Learning about T lymphocytes is key for better immune care. At Liv Hospital, we focus on patient needs and follow global health standards. This ensures top-notch care for everyone.
T lymphocytes, or T cells, are vital for our immune system. They start from hematopoietic stem cells in the bone marrow and grow in the thymus. This growth is vital for fighting off infections and diseases.
We know how important T lymphocytes are for our immune system. We’re dedicated to giving top healthcare to all patients, including those from abroad.
Key Takeaways
- T lymphocytes are formed from hematopoietic stem cells in the bone marrow.
- Maturation of T lymphocytes occurs in the thymus.
- Understanding T lymphocyte development is key for immune care.
- Liv Hospital offers patient-focused care and follows global health standards.
- Advanced immune care relies on knowing how immune cells develop.
The Essential Role of T Lymphocytes in Immune Function
T lymphocytes are key players in our immune system. They help us fight off many diseases. These cells make sure our immune response is strong but controlled.
Definition and Types of T Lymphocytes
T lymphocytes, or T cells, are vital for cell-mediated immunity. There are different types of T cells, each with its own job. Cytotoxic T cells can kill infected cells or start the immune response. Helper T cells help activate other immune cells. Regulatory T cells keep the immune response in check, preventing harm to our own tissues.
“The diversity of T cell functions allows for a nuanced and effective immune response,” as noted by immunologists. This variety is key to fighting off many pathogens.
Overview of T Cell Functions in Immunity
T cells work together for our immune protection. Cytotoxic T cells kill infected cells or send signals. Helper T cells help B cells make antibodies to fight pathogens. Regulatory T cells balance the immune response, preventing autoimmunity.
- Cytotoxic T cells kill infected cells or produce chemical signals.
- Helper T cells assist in activating other immune cells.
- Regulatory T cells control the immune response.
Understanding T lymphocytes and their roles shows how complex and effective our immune system is. Ongoing research helps us find new ways to boost our immune function and treat diseases.
Understanding the Immune System’s Cellular Components

To fully grasp the immune response, it’s key to know the various cells involved. The immune system is a complex network of cells, tissues, and organs. They work together to protect the body from harmful pathogens.
The Lymphoid System Architecture
The lymphoid system is a critical part of the immune system. It includes primary and secondary lymphoid organs. Primary lymphoid organs, like the bone marrow and thymus, are where lymphocytes grow and mature.
Secondary lymphoid organs, like lymph nodes, spleen, and mucosa-associated lymphoid tissues (MALT), are where immune responses start. These organs help lymphocytes meet and fight antigens.
- Lymph nodes filter lymph fluid, trapping pathogens and activating immune cells.
- The spleen filters blood, removing old red blood cells and activating immune responses.
- MALT protects mucosal surfaces, such as those in the respiratory, gastrointestinal, and genitourinary tracts.
Differentiation Between Innate and Adaptive Immunity
The immune system is divided into innate immunity and adaptive immunity. Innate immunity offers quick defense against infection. It uses physical barriers, cells, and proteins to fight off pathogens.
Adaptive immunity, in contrast, provides long-lasting protection. It involves lymphocytes (T cells and B cells) that recognize and remember specific pathogens. This leads to a stronger response when the body faces the same pathogen again.
| Characteristics | Innate Immunity | Adaptive Immunity |
|---|---|---|
| Response Time | Immediate | Delayed, but more effective upon subsequent infections |
| Specificity | Non-specific | Specific to individual pathogens |
| Memory | No memory | Immunological memory |
It’s important to understand the difference between innate and adaptive immunity. T lymphocytes play a key role in adaptive immunity. They are vital for fighting infections and keeping an eye out for tumors.
Where Are T Lymphocytes Formed: The Bone Marrow Origin
In the bone marrow, hematopoietic stem cells turn into T lymphocyte precursors. This is key for the immune system’s growth. The bone marrow is where all blood cells, including T cell precursors, are made.
Hematopoietic Stem Cells as Precursors
Hematopoietic stem cells are vital for making all blood cells, including immune cells. They can grow and change into different cell types. Hematopoietic stem cells are the foundation of the immune system, leading to myeloid and lymphoid lineages. The lymphoid lineage includes T cells, B cells, and natural killer cells, all important for immunity.
Scientists are working on making T cells in the lab, which could change immune therapy as reported in this article. This shows how important T cell development is.
Early Development of Lymphoid Progenitors
The early stages of lymphoid progenitors are complex. Hematopoietic stem cells turn into multipotent progenitors. These then become lymphoid-primed multipotent progenitors, and then common lymphoid progenitors. These are the precursors to T cells, B cells, and other lymphoid cells.
“The development of lymphoid progenitors is a critical step in the formation of T lymphocytes, setting the stage for their maturation in the thymus.” –
The development of lymphoid progenitors is controlled by many factors, like transcription factors and cytokines. Knowing these controls helps us understand the immune system better.
| Cell Type | Description | Role in Immunity |
|---|---|---|
| Hematopoietic Stem Cells | Self-renewing cells that give rise to all blood cells | Foundation of the immune system |
| Lymphoid Progenitors | Cells that differentiate into T cells, B cells, and NK cells | Precursor to immune cells |
| T Lymphocytes | Mature cells that play a central role in cell-mediated immunity | Key players in adaptive immunity |
The creation of T lymphocytes from hematopoietic stem cells in the bone marrow is key. It sets the stage for a working immune system. Learning about this process helps us understand how the immune system works and when it doesn’t.
The Journey from Bone Marrow to Thymus
T cell precursors start their journey from the bone marrow to the thymus. They are guided by complex molecular signals. This journey is key for the development of T lymphocytes, which are vital for our immune response.
Mechanisms of T Cell Precursor Migration
The journey of T cell precursors from the bone marrow to the thymus is complex. Chemokines are key, providing signals for the cells to reach the thymus. These chemokines are essential for guiding the cells to their destination.
Research shows that specific chemokine receptors on T cell precursors interact with their ligands in the thymus. For example, CCR9 and CCL25 are important in this process. This interaction is vital for T cell development.
Factors Influencing Thymic Homing
Several factors affect T cell precursors’ homing to the thymus. Adhesion molecules and their ligands help in the initial steps of migration. These interactions are critical for the cells to enter the thymus.
The thymus’s microenvironment also supports the migration and development of T cell precursors. The thymic stroma provides growth factors and signals for T cell maturation. Understanding these factors is key to grasping T cell development.
In conclusion, the journey of T cell precursors from the bone marrow to the thymus is complex. It involves multiple molecular signals and cellular interactions. We’ve highlighted the key mechanisms and factors, showing their importance in developing a functional immune system.
The Thymus: Primary Site of T Lymphocyte Maturation
The thymus is key to our immune system. It’s where T lymphocytes mature. This is vital for a strong immune system. We’ll look at the thymus’s structure and its role in T cell maturation.
Thymic Architecture and Microenvironments
The thymus has different areas, like the cortex and medulla. These areas have unique environments for T cell development. The cortex is where T cells start to grow and get selected. The medulla is where they finish maturing and getting selected.
The thymus’s design helps T cells mature. The cortex is full of young T cells. The medulla has more mature T cells and other important cells. These cells help T cells get ready to fight off infections.
Cellular Interactions in the Thymus
In the thymus, cells work together to help T cells mature. They make sure T cells can fight off infections without attacking the body. This is called positive selection. They also remove T cells that might attack the body, which is called negative selection.
The thymus’s environment is key to these interactions. T cells and other cells, like thymic epithelial cells and dendritic cells, work together. This teamwork is essential for T cells to be ready to fight off infections without attacking the body.
The Complex Process of T Cell Maturation
T cell development in the thymus is a complex process. It involves several stages that lead to mature T cells. This journey includes many cellular interactions and selection processes. These ensure the production of functional and self-tolerant T cells.
Stages of T Cell Development in the Thymus
The development of T cells in the thymus has three main stages: double-negative, double-positive, and single-positive.
- Double-Negative Stage: At this initial stage, T cell precursors lack both CD4 and CD8 markers. During this phase, the cells undergo rearrangement of the T cell receptor (TCR) genes.
- Double-Positive Stage: Cells that successfully rearrange their TCR genes progress to the double-positive stage, where they express both CD4 and CD8 markers. This stage is critical for the selection processes that follow.
- Single-Positive Stage: After undergoing positive and negative selection, T cells mature into either CD4+ or CD8+ single-positive cells, which are then released into the periphery.
CD4 and CD8 Lineage Commitment
The commitment to either the CD4 or CD8 lineage is a key part of T cell development. This process is tightly regulated and involves complex signaling pathways.
CD4 lineage commitment is linked to helper T cells, which are vital for coordinating immune responses. On the other hand, CD8 lineage commitment leads to cytotoxic T cells. These cells are key in eliminating infected cells or tumor cells.
“The precise regulation of CD4 and CD8 lineage commitment is critical for the proper functioning of the immune system.”
Many factors influence lineage commitment, including the strength of TCR signaling and specific transcription factors. Understanding these processes is key to grasping the complexity of T cell development.
Selection Processes in T Cell Development
T cell development is shaped by two key processes: positive selection and negative selection. These processes are vital for T cells to fight off infections without attacking the body’s own cells.
Positive Selection: Ensuring MHC Restriction
Positive selection picks T cells that can recognize self-MHC molecules. This is important because it lets T cells work well with antigen-presenting cells. T cells that can’t recognize self-MHC molecules die off.
MHC restriction is a result of positive selection. It means T cells can only see antigens presented by self-MHC molecules. This helps T cells fight off invaders while ignoring the body’s own cells.
Negative Selection: Eliminating Self-Reactive T Cells
Negative selection gets rid of T cells that react to self-antigens. This happens mainly in the thymus, where T cells meet self-antigens. T cells that react too strongly to these antigens die, preventing them from causing harm.
Negative selection is very important. It keeps the immune system from attacking itself by making sure T cells don’t react to the body’s own tissues.
| Selection Process | Function | Outcome |
|---|---|---|
| Positive Selection | Ensures T cells can recognize self-MHC molecules | MHC restriction; survival of potentially useful T cells |
| Negative Selection | Eliminates T cells reactive against self-antigens | Prevention of autoimmunity; immune tolerance |
In summary, the selection processes in T cell development are key for a healthy immune system. Positive and negative selection work together to make sure T cells can fight off infections without harming the body.
Comparing T and B Lymphocyte Development
T and B lymphocytes start from hematopoietic stem cells in the bone marrow. But, their growth paths are quite different. T cells grow up in the thymus, while B cells finish their growth in the bone marrow. This shows just one of the many ways they are unique.
B Cell Maturation in the Bone Marrow
B cell growth in the bone marrow goes through many stages. From the pro-B cell to the mature B cell, they make unique antibodies. The bone marrow’s environment is key for their growth.
“The bone marrow is a supportive place for B cell growth,” say immunology experts. It has many cell types and growth factors helping them mature.”
Key Differences in Developmental Pathways
T and B lymphocytes have different growth paths. T cells grow in the thymus, where they learn to recognize self-MHC molecules. This helps them avoid attacking the body’s own cells. B cells, on the other hand, grow in the bone marrow. They also learn to avoid attacking the body, but in a different way.
- T cells undergo thymic selection, which includes both positive and negative selection.
- B cells undergo selection in the bone marrow, with a focus on eliminating self-reactive B cells.
- The thymus and bone marrow provide unique microenvironments that support the maturation of T and B cells, respectively.
Knowing these differences helps us understand T and B cells’ roles in fighting off infections. By looking at how they grow, we learn more about how our immune system works and how it can go wrong.
Age-Related Changes in T Lymphocyte Production
Aging affects how our immune system works, including T lymphocytes. These cells are key to fighting off infections and diseases. As we get older, our immune system changes, making it less effective.
The thymus, where T lymphocytes mature, shrinks with age. This starts early and gets worse with time. It means fewer new T cells are made.
Thymic Involution and Its Impact
The thymus gland gets smaller after puberty. This makes it harder for it to produce mature T lymphocytes. The decline in thymic function means fewer naive T cells, which are important for fighting new infections.
Research shows thymic involution is more than just shrinking. It’s a complex process that changes the thymus’s environment.
“The thymus is a barometer of immunological health, and its involution has significant implications for immune function in aging individuals.”
| Age Group | Thymic Function | T Cell Production |
|---|---|---|
| Young Adults | High | High |
| Middle-Aged | Moderate | Moderate |
| Elderly | Low | Low |
Consequences for Immune Function in Aging
Thymic involution affects T lymphocyte production, leading to weaker immune function in older adults. This results in a less diverse T cell repertoire, making it harder to fight off infections and respond to vaccines.
Also, fewer naive T cells mean the immune system can’t handle new pathogens well. This shows why understanding these changes is key to improving immune function in older adults.
In summary, thymic involution greatly impacts immune function in older people. Knowing this helps us find ways to boost immune health in seniors.
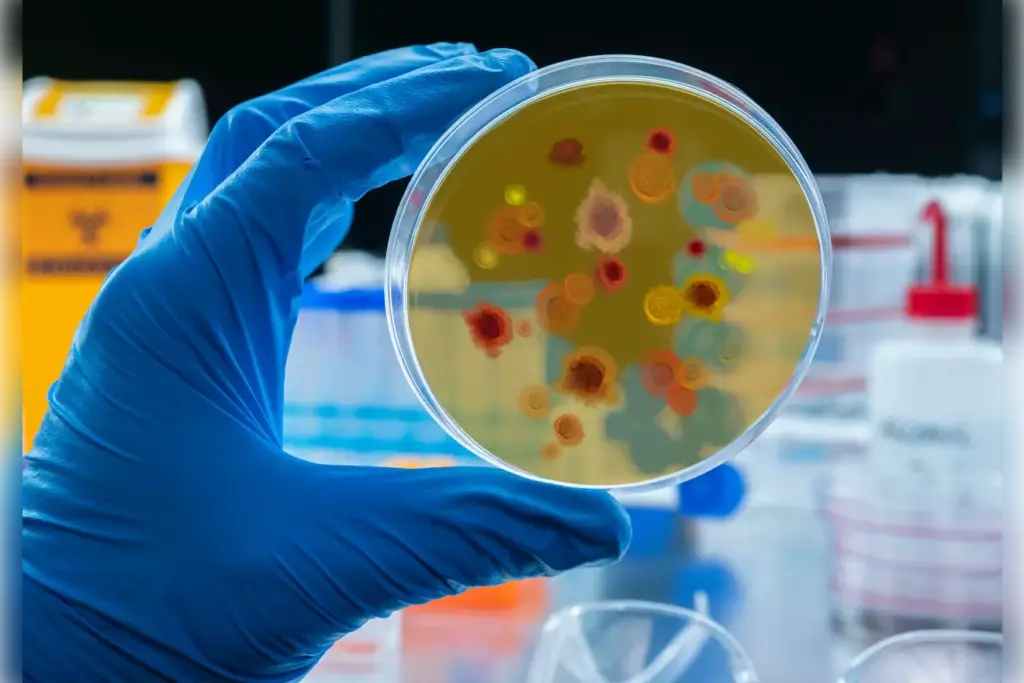
Clinical Implications of T Cell Development
Understanding T cell development is key to grasping immunodeficiencies and finding treatments. T cells are vital to our immune system. Problems in their development can cause many health issues.
Immunodeficiencies Related to T Cell Formation
Defects in T cell development can lead to different kinds of immunodeficiencies. These can be mild or severe. They often come from genetic mutations that affect T cell growth or signaling.
Severe Combined Immunodeficiency (SCID) is a serious condition where people lack T cells. This makes them very prone to infections. DiGeorge Syndrome is another example, showing how important T cell development is for our immune system.
Therapeutic Approaches Targeting T Cell Development
New treatments are being developed thanks to our growing knowledge of T cell development. Gene therapy is one, aiming to fix genetic problems in SCID and other conditions. It’s a big step towards treating these diseases.
Immunomodulatory therapies are also being explored. They try to improve T cell function in autoimmune diseases or boost T cell responses in cancer treatment. These therapies show promise in treating various immune disorders by targeting T cell development.
As we learn more about T cell development, we’ll see more treatments for immunodeficiencies and T cell-related conditions. This is an exciting area of research.
Conclusion
We’ve looked into how T lymphocytes form and mature, showing their key role in our immune system. T lymphocytes are vital for our body’s defense, starting their journey in the bone marrow and finishing in the thymus.
Knowing how T lymphocytes develop helps us understand how our immune system works. The factors that affect their growth and function are key to a strong immune response against diseases.
Understanding T lymphocytes helps us tackle immune-related diseases better. As we learn more about the immune system, we can create better treatments. This will help keep our immune system strong and our health good.
Where are T lymphocytes formed?
T lymphocytes start in the bone marrow. They come from hematopoietic stem cells.
Where do T lymphocytes mature?
They mature in the thymus. Here, they go through many stages and selection processes.
What is the role of the thymus in T lymphocyte development?
The thymus is key for T lymphocyte maturation. It provides a special environment for T cell development and selection.
What are the different types of T lymphocytes?
There are several types of T lymphocytes. These include cytotoxic T cells, helper T cells, and regulatory T cells. Each type has its own role in the immune response.
How do T lymphocytes develop from hematopoietic stem cells?
T lymphocytes start from hematopoietic stem cells in the bone marrow. They then move to the thymus for maturation and selection.
What is the significance of positive and negative selection in T cell development?
Positive selection helps T cells interact with self-MHC molecules. Negative selection removes self-reactive T cells. This ensures T cells are functional and tolerant.
How does T lymphocyte development differ from B lymphocyte development?
T and B lymphocytes both start from hematopoietic stem cells in the bone marrow. But, they mature in different places (thymus for T cells and bone marrow for B cells). Their development processes are also different.
What is thymic involution, and how does it impact immune function?
Thymic involution is the thymus shrinking with age. This leads to fewer new T cells, affecting immune function in older adults.
What are the clinical implications of defects in T cell development?
Defects in T cell development can cause immunodeficiencies. Understanding T cell biology is key for treating these conditions.
Where do T cells migrate to for maturation?
T cells go to the thymus for maturation. There, they go through developmental stages and selection processes.
What is the site of T lymphocyte maturation?
The thymus is where T lymphocytes mature. Here, they undergo positive and negative selection to become functional and self-tolerant.
References
- LibreTexts. Maturation of T Cells. In Adaptive Immunity. Available from: https://med.libretexts.org/Bookshelves/Anatomy_and_Physiology/Anatomy_and_Physiology_(Boundless)/20:_Immune_System/20.3:_Adaptive_Immunity/20.3C:_Maturation_of_T_Cells
- British Society for Immunology / Immunology.org. T-cell development / the thymus. Available from: https://www.immunology.org/public-information/bitesized-immunology/immune-development/t-cell-development-thymus
- Starr TK, Jameson SC, Hogquist KA. Positive and negative selection of T cells. Nature Reviews Immunology. 2003;3(4):269-278. Available from: https://www.nature.com/articles/nri913
- Osmosis. T-cell development [Video]. Available from: https://www.osmosis.org/video/T-cell_development
- Singer A, Adoro S, Park JH. Lineage fate and intense debate: myths, models and mechanisms of CD4- versus CD8-lineage choice. PMC. 2010;1:75. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC2958614/