Patients might worry about how their bladder function will change after a robotic hysterectomy. Changes in bladder function can really affect a person’s life during recovery time.
It’s important for patients to know about the possible hysterectomy side effects on the bladder. This helps them understand what to expect and make better choices about their care.
Key Takeaways
- Robotic hysterectomy is a minimally invasive surgery that can affect bladder function.
- Changes in bladder function can impact a patient’s quality of life.
- Understanding possible side effects is key for managing expectations.
- Recovery time can vary based on individual factors.
- Patients should talk to their healthcare provider about their concerns.
Understanding Hysterectomy: Types and Approaches

A hysterectomy is when the uterus is surgically removed. It’s done for many reasons, like uterine cancer, fibroids, and severe bleeding. The surgery can vary in how much is removed and the method used.
What is a Hysterectomy?
A hysterectomy is a surgery to remove the uterus. Sometimes, other parts of the reproductive system are also removed. This is done for conditions like uterine cancer, endometriosis, and fibroids.
Doctors usually suggest a hysterectomy after trying other treatments. It’s a big surgery that affects a woman’s reproductive and overall health.
Different Types of Hysterectomies
There are several types of hysterectomies:
- Partial (or Subtotal) Hysterectomy: Removes the uterus but keeps the cervix.
- Total Hysterectomy: Removes both the uterus and the cervix.
- Radical Hysterectomy: Removes the uterus, cervix, part of the vagina, and sometimes lymph nodes. It’s for cancer cases.
Each type is chosen based on the patient’s condition, age, and health status.
Traditional vs. Minimally Invasive Approaches
Hysterectomies can be done in different ways. Traditional open hysterectomy uses a big incision. Minimally invasive approaches, like laparoscopic or robotic, use smaller cuts. These can lead to quicker recovery and less pain.
Robotic hysterectomy is a minimally invasive method. It uses a robotic system for better precision and flexibility. It has benefits like less blood loss, shorter hospital stays, and fewer complications.
Robotic Hysterectomy: A Modern Surgical Technique

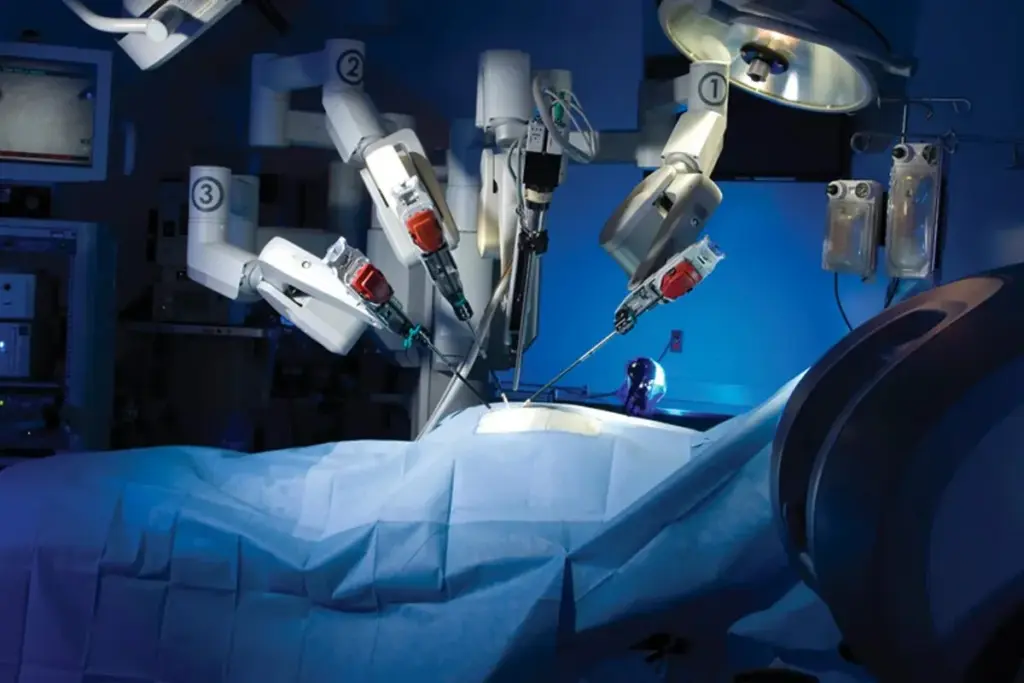
Robotic-assisted hysterectomy is a new way to do surgery. It lets surgeons work with more precision and flexibility. This method has changed gynecological surgery, giving patients a less invasive option for hysterectomies.
How Robotic Surgery Works
Robotic hysterectomy uses a special robotic system. This system lets surgeons do complex surgeries through small cuts. It has a console for the surgeon, robotic arms, and a 3D vision system.
Key Components of Robotic Surgery:
- High-definition 3D visualization
- Robotic arms with precise instrumentation
- Enhanced ergonomics for the surgeon
The surgeon controls the robotic arms from a console. This setup gives them more precision and control than traditional surgery.
Benefits of Robotic-Assisted Hysterectomy
Robotic-assisted hysterectomy has many benefits. Some of the main advantages are:
|
Benefit |
Description |
|---|---|
|
Less Pain |
Smaller cuts mean less damage and pain after surgery. |
|
Quicker Recovery |
Patients usually heal faster and can get back to normal sooner. |
|
Reduced Risk of Complications |
The precision of robotic surgery lowers the risk of problems during and after surgery. |
Potential Drawbacks and Considerations
While robotic hysterectomy has many benefits, there are also some downsides. These include:
- Higher costs associated with robotic surgery
- Limited availability of robotic systems in all medical facilities
- The need for specialized training for surgeons
Patients should talk to their healthcare provider about these points. This helps decide if robotic hysterectomy is right for them.
The Relationship Between the Uterus and Bladder
It’s important to know how the uterus and bladder work together. This is key to understanding how a hysterectomy might affect the bladder. They are connected through their anatomy, support structures, and nerve pathways.
Anatomical Proximity
The uterus and bladder are very close in the pelvic cavity. This closeness means surgery in this area can affect both organs. The bladder is right in front of the uterus, held in place by support structures.
Shared Support Structures
The uterus and bladder have a shared system of support. This includes ligaments and muscles of the pelvic floor. These structures are vital for both organs to function properly. The pelvic floor muscles, in particular, support both organs and are essential for their normal function.
Nerve Pathways Affecting Both Organs
The nerves for the uterus and bladder come from the same pelvic plexus. This means they share a nerve pathway. Damage to these nerves during a hysterectomy can affect the bladder. It’s important for surgeons to understand these pathways to avoid damage during robotic hysterectomy.
|
Aspect |
Description |
Impact on Bladder Function |
|---|---|---|
|
Anatomical Proximity |
Close location of uterus and bladder |
Potential for surgical impact on bladder |
|
Shared Support Structures |
Common ligaments and pelvic floor muscles |
Influence on bladder position and function |
|
Nerve Pathways |
Shared nerve supply from pelvic plexus |
Possible nerve damage during hysterectomy |
The connection between the uterus and bladder is complex. It involves anatomy, structure, and nerves. Knowing this relationship helps predict and manage how a hysterectomy might affect the bladder.
Immediate Effects on the Bladder During Surgery
During a robotic hysterectomy, the bladder faces several immediate effects. Its close location to the uterus means surgery in this area can affect bladder function and position.
Surgical Manipulation and Temporary Displacement
The robotic hysterectomy procedure involves surgical manipulation that may cause temporary displacement of the bladder. This is needed to ensure a clear surgical site for the surgeon to safely perform the hysterectomy.
The bladder is carefully moved aside to access the uterus. This can sometimes lead to temporary changes in its position or function.
Catheterization During the Procedure
Catheterization is a common practice during robotic hysterectomy. It ensures the bladder is empty and doesn’t block the surgical area. This reduces the risk of bladder injury during the procedure.
The catheter is usually removed shortly after surgery. This is when the patient can urinate on their own.
Potential for Intraoperative Complications
While rare, intraoperative complications like bladder injury can happen during robotic hysterectomy. The risk is lowered by the surgeon’s skill and the precision of robotic-assisted surgery.
It’s important to watch for any signs of complications during surgery. This ensures any issues are quickly dealt with.
Common Bladder Issues in the First Week After Surgery
Knowing about bladder problems after a robotic hysterectomy helps patients get ready for recovery. In the first week, women might face several bladder issues. These problems come from the surgery and how the body reacts to it.
Urinary Retention
Urinary retention is a common problem in the first week after surgery. It happens when you can’t fully empty your bladder. Swelling, pain, or nerve damage from surgery can cause it. It’s important to watch your urine output and tell your healthcare providers if you have trouble.
Difficulty Emptying the Bladder Completely
Some patients struggle to empty their bladder fully. This might be because of the catheter used during surgery or swelling after it. Proper catheter care and following your healthcare team’s advice can help.
Catheter Management and Removal
Managing your catheter is key after surgery. The catheter usually comes out a few days after, but it depends on your recovery. Pay attention to signs of urinary tract infections and follow your healthcare team’s instructions for catheter care and removal.
Here are some tips for dealing with bladder issues:
- Drink enough fluids to keep your urinary system clean
- Use a timed voiding schedule to train your bladder
- Do pelvic floor exercises as your healthcare provider suggests
- Watch for signs of infection, like burning while urinating or fever
Understanding these bladder issues and how to handle them can make your recovery smoother after a robotic hysterectomy.
Hysterectomy Recovery: Bladder Function Weeks 1-4
After a robotic hysterectomy, the bladder goes through changes. It’s important to understand these changes and how to manage them for a smooth recovery.
Gradual Return to Normal Urination
Patients usually start to urinate normally again in the first few weeks. At first, they might need a catheter to help empty their bladder. As they heal, the catheter is removed, and they regain bladder control.
Key milestones in the return to normal urination include:
- Reduced reliance on catheterization
- Increased bladder capacity
- Improved ability to empty the bladder completely
Managing Urgency and Frequency
Women may feel the need to urinate often and urgently after surgery. These symptoms can be managed with lifestyle changes and exercises.
Strategies for managing urgency and frequency include:
- Fluid management: Monitoring and adjusting fluid intake to reduce frequency
- Timed voiding: Scheduling regular bathroom visits to maintain bladder control
- Pelvic floor exercises: Strengthening the muscles that support bladder function
Exercises to Improve Bladder Control
Pelvic floor exercises, or Kegel exercises, are great for bladder control. They strengthen the muscles around the bladder, helping to prevent incontinence and improve bladder function.
To perform Kegel exercises:
- Identify the pelvic floor muscles by stopping the flow of urine mid-stream
- Contract these muscles for 5-10 seconds, then release for the same duration
- Repeat this cycle 10-15 times, three times a day
By doing these exercises daily, women can improve their bladder control. This can help prevent long-term bladder problems after a robotic hysterectomy.
Long-Term Changes to Bladder Position and Support
After a robotic hysterectomy, the body’s anatomy changes. This can affect the bladder’s health. The uterus’s removal can shift the pelvic anatomy, impacting the bladder’s support.
Anatomical Shifts After Uterus Removal
The uterus is key to the pelvic anatomy. Its removal can cause the bladder to shift. These anatomical shifts can change how the bladder is supported and functions.
Research shows that uterus removal can change the bladder’s position. This can lead to urinary incontinence or trouble fully emptying the bladder.
Impact on Pelvic Floor Support
The pelvic floor supports the bladder and other organs. After a hysterectomy, this support can weaken. This can cause long-term bladder control and support issues.
Weakened pelvic floor muscles can lead to less bladder support. This can cause stress urinary incontinence. It’s important for patients to know about these changes to manage their bladder health.
Preventive Measures for Optimal Healing
To lessen the long-term effects on bladder support, several preventive measures can help. Pelvic floor exercises, like Kegel exercises, can strengthen the bladder’s support muscles.
- Do regular pelvic floor physical therapy to improve muscle strength and coordination.
- Keep a healthy weight to reduce pressure on the pelvic floor.
- Avoid heavy lifting and bending to minimize strain on the pelvic anatomy.
By taking these steps, patients can help their bodies heal better. This can reduce the risk of long-term bladder support and function problems.
Potential Complications: Urinary Tract Infections
Hysterectomy patients should know about the risk of urinary tract infections during recovery. UTIs can happen after a hysterectomy. Knowing the risks and taking steps to prevent them can help.
Increased Risk Factors Post-Surgery
Several factors raise the risk of UTIs after a hysterectomy. Catheter use during and after surgery is a big risk, as it can bring bacteria into the urinary tract. Also, temporary changes in urinary tract function and nerve damage during surgery can increase the risk.
The use of a catheter is necessary but can let bacteria into the urinary system. Healthcare providers must use strict sterile techniques when inserting and maintaining catheters to lower this risk.
Symptoms to Watch For
It’s important to know the symptoms of UTIs to get treatment early. Common signs include dysuria (painful urination), frequent urination, and urine that is cloudy or has a strong odor. Some people may also feel pelvic pain or discomfort.
If you notice these symptoms, contact a healthcare provider right away. Early treatment can stop the infection from spreading to the kidneys, which can cause more serious problems.
Prevention Strategies
There are ways to prevent UTIs after a hysterectomy. Proper catheter care and removing the catheter as soon as it’s no longer needed are key. Drinking plenty of water helps flush out bacteria from the urinary tract.
Good hygiene, like wiping from front to back, can also prevent bacteria spread. Some doctors might suggest cranberry products or probiotics to prevent UTIs. But, the evidence for these is not clear-cut.
Managing Incontinence After Hysterectomy
Managing incontinence after a hysterectomy means knowing its types and causes. It also involves finding effective ways to manage it. The surgery can affect the pelvic floor and nearby structures, leading to incontinence.
Types of Incontinence That May Occur
Women may face different types of incontinence after a hysterectomy. These include:
- Stress Incontinence: This is when urine leaks when you cough, sneeze, or move a lot.
- Urge Incontinence: It’s when you suddenly feel the need to urinate and can’t hold it.
- Overflow Incontinence: This is when urine leaks constantly because you can’t empty your bladder fully.
- Mixed Incontinence: It’s a mix of stress and urge incontinence.
Understanding these types of incontinence is crucial for developing an effective management plan.
Conservative Management Approaches
There are many ways to manage incontinence without surgery. These include:
- Pelvic Floor Exercises: Kegel exercises can strengthen the muscles that control your bladder.
- Behavioral Therapies: Bladder training and timed voiding can help manage incontinence.
- Lifestyle Modifications: Drinking the right amount of water, avoiding caffeine and alcohol, and keeping a healthy weight can also help.
These methods can be adjusted to fit your specific needs and type of incontinence.
When to Consider Additional Interventions
If these methods don’t work, you might need more help. This could include:
- Medications: To help with urge incontinence or improve bladder control.
- Minimally Invasive Procedures: Like bulking agents or sling procedures to support the urethra.
- Surgical Options: Surgery might be needed to fix underlying issues causing incontinence.
Talking to a healthcare provider is key to finding the right solution for you.
Understanding incontinence and trying different management strategies can help women after a hysterectomy. It can greatly improve their quality of life.
Pelvic Floor Physical Therapy for Bladder Recovery
After a hysterectomy, pelvic floor physical therapy can greatly help with bladder recovery. This therapy is made for those facing challenges with bladder function and pelvic health after surgery.
Benefits of Specialized Physical Therapy
Pelvic floor physical therapy brings many benefits to those recovering from a hysterectomy. Improved bladder control is a key advantage. It strengthens the muscles that help the bladder work better. It also lowers the chance of problems like urinary incontinence and pelvic organ prolapse.
Medical News Today says this therapy boosts muscle strength and improves pelvic floor function. This helps a lot with bladder recovery.
Common Therapeutic Techniques
Therapists use different methods to help patients after a hysterectomy. These include:
- Pelvic floor exercises, like Kegel exercises, to make bladder muscles stronger.
- Manual therapy to loosen tension in the pelvic floor muscles.
- Biofeedback to help patients control their pelvic floor muscles.
- Electrical stimulation to build muscle strength and better bladder control.
Finding a Qualified Pelvic Floor Therapist
To find a good pelvic floor therapist, look for someone with the right training. Make sure they have certifications and experience with post-hysterectomy patients. Getting recommendations from doctors or support groups can also help a lot.
Adding pelvic floor physical therapy to your recovery plan can greatly improve bladder function. It can also make your life better after a hysterectomy.
Lifestyle Modifications to Support Bladder Health
To keep your bladder healthy after a robotic hysterectomy, making some changes is key. You’ll want to eat right, manage your fluids, and adjust your activities. These steps can really help your recovery and bladder function.
Dietary Considerations
Eating well is important for bladder health. Some foods can bother your bladder, while others help. More fiber can stop constipation, which is good because straining can hurt your bladder.
Here are some diet tips:
- Eat foods high in fiber like fruits, veggies, and whole grains
- Try to avoid or cut down on foods that irritate your bladder, like caffeine, alcohol, and spicy foods
- Add foods rich in omega-3 fatty acids to fight inflammation
Fluid Management Strategies
It’s important to manage your fluids well for bladder health. You want to stay hydrated but not overdo it. Drinking water is good, but how much and when depends on you.
Here are some tips for managing fluids:
- Drink most of your fluids during the day and less at night to avoid midnight bathroom trips
- Stay away from fluids that can irritate your bladder, like those with caffeine or alcohol
- Check your urine color to make sure it’s pale yellow, which means you’re drinking enough
Activity Modifications During Recovery
Changing how you move during recovery can help your bladder. Avoid heavy lifting and bending to ease pressure on your pelvic floor.
Here are some activity changes to consider:
|
Activity |
Recommended Modification |
Benefits |
|---|---|---|
|
Heavy Lifting |
Avoid lifting objects over 10 pounds |
Reduces strain on the pelvic floor |
|
Bending and Straining |
Minimize bending and straining activities |
Decreases pressure on the bladder |
|
Exercise |
Engage in gentle exercises like pelvic tilts and Kegel exercises |
Strengthens pelvic floor muscles |
When to Seek Medical Attention for Bladder Issues
Knowing when to get medical help after a hysterectomy is key. Some bladder problems are normal, but others might mean you need to see a doctor right away.
Red Flag Symptoms
Some symptoms mean you should get help fast. These include:
- Severe pain or discomfort in the pelvic area
- Difficulty starting or stopping urine flow
- Persistent or severe urinary incontinence
- Blood in the urine or abnormal discharge
- Fever or chills, which could indicate infection
Medical News Today says it’s important to know these signs. This way, you can get help quickly and avoid bigger problems.
Differentiating Normal Recovery from Complications
It’s important to tell normal recovery symptoms from signs of trouble. Normal symptoms might be a little discomfort or needing to pee more often. But if these get worse or you notice other bad signs, you should see a doctor.
Watching how your body reacts to surgery and knowing what’s normal can help spot problems early.
Emergency vs. Routine Follow-up Concerns
It’s important to know if your symptoms are an emergency or if you can wait for a check-up. Emergencies include a lot of pain, a lot of bleeding, or signs of infection. For less urgent issues, you should make an appointment with your doctor.
“If you’re experiencing symptoms that are concerning or worsening, it’s always better to err on the side of caution and seek medical advice.”
Being informed and proactive can help you recover faster. This way, you can deal with any bladder problems quickly.
Long-Term Bladder Function After Robotic Hysterectomy
It’s important for women to know how robotic hysterectomy affects bladder function long-term. This surgery is known for being less invasive and having quicker recovery times. But, its lasting effects on bladder function are a big worry for many.
What to Expect at 6 Months
Managing these symptoms can involve pelvic floor exercises, changing what you eat, and sometimes medicine. It’s key to keep up with your doctor to check on your progress and fix any issues.
One Year Post-Surgery and Beyond
By one year after surgery, most women fully recover bladder function. Research shows robotic hysterectomy has lower risks of bladder problems compared to older surgeries.
Things like your health, age, and any past health issues can change how fast and fully you recover. Staying healthy, eating right, and exercising can help keep your pelvic area in good shape.
Factors Affecting Long-Term Outcomes
Several things can impact how well your bladder works long-term after robotic hysterectomy. These include your age at surgery, any past pelvic floor problems, and the surgery method used.
- The surgeon’s skill and experience
- How well you follow post-op care
- Any issues that come up during or after surgery
Knowing these factors helps doctors give better care and advice. This can help women have better bladder function long-term after robotic hysterectomy.
Comparing Bladder Effects: Robotic vs. Traditional Hysterectomy
It’s important to know the differences between robotic and traditional hysterectomy for bladder health after surgery. Both methods have their own benefits and drawbacks, mainly for bladder recovery.
Recovery Trajectories
The recovery for bladder function is different between robotic and traditional hysterectomy. Robotic surgery is less invasive, leading to quicker recovery times. Studies show patients with robotic hysterectomy have less pain and shorter hospital stays. This means they can get back to normal bladder function faster.
On the other hand, traditional hysterectomy, with its larger incision, takes longer to recover. The bigger incision can cause more pain and longer use of catheters. This affects bladder recovery more.
Complication Rates and Severity
Robotic hysterectomy has lower complication rates, including bladder issues. Its precision reduces damage to tissues and nerves. This lowers the risk of long-term bladder problems.
Traditional hysterectomy, though effective, has a higher risk of complications like infections and adhesions. These can harm bladder health. The severity of these complications can be high and often need more medical help.
|
Surgical Method |
Complication Rate |
Severity of Complications |
|---|---|---|
|
Robotic Hysterectomy |
Lower |
Less Severe |
|
Traditional Hysterectomy |
Higher |
More Severe |
Patient-Reported Outcomes
Patient feedback shows robotic hysterectomy has better effects on bladder health. Studies show patients are happier and have fewer bladder problems after robotic surgery. This is because robotic surgery is more precise and less invasive.
Patients usually feel less pain and have fewer complications. This makes their recovery better.
In summary, robotic and traditional hysterectomy both have their uses in gynecological surgery. But, the choice affects bladder health and recovery. Knowing these differences helps patients and doctors make better decisions.
Conclusion: The Road to Complete Bladder Recovery
Understanding how robotic hysterectomy affects the bladder is key for a good recovery. This article has looked at how the uterus and bladder work together. It also covered the immediate and long-term effects of surgery and how to manage bladder health after.
For bladder recovery, a complete care plan is needed. This includes pelvic floor physical therapy, making lifestyle changes, and knowing about possible problems. By following recovery tips like eating right, managing fluids, and adjusting activities, patients can better their bladder health and overall well-being.
Future studies might aim to improve surgery techniques and post-op care to reduce bladder issues. As research grows, we’ll learn more about what affects bladder recovery. This will help doctors give better support to patients after robotic hysterectomy.
By summarizing important points and stressing the need for full care, patients and doctors can work together. This will help achieve the best results and improve bladder recovery after robotic hysterectomy. It will also make life better overall.
FAQ
What is a robotic hysterectomy?
A robotic hysterectomy is a surgery to remove the uterus. It uses a robotic system for better precision and flexibility.
How does a hysterectomy affect the bladder?
The uterus and bladder are close together. This can cause bladder issues like trouble urinating and incontinence.
What are the common bladder issues after a robotic hysterectomy?
Issues include trouble urinating and incontinence. These can be managed with exercises and lifestyle changes.
How long does it take to recover from a robotic hysterectomy?
Recovery time is about 4-6 weeks. Bladder function may take months to fully recover.
What are the benefits of pelvic floor physical therapy after a hysterectomy?
Physical therapy can improve bladder function and reduce incontinence. A therapist can create a personalized exercise plan.
How can I prevent urinary tract infections (UTIs) after a hysterectomy?
Stay hydrated and practice good hygiene to prevent UTIs. Watch for symptoms and seek medical help if needed.
What lifestyle modifications can support bladder health after a hysterectomy?
Making dietary changes and managing fluids can help. Pelvic floor exercises can also improve bladder control.
When should I seek medical attention for bladder issues after a hysterectomy?
Seek medical help for severe pain, trouble urinating, or signs of infection. It’s important to know when to seek help.
How does robotic hysterectomy compare to traditional hysterectomy in terms of bladder effects?
Robotic hysterectomy may have faster recovery and fewer complications. But, results can vary, so talk to your doctor.
What can I expect in terms of long-term bladder function after a robotic hysterectomy?
Most women see improvement in bladder function within 6-12 months. Health, pelvic floor strength, and lifestyle habits play a role.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC6497180/





