Last Updated on October 21, 2025 by mcelik
Myeloproliferative neoplasms (MPNs) are rare blood cancers that affect many people. They happen to about 0.5-3.2 per 100,000 people each year. Knowing how they are diagnosed is very important.
To find out if someone has myeloproliferative neoplasms, doctors use many steps. They look at the patient’s medical history and do a physical check-up. They also run lab tests and might do genetic tests.
The World Health Organization (WHO) has a guide for diagnosing MPNs. This guide helps doctors figure out if someone has polycythemia vera (PV), essential thrombocythemia (ET), or primary myelofibrosis (PMF).
Key Takeaways
- MPNs are rare hematological disorders.
- Diagnosis involves a combination of clinical findings and laboratory tests.
- The WHO classification is used to diagnose MPNs.
- Polycythemia vera, essential thrombocythemia, and primary myelofibrosis are the three classic MPNs.
- Genetic testing may be required for an accurate diagnosis.
What Are Myeloproliferative Disorders?

Myeloproliferative neoplasms (MPNs) are diseases where the bone marrow makes too many blood cells. This can cause health problems. The bone marrow makes too many red blood cells, white blood cells, or platelets.
Definition and Classification
MPNs are a kind of blood cancer that starts in the bone marrow. “Myeloproliferative” means the bone marrow makes too many blood cells. They are divided based on the type of blood cell made too much and genetic mutations.
The World Health Organization (WHO) has a system to classify MPNs. This system helps doctors diagnose and understand the different types of MPNs. It’s important to choose the right treatment.
Common Types of Myeloproliferative Neoplasms
There are three main types of MPNs: Polycythemia Vera (PV), Essential Thrombocythemia (ET), and Primary Myelofibrosis (PMF).
- Polycythemia Vera (PV): This is when there are too many red blood cells. It can make blood thick and increase the risk of blood clots.
- Essential Thrombocythemia (ET): This is when there are too many platelets. It can make bleeding or clotting more likely.
- Primary Myelofibrosis (PMF): This is when the bone marrow gets scarred. It can cause anemia, spleen enlargement, and other problems.
| Type of MPN | Primary Characteristic | Common Complications |
| Polycythemia Vera (PV) | Overproduction of red blood cells | Blood clots, thickened blood |
| Essential Thrombocythemia (ET) | Overproduction of platelets | Bleeding, clotting |
| Primary Myelofibrosis (PMF) | Scarring of the bone marrow | Anemia, spleen enlargement |
Prevalence and Risk Factors
MPNs are not very common, with about 1-3 cases per 100,000 people each year. The risk factors differ for each type of MPN.
Genetic mutations, like the JAK2 mutation, and exposure to toxins can increase the risk of MPNs. Knowing these risk factors helps in early detection and management.
Early Signs and Symptoms of Myeloproliferative Disorder
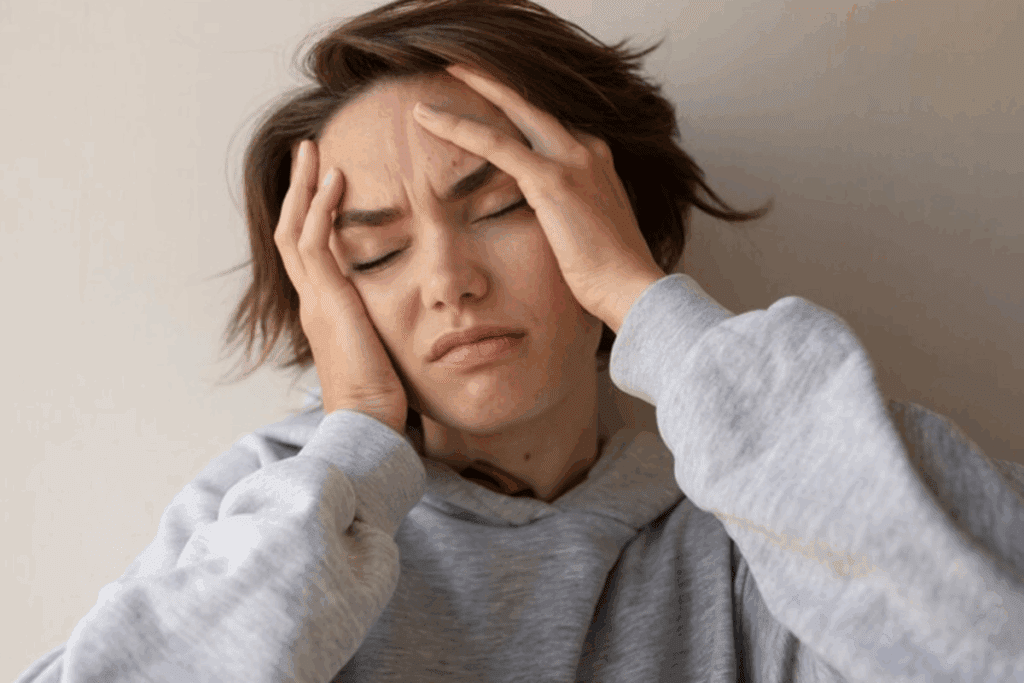
It’s important to spot the early signs of myeloproliferative disorder to get medical help quickly. Myeloproliferative neoplasms (MPNs) show up in different ways. Knowing the signs helps both patients and doctors.
Common Physical Symptoms
People with myeloproliferative disorders often feel tired, weak, and lose weight. They might also have:
- Fatigue and weakness
- Weight loss
- Abdominal pain or discomfort, often due to an enlarged spleen
- Bone pain
- Shortness of breath
These symptoms can really affect a person’s life. They might make someone want to see a doctor.
Systemic Manifestations
MPNs can also cause other symptoms. These include:
- Fever
- Night sweats
- General malaise
These signs can show how serious the disorder is.
When to Seek Medical Attention
If symptoms don’t go away or get worse, it’s time to see a doctor. Catching the disorder early can make a big difference in treatment.
| Symptom | Possible Indication |
| Persistent fatigue | Anemia or bone marrow dysfunction |
| Unexplained weight loss | Metabolic changes or disease progression |
| Abdominal pain | Splenomegaly (enlarged spleen) |
If you or someone you know has these symptoms, seeing a doctor is key. They can help figure out what’s going on and how to treat it.
Initial Medical Evaluation Process
When doctors think Myeloproliferative Neoplasms might be present, they start a detailed check-up. This step is key to finding out if these disorders are there. It also sets the stage for more tests to come.
Medical History Assessment
The first step is a deep dive into the patient’s medical history. Doctors ask about symptoms, how long they’ve lasted, and what makes them better or worse. They also look at past health issues and family history for blood disorders.
This helps doctors spot patterns or risks linked to Myeloproliferative Neoplasms.
Physical Examination Findings
The physical exam is another vital part of the initial check. Doctors search for signs like an enlarged spleen or liver. These signs can point to Myeloproliferative Neoplasms and guide further tests.
Preliminary Screening Tests
Preliminary screening tests are key to spotting blood cell count issues. These might hint at Myeloproliferative Neoplasms. Tests like a Complete Blood Count (CBC) and a blood smear examination are used. The CBC shows blood cell levels, and the blood smear looks at cell shape.
These tests help doctors decide if more tests are needed. They also help pick the right tests to run next.
Complete Blood Count Analysis in Diagnosis
The complete blood count (CBC) test is key in diagnosing myeloproliferative neoplasms. It measures blood cell levels, giving vital info for diagnosing MPNs.
Red Blood Cell Abnormalities
Red blood cell issues are a big clue in diagnosing some MPNs. For example, polycythemia vera (PV) shows too many red blood cells, causing blood to thicken and raising the risk of blood clots. Some people might have anemia, showing a drop in red blood cell production or function.
White Blood Cell Count Significance
The white blood cell count is also very important in CBC tests. A high count, or leukocytosis, can point to chronic myeloid leukemia (CML) or other MPNs. It’s key to match this with other signs to figure out the exact MPN.
Platelet Count Abnormalities
Platelet count issues are also key in diagnosing MPNs. Essential thrombocythemia (ET) shows a high platelet count, raising the risk of blood clots. Some might have low platelet counts, linked to myelofibrosis or other bone marrow problems.
Blood Smear Examination
A blood smear is a big part of CBC tests. It shows blood cell shapes, revealing signs like teardrop cells or nucleated red blood cells seen in myelofibrosis. Seeing immature granulocytes or blasts can also hint at an MPN.
In short, a detailed CBC test, including blood cell and platelet counts, and a blood smear, is vital for diagnosing MPNs. These findings help guide more tests and treatment plans.
Genetic Testing for Myeloproliferative Disorder
Genetic testing is key in diagnosing myeloproliferative neoplasms (MPNs). It finds specific genetic mutations linked to MPNs. This lets doctors make accurate diagnoses and plan treatments.
JAK2 Gene Mutation Testing
The JAK2 V617F mutation is common in MPNs, like polycythemia vera (PV). JAK2 gene mutation testing spots this mutation. It helps diagnose PV and other MPNs.
CALR Exon9 Mutation Analysis
CALR exon9 mutations are found in MPNs, like essential thrombocythemia (ET) and primary myelofibrosis (PMF). CALR exon 9 mutation analysis finds these mutations. It helps diagnose ET and PMF.
MPL Mutation Testing
MPL mutations are linked to MPNs, mainly ET and PMF. MPL mutation testing finds these mutations. It gives valuable information for diagnosis and treatment.
Myeloproliferative Neoplasm Panel
A myeloproliferative neoplasm panel tests multiple genes linked to MPNs, like JAK2, CALR, and MPL. It spots specific genetic mutations. This helps doctors make accurate diagnoses and plan treatments.
Genetic testing in MPN diagnosis has many benefits:
- Accurate diagnosis: It finds specific genetic mutations linked to MPNs.
- Targeted treatment: It lets doctors plan treatments based on genetic mutations.
- Risk assessment: It helps assess the risk of disease progression and transformation.
Bone Marrow Biopsy and Aspiration
Bone marrow biopsy and aspiration are key for understanding myeloproliferative neoplasms (MPNs). They remove bone marrow tissue and cells for examination. This helps doctors see how the marrow is doing.
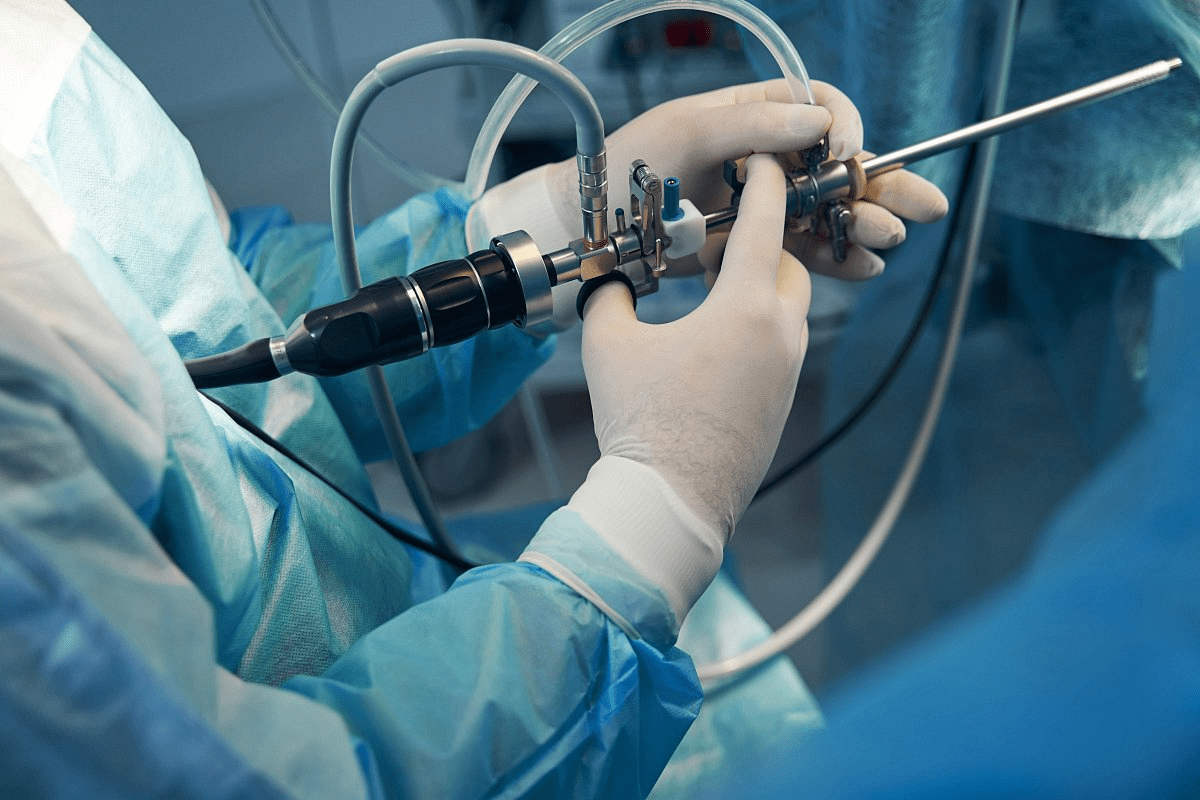
The Procedure Process
The bone marrow biopsy and aspiration are done together. The biopsy takes a small bone piece to check the marrow’s structure. Aspiration gets marrow cells. Both are done under local anesthesia.
The process starts with the patient getting comfortable. The skin is cleaned and numbed. A needle is used to take a marrow sample. For the biopsy, a bigger needle removes a bone piece.
Interpreting Bone Marrow Results
Understanding bone marrow results needs expertise. It involves looking at cell count, shape, and marrow structure. Results can show blood cell issues, fibrosis, or cancer cells.
A normal result means the marrow works well. An abnormal result might show cell or fibrosis changes. These could mean an MPN.
When Bone Marrow Biopsy is Negative
A negative bone marrow biopsy doesn’t always mean no MPN. The disease might be scattered, or the sample might miss it. Other tests are needed for a clear diagnosis.
Bone Marrow Histology Findings
Bone marrow histology findings are key. They show the marrow’s structure, like fibrosis and cell count. These details help diagnose and classify MPNs.
These findings can spot specific MPN types, like polycythemia vera or primary myelofibrosis. Knowing these details is important for correct diagnosis and treatment.
Diagnostic Criteria for Specific Myeloproliferative Neoplasms
The World Health Organization (WHO) has a clear guide for diagnosing MPNs like PV, ET, PMF, and CML. This guide uses clinical signs, lab results, and genetic tests to confirm a diagnosis.
Polycythemia Vera Diagnostic Criteria
To diagnose polycythemia vera (PV), doctors look for certain signs. These include hemoglobin or hematocrit levels above normal, the JAK2 mutation, and a bone marrow that’s too full. They also check for low serum erythropoietin levels.
Essential Thrombocythemia Diagnosis
Essential thrombocythemia (ET) is identified by sustained thrombocytosis and specific genetic markers like JAK2, CALR, or MPL. Doctors also rule out other reasons for high platelet counts.
Primary Myelofibrosis Diagnosis
Diagnosing primary myelofibrosis (PMF) involves several steps. These include bone marrow fibrosis, a clonal marker, and symptoms like splenomegaly. The WHO criteria also exclude other myeloid neoplasms.
Chronic Myeloid Leukemia Diagnosis
Chronic myeloid leukemia (CML) is identified by the Philadelphia chromosome or BCR-ABL1 gene. Doctors look for elevated white blood cell counts and the BCR-ABL1 transcript.
Accurate diagnosis of MPNs is key to the right treatment and better patient outcomes. A detailed diagnostic process, including genetic tests and bone marrow exams, is vital for identifying the correct MPN type.
Advanced Imaging in Diagnosis
Advanced imaging is key in diagnosing MPNs. These methods give us important details about the spleen and liver. These organs are often affected by myeloproliferative neoplasms.
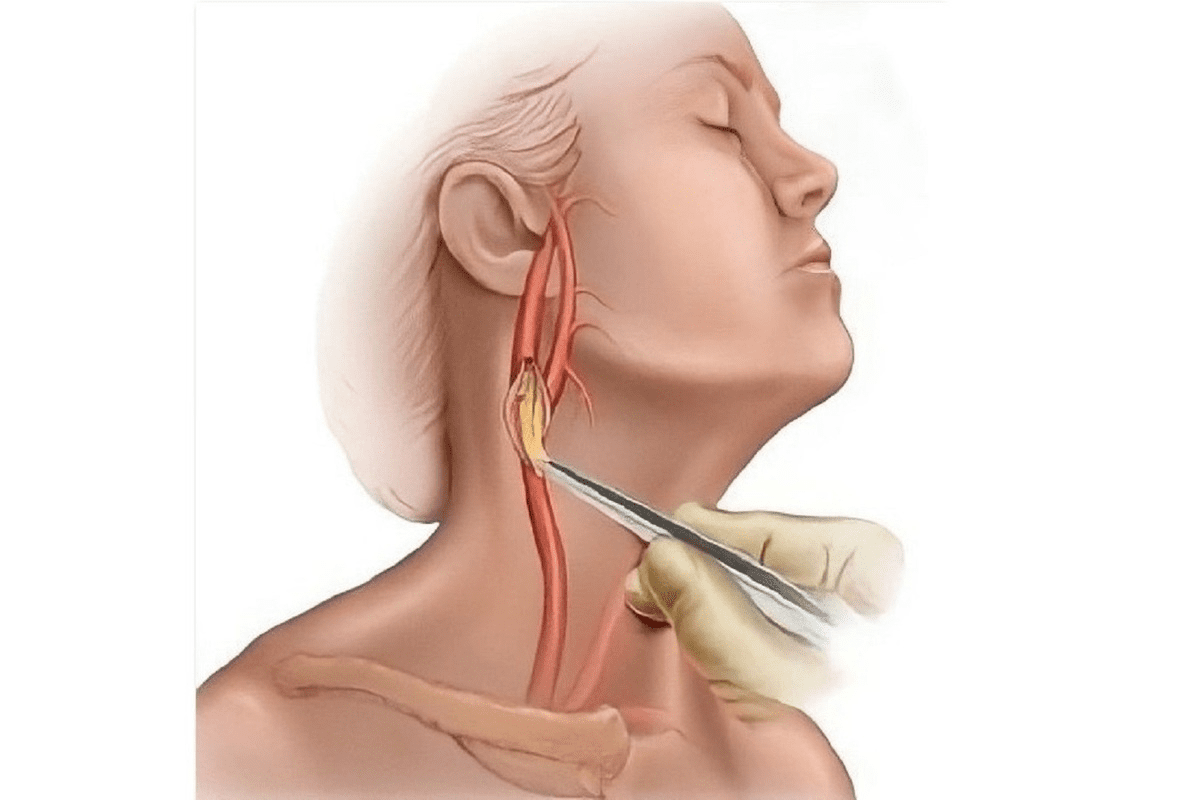
Ultrasound Assessment of Spleen and Liver
Ultrasound is a non-invasive way to check spleen size and liver shape. It’s great for spotting splenomegaly, a common sign in many MPNs.
CT and MRI Applications
CT and MRI scans give us more detailed views of the spleen and liver. They help spot structural issues and see how far the disease has spread.
Key applications include:
- Assessing spleen size and texture
- Evaluating liver morphology and detecting focal lesions
- Guiding diagnostic and therapeutic interventions
Nuclear Medicine Studies
Nuclear medicine studies, like bone marrow scintigraphy, show us how the bone marrow works and where it is. This info is vital for diagnosing and managing MPNs.
| Imaging Modality | Primary Use in MPN Diagnosis | Key Benefits |
| Ultrasound | Spleen size assessment, liver morphology | Non-invasive, quick, and cost-effective |
| CT/MRI | Detailed spleen and liver assessment | High-resolution images detect structural abnormalities |
| Nuclear Medicine | Bone marrow function and distribution | Provides functional information, aids in disease staging |
Differential Diagnosis Considerations
Diagnosing myeloproliferative neoplasms (MPNs) can be tricky because they look like other blood disorders. It’s important to tell them apart from other conditions. This is called differential diagnosis.
Secondary Causes of Blood Cell Abnormalities
When checking for MPNs, we must think about other reasons for blood cell problems. Things like infections, inflammation, and some medicines can mess with blood counts. For example, too many red blood cells can happen because of low oxygen or tumors.
Other Hematologic Disorders
We also need to look at other blood diseases when diagnosing MPNs. Leukemia and lymphoma can look similar to MPNs. For example, chronic myeloid leukemia (CML) can have high white blood cell counts like some MPNs.
To tell them apart, we do genetic tests and check the bone marrow.
Distinguishing Between MPN Types
It’s important to know the difference between different MPNs to treat them correctly. The main types are polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF). Each has its own signs and treatment.
For example, PV means you have too many red blood cells. ET means you have too many platelets. Knowing these differences helps doctors give the right treatment.
In short, figuring out what kind of MPN someone has is a big deal. By looking at other blood problems, other diseases, and the different types of MPNs, doctors can make sure they diagnose and treat correctly.
The Role of Hematologists in Diagnosis
Hematologists are key in diagnosing myeloproliferative disorders. They are medical experts who handle blood disorders, including myeloproliferative neoplasms (MPNs). Their knowledge is essential for the complex process of diagnosing MPNs.
When to Consult a Hematologist
If you think you might have MPNs, see a hematologist. They should be seen if initial tests show odd blood cell counts or if symptoms of MPNs appear.
A study in the Journal of Clinical Oncology found that seeing a hematologist early improves diagnosis and care.
The involvement of hematologists in the diagnostic process is critical for accurate diagnosis and effective management of MPNs.
The Diagnostic Workup Process
The process to diagnose involves a detailed medical history, physical check-up, lab tests, and sometimes genetic tests. Hematologists use this data to figure out if you have an MPN and what type it is.
- Comprehensive medical history assessment
- Physical examination to detect signs such as splenomegaly
- Laboratory tests, including complete blood count (CBC) and blood smear examination
- Genetic testing for mutations such as JAK2, CALR, and MPL
| Diagnostic Test | Purpose |
| Complete Blood Count (CBC) | To assess blood cell counts and detect abnormalities |
| Blood Smear Examination | To examine the morphology of blood cells |
| Genetic Testing | To identify specific mutations associated with MPNs |
Specialized Testing Centers
Specialized testing centers offer advanced tests like molecular genetic testing. These places have the latest technology and experts in hematopathology.
Hematologists are essential in diagnosing and managing MPNs. Their skills ensure patients get the right diagnosis and treatment.
Understanding Diagnostic Test Results
Getting the most out of diagnostic test results is vital for managing MPNs. These tests give us key info on genetic mutations and blood cell health.
Interpreting JAK2 Test Results
The JAK2 V617F mutation test is a key tool in diagnosing MPNs. It checks for a specific JAK2 gene mutation linked to MPNs like polycythemia vera and essential thrombocythemia.
Key aspects of JAK2 test results:
- A positive result shows the JAK2 V617F mutation is present.
- A negative result doesn’t mean you can’t have an MPN.
- The test is part of a bigger set of criteria to confirm an MPN diagnosis.
What Positive and Negative Results Mean
It’s important to understand what positive and negative test results mean. This knowledge helps both patients and doctors.
Positive results for genetic mutations like JAK2 V617F confirm an MPN. But these results must be looked at with other diagnostic findings and the patient’s overall health.
Negative results don’t always mean you don’t have an MPN. Some patients might have other mutations or traits not caught by one test.
Laboratory Values in MPNs
Laboratory values, like those from a complete blood count (CBC), are key in diagnosing and managing MPNs.
| Laboratory Test | Normal Range | MPN Implications |
| White Blood Cell Count | 4,500-11,000/μL | Elevated counts may indicate MPN or other conditions. |
| Red Blood Cell Count | Male: 4.32-5.72 million cells/μL; Female: 3.90-5.03 million cells/μL | Abnormalities can indicate polycythemia vera or other MPNs. |
| Platelet Count | 150,000-450,000/μL | Thrombocytosis may be associated with essential thrombocythemia. |
Understanding these lab values in the context of a patient’s health and medical history is key. It helps in accurate diagnosis and effective MPN management.
Diagnostic Challenges and Limitations
Diagnosing Myeloproliferative Neoplasms (MPNs) is tough because of their complexity. The process is made harder by similar symptoms in different MPNs and changing diagnostic rules.
Overlapping Symptoms Between MPN Types
One big challenge is that symptoms like fatigue and splenomegaly can show up in many MPNs. This makes it hard to tell them apart just by looking at symptoms.
This similarity can cause delays in getting a diagnosis. A detailed diagnostic process, including lab tests and genetic analysis, is needed to accurately identify MPNs.
Evolving Diagnostic Criteria
The rules for diagnosing MPNs have changed over time. Now, genetic markers like JAK2 are used, making diagnosis more precise.
But these changes also bring challenges. Doctors need to keep up with new guidelines and research. This means they must stay educated and aware of the latest findings.
| Diagnostic Criteria | Previous Guidelines | Current Guidelines |
| Genetic Mutations | Limited to JAK2 V617F | Includes JAK2, CALR, and MPL mutations |
| Bone Marrow Biopsy | Required for diagnosis | Still essential, with increased emphasis on molecular analysis |
| Clinical Features | Focused on splenomegaly and thrombocytosis | Encompasses a broader range of symptoms and laboratory findings |
Unclassifiable Myeloproliferative Neoplasms
Some patients don’t fit into any specific MPN category. This is often because of early disease, overlap, or rare genetic mutations. Such cases are called unclassifiable MPNs.
Dealing with unclassifiable MPNs is tricky. There’s not much research to guide treatment. Doctors must use their knowledge and available data to make treatment plans.
Post-Diagnosis Classification and Risk Stratification
After getting a diagnosis of a myeloproliferative neoplasm, the next step is to classify and stratify the risk. This is key to predicting how the disease will progress and planning treatment. It involves a detailed look to figure out the exact type of MPN and its risks.
Prognostic Scoring Systems
Prognostic scoring systems are important for predicting patient outcomes. The International Prognostic Scoring System (IPSS) is a widely used tool for assessing prognosis in some MPNs. The Dynamic IPSS (D-IPSS) also offers insights by looking at changes in clinical data over time.
- The IPSS score helps in stratifying patients into different risk categories.
- D-IPSS provides a more dynamic assessment by considering changes in clinical parameters over time.
Risk Assessment Tools
Risk assessment tools are key for evaluating the chance of disease progression and complications. They look at genetic mutations, blood counts, and symptoms to give a full risk profile.
- Genetic testing for mutations such as JAK2, CALR, and MPL.
- Assessment of blood cell counts and other hematological parameters.
- Evaluation of clinical symptoms and signs, such as splenomegaly.
Impact on Treatment Planning
The results of post-diagnosis classification and risk stratification greatly affect treatment planning. Understanding the specific risks of an MPN helps healthcare providers tailor treatments. This ensures the most critical aspects of the disease are addressed.
Treatment plans can include various interventions. This includes pharmacological therapies to reduce disease activity and supportive care to improve quality of life. The choice of treatment depends on the risk category and the specific characteristics of the MPN.
Conclusion: Navigating Your Diagnostic Journey
Understanding Myeloproliferative Neoplasms (MPNs) is tough. Getting a correct diagnosis needs a detailed plan. This includes many tests and checks.
It’s important for patients to team up with their doctors. Hematologists play a key role in managing MPNs. Knowing about the diagnostic steps helps patients handle their journey better.
Being well-informed helps patients grasp their diagnosis and treatment options. Working together with doctors is key. This teamwork is essential for the best results in treating MPNs.
FAQ
What is a myeloproliferative disorder?
Myeloproliferative disorders are blood cancers. They cause too many blood cells to be made.
What are the common types of myeloproliferative neoplasms?
The main types are polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF).
What are the early signs and symptoms of myeloproliferative disorder?
Early signs include fatigue, weight loss, and stomach pain. Other symptoms are fever, night sweats, and bone pain.
How is a complete blood count (CBC) used in the diagnosis of myeloproliferative disorder?
A CBC checks blood cell levels. It shows if there are too many red or white blood cells or platelets.
What is the significance of JAK2 gene mutation testing in myeloproliferative disorder?
The JAK2 V617F mutation is common in myeloproliferative neoplasms. It’s often found in polycythemia vera.
What is a bone marrow biopsy and aspiration?
These are tests to remove bone marrow tissue. They help diagnose myeloproliferative neoplasms.
How are myeloproliferative neoplasms classified and risk-stratified after diagnosis?
Systems like the International Prognostic Scoring System (IPSS) are used. They help predict patient outcomes.
What is the role of hematologists in the diagnosis of myeloproliferative disorder?
Hematologists specialize in blood disorders. They diagnose and manage myeloproliferative neoplasms.
What are the diagnostic challenges and limitations in myeloproliferative neoplasms?
Challenges include symptoms that overlap between types. There are also evolving criteria and unclassifiable cases.
How are diagnostic test results interpreted in myeloproliferative neoplasms?
Test results are looked at with the patient’s symptoms and history in mind.
What is the impact of post-diagnosis classification and risk stratification on treatment planning?
These results affect treatment plans and outcomes.
References
- Choi, C. W. (2015). Guidelines for the management of myeloproliferative neoplasms. Blood research, 50(4), 180-187. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4642006/