality of life.
Quality of Life Considerations
After prostate removal, how well you feel is very important. The surgery can save your life but might change how you urinate and have sex.
Rehabilitation and support are crucial to improve your quality of life. Many men find help in pelvic floor physical therapy and other treatments to manage side effects.
Cancer Recurrence Risks and Monitoring
The chance of cancer coming back after prostate removal depends on several factors. These include the cancer’s initial stage and how clean the surgery was.
Regular PSA tests are key to catching cancer recurrence early. Knowing the risks and benefits of follow-up plans helps men make informed choices about their care.
Follow-up Care After Radical Prostatectomy
After a radical prostatectomy, it’s key to know about follow-up care. This care helps you recover well and stay healthy long-term. It includes regular medical visits and tests to check on your health and catch any problems early.
Regular Medical Check-ups Schedule
Regular visits to the doctor are vital after a radical prostatectomy. These visits include:
- Physical exams to check your health and look for any complications or cancer coming back.
- Looking over your medical history to talk about any side effects or concerns.
- Talking about how you’re doing and making changes to your care plan if needed.
At first, you’ll see your doctor often, like every few months. As you get better, these visits will become less frequent.
PSA Testing After Prostatectomy
PSA (Prostate-Specific Antigen) testing is a big part of follow-up care after prostate surgery. It checks if prostate cancer has come back. If PSA levels are not zero, it could mean cancer is back, and you might need more treatment.
PSA tests are done:
- Every 3-6 months for the first few years after surgery.
- Once a year if PSA levels stay zero.
Signs That Require Immediate Medical Attention
While you’re recovering, watch for signs of trouble. These signs mean you need to see a doctor right away. They include:
- Severe pain that can’t be controlled with medicine.
- Signs of infection, like fever, chills, or redness around the surgery site.
- Urinary problems, such as not being able to hold your urine or having trouble starting to urinate.
- Any other unusual symptoms or worries.
Long-term Monitoring Protocols
After surgery, you’ll keep getting PSA tests and seeing your doctor regularly. These visits might not be as often, but they’re still important. They help catch any late problems or cancer coming back.
Your doctor might also suggest:
- Changes in your lifestyle to help with side effects and stay healthy.
- Rehab programs to help with urinary and sexual issues.
Following a good follow-up care plan helps you recover well. It also helps you catch and deal with any problems early. This way, you can live a better life after your surgery.
Advances in Prostate Removal Techniques
New surgical techniques are changing prostate removal, making recovery better and side effects less. The field of prostate surgery has made big strides. This is thanks to research, new tech, and understanding what patients need.
Latest Surgical Innovations
New surgical methods are making prostate removal more precise and less invasive. Robotic-assisted surgery is becoming more common. It offers better results and faster recovery times. Robotic surgery lets surgeons do complex tasks with more accuracy.
Focal Therapy Options
Focal therapy is a big change in treating prostate cancer. It targets the cancer while keeping healthy tissue safe. This method can lower the risk of side effects from traditional surgery. Focal therapy is great for patients with localized cancer, offering a less invasive option.
|
Therapy Type |
Description |
Benefits |
|---|---|---|
|
Focal Laser Ablation |
Minimally invasive procedure using laser to destroy cancer cells |
Preserves surrounding tissue, reduces side effects |
|
High-Intensity Focused Ultrasound (HIFU) |
Non-invasive treatment using ultrasound waves to target cancer |
Minimal recovery time, reduced risk of incontinence |
|
Cryotherapy |
Procedure that freezes cancer cells, leading to their death |
Effective for localized cancer, minimal damage to surrounding tissue |
Research on Reducing Side Effects
Research is working to lessen side effects from prostate surgery. Studies are looking at new ways and tech to help with urinary and sexual issues after surgery. By figuring out why these problems happen, researchers can find better ways to fix them. This will improve life for patients after surgery.
Future Directions in Prostate Cancer Treatment
The future of treating prostate cancer looks bright. New trends and tech are coming. Genomic medicine and immunotherapy will likely change how we treat prostate cancer. As research keeps moving forward, we’ll see more tailored and effective treatments for patients.
Conclusion
Men can live well after prostate removal with the right care and support. It’s key to understand how it affects urinary and sexual function. This helps manage expectations and improve life quality. Following a detailed recovery plan helps men avoid complications and adjust to body changes. Regular check-ups are vital. They help catch cancer signs early and solve problems quickly. Thanks to new prostate removal methods and ongoing support, men can face challenges head-on. They can keep a high quality of life. We stress the need for a strong support system for men to recover and thrive post-surgery.
FAQ
What is the primary function of the prostate gland?
The prostate gland is key to male reproductive health. It makes seminal fluid. This fluid nourishes and protects sperm during ejaculation.
Why is prostate removal surgery performed?
Surgery to remove the prostate is often for cancer. It’s called radical prostatectomy. For BPH, a simple prostatectomy is used to ease symptoms.
What are the potential side effects of prostate removal surgery?
Side effects can include trouble controlling urine, erectile issues, and changes in ejaculation and orgasm. But, how bad these are and for how long varies.
How long does it take to recover from prostate removal surgery?
Recovery time after prostate surgery varies. Most men can get back to normal in weeks to months. But, it can take up to a year or more to fully recover.
What are the alternatives to complete prostate removal?
Options besides removing the prostate include focal therapy and active surveillance. These might be good for early cancer or BPH.
How does prostate removal affect life expectancy?
Life expectancy after prostate removal depends on cancer stage, health, and other conditions. Thanks to better treatments, survival rates have improved a lot.
What follow-up care is required after radical prostatectomy?
After radical prostatectomy, regular check-ups and PSA tests are crucial. Also, watching for cancer signs is important.
Can erectile dysfunction after prostate removal be treated?
Yes, erectile dysfunction can be treated. Options include medications, lifestyle changes, and other interventions to help regain sexual function.
How can men cope with the psychological impact of prostate removal?
Men can deal with the emotional impact by seeking mental health support. They should also use coping strategies and talk openly with healthcare providers and loved ones.
What are the latest advances in prostate removal techniques?
New techniques include robotic-assisted surgery and focal therapy. These aim to lessen side effects and improve results.
What is the role of rehabilitation in recovering urinary function after prostatectomy?
Rehabilitation, like pelvic floor exercises, is key for urinary recovery after prostatectomy. It helps men regain control and manage incontinence.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/38233329/





