
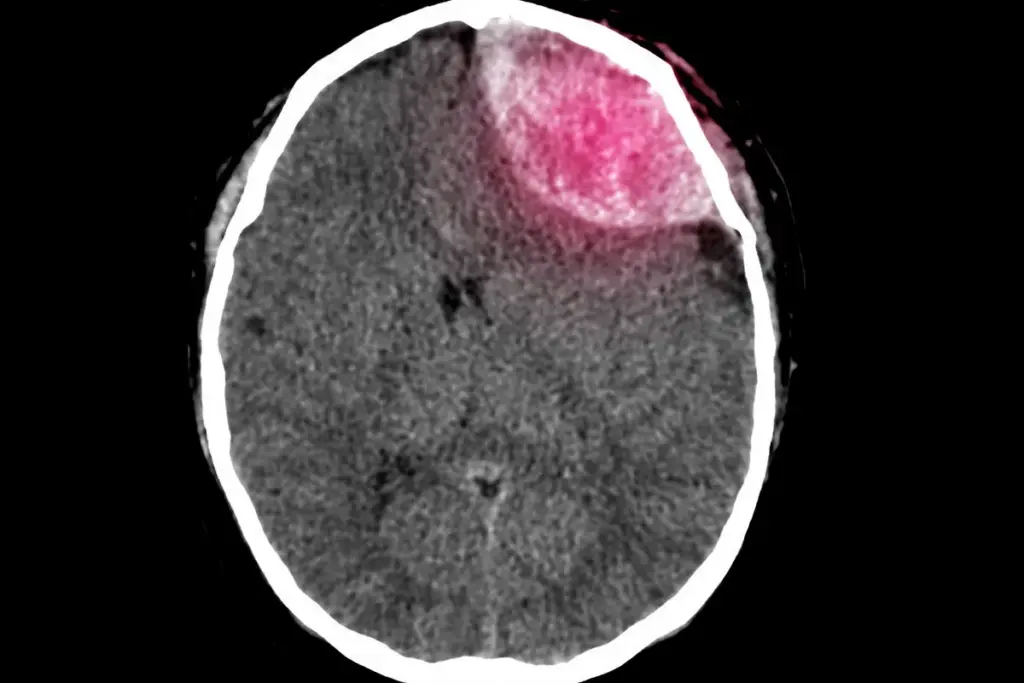
Brain surgery is a complex medical procedure. It treats serious conditions like tumors, blood clots, and epilepsy. The risks and complexity make it a daunting choice for many.
There are many types of brain surgery, each with its own risks. Some are considered major surgeries because they’re very complex. These surgeries involve critical brain areas or require removing a lot of brain tissue.
Key Takeaways
- Brain surgery treats various conditions like tumors, blood clots, and epilepsy.
- The complexity of brain surgery poses significant risks to patients.
- Major surgeries involving critical brain areas are considered riskiest.
- Procedures like aneurysm clipping and tumor removal are common brain surgeries.
- Understanding the risks is crucial for patients considering brain surgery.
The Complexity and Dangers of Neurosurgical Procedures
Neurosurgical procedures are complex and risky. They involve delicate operations that can greatly affect a patient’s life. The complexity of these procedures is a big reason for their risks.
Why Brain Surgery Carries Inherent Risks
Brain surgery is risky because of the brain’s delicate nature. The brain controls many body functions. Damage can lead to serious problems, like speech or vision issues.
Some risks of brain surgery include:
- Bleeding or hemorrhage
- Infection
- Blood clots
- Stroke or cerebral vasospasm
- Damage to surrounding brain tissue
These risks are made worse by the complexity of neurosurgical procedures. These surgeries often involve navigating through delicate brain structures.
“The brain is a complex and dynamic system, and neurosurgery requires a deep understanding of its anatomy and function.” –
A renowned neurosurgeon
Mortality and Morbidity Statistics in Neurosurgery
Mortality and morbidity rates in neurosurgery depend on the procedure, patient condition, and surgeon’s experience. Studies show mortality rates range from 0.5% to 5%. Morbidity rates can be up to 20%.
|
Procedure Type |
Mortality Rate (%) |
Morbidity Rate (%) |
|---|---|---|
|
Craniotomy |
1.2 – 3.5 |
5 – 15 |
|
Spinal Surgery |
0.5 – 2 |
3 – 10 |
|
Brain Tumor Resection |
2 – 5 |
10 – 20 |
These statistics show the need for careful planning, precise execution, and thorough post-operative care in neurosurgery.
Brain Stem Surgery: The Most Precarious Neurosurgical Frontier

Surgery on the brain stem is very complex. It’s because it controls breathing, heart rate, and blood pressure. The brain stem connects the cerebrum to the spinal cord. It’s key for many automatic body functions.
Critical Functions Controlled by the Brain Stem
The brain stem handles several important tasks, including:
- Regulating heart rate and blood pressure
- Controlling breathing and respiratory rate
- Managing sleep and arousal
- Facilitating the transmission of signals between the brain and the rest of the body
Because of its vital role, surgery here is very challenging. Neurosurgeons must be very careful to avoid harming the brain stem’s delicate parts.
Why Mortality Rates Remain High
Even with better neurosurgical methods, brain stem surgery still has high death rates. This is because of several reasons:
|
Factor |
Description |
Impact on Mortality |
|---|---|---|
|
Location |
The brain stem’s critical location makes surgical access challenging. |
High risk of damage to vital structures. |
|
Delicacy of Structures |
The brain stem contains delicate neural structures crucial for survival. |
Increased risk of post-operative complications. |
|
Surgical Precision |
The need for extreme precision during surgery. |
Minor errors can lead to significant morbidity or mortality. |
It’s important for neurosurgeons and patients to understand these challenges. New surgical methods and technology help improve results. But, the risks of brain stem surgery mean careful thought and planning are needed.
Cerebral Aneurysm Clipping: Racing Against Rupture
Cerebral aneurysm clipping is a delicate and risky procedure. It aims to secure blood vessels to prevent rupture. This process is both urgent and carries significant risks.
The Delicate Process of Securing Blood Vessels
Securing blood vessels in cerebral aneurysm clipping needs precision and finesse. Neurosurgeons must carefully navigate the brain’s vascular anatomy. They aim to find and isolate the aneurysm.
This involves:
- Careful dissection to expose the aneurysm
- Temporary clipping to control blood flow
- Permanent clipping to exclude the aneurysm from the circulation
The goal is to remove the aneurysm without harming nearby brain tissue or blood vessels. This is a tough task, as the aneurysm is often close to vital areas.
Complications and Emergency Scenarios
Even with skilled neurosurgeons, complications can happen during cerebral aneurysm clipping. These may include:
- Rupture of the aneurysm during surgery
- Vasospasm or thrombosis of surrounding blood vessels
- Injury to adjacent neural structures
In emergencies, neurosurgeons must act quickly to reduce damage. They might use emergency clipping, vasodilator therapy, or other treatments to stabilize the patient.
Understanding cerebral aneurysm clipping and its risks helps us prepare for complications. This way, we can better handle the challenges of this complex procedure.
Arteriovenous Malformation (AVM) Resection: Untangling the Vascular Web
AVM resection is a complex surgery. It removes abnormal connections between arteries and veins in the brain. These malformations can cause serious health problems, like bleeding and brain damage.
Challenges of High-Flow Blood Vessels
Dealing with high-flow blood vessels is a big challenge in AVM resection. “High-flow AVMs are risky because of the fast blood flow,” says a top neurosurgeon. This fast flow can cause aneurysms and bleeding during surgery.
Spetzler-Martin Grading System and Risk Assessment
The Spetzler-Martin Grading System helps assess AVM resection risks. It looks at the AVM’s size, location, and how it drains blood. This helps predict surgery complications.
- Grade I: Small, easy-to-resect AVMs.
- Grade II: Larger AVMs or those with deep venous drainage, presenting moderate surgical challenges.
- Grade III: AVMs with a higher risk profile due to their size, location, or other factors.
- Grade IV and V: Large, complex AVMs with significant risks associated with their resection.
Risk assessment is key in AVM resection. Surgeons use the Spetzler-Martin Grading System and other tools to plan surgery. They look at the AVM’s anatomy, the patient’s health, and other factors to reduce risks.
Understanding high-flow blood vessels and using the Spetzler-Martin Grading System helps surgeons. They can better plan and achieve success in untangling the vascular web during AVM resection.
Awake Craniotomy: Surgery While Conscious
Brain surgery can sometimes need an awake craniotomy. This means the patient stays awake and alert. It’s a complex surgery that lets neurosurgeons work on the brain while the patient is awake.
This method is key for surgeries near areas that control important functions. These include speech, movement, and feeling sensations.
Mapping Brain Function in Real-Time
During an awake craniotomy, the brain’s functions are mapped live. Surgeons stimulate different brain areas to see what they do. Real-time mapping helps them avoid harming important brain spots.
Neurosurgeonsays, “Awake craniotomy has changed how we safely remove tumors near important brain areas.” It makes surgery more precise and improves patient results by protecting vital brain functions.
Psychological and Physical Challenges
Being awake during surgery is tough for patients. It requires careful setup and watching to keep them safe and comfortable. Patients must stay still and listen carefully, which is hard.
Deep Brain Tumor Resection: Reaching the Unreachable
Removing deep-seated brain tumors is a complex task. It needs precision, advanced tech, and a deep understanding of the brain. We’ll look at the surgical methods used, the challenges of reaching these tumors, and the risks involved.
Surgical Approaches to Deep-Seated Tumors
Surgeons use different surgical approaches to get to deep brain tumors. Each method has its own challenges and things to consider. The approach depends on the tumor’s location, size, and the patient’s health.
Advanced imaging, like intraoperative MRI, is key. It helps navigate the brain’s complex structures. This ensures the tumor is removed completely.
One big challenge is avoiding damage to the surrounding brain. Neurosurgeons plan carefully and use real-time imaging. Minimally invasive techniques can also help. They might reduce recovery time and lower the risk of complications.
Risk of Permanent Neurological Damage
Deep brain tumor resection comes with a big risk of permanent neurological damage. Tumors near important brain areas mean small mistakes can have big effects. Patients and their families need to understand these risks before surgery.
There’s also a chance of severe postoperative pain and other issues like infection or swelling. A good care plan, including pain management and rehab, is crucial for the best results.
Hemispherectomy: Removing Half the Brain
For those with severe seizure conditions, hemispherectomy can be a game-changer. This rare surgery removes or disconnects half of the brain. It’s considered for those with epilepsy that hasn’t improved with other treatments.
Indications for This Extreme Procedure
Hemispherectomy is for severe seizure disorders that don’t respond to other treatments. Conditions like Rasmussen’s encephalitis and hemimegalencephaly might lead to this surgery. Doctors and families discuss it after careful evaluation.
Long-term Outcomes and Adaptation
Results of hemispherectomy vary. Some see a big drop or stop in seizures. Others might still have seizures but less often or severe. The surgery can lead to neurological issues, but many adapt well.
Important things to know about hemispherectomy include:
- The surgery can be anatomical (removing half) or functional (disconnecting half).
- Before surgery, imaging and EEG studies are done to check the seizure focus.
- After surgery, intensive rehab helps patients adjust to any new challenges.
In summary, hemispherectomy is a complex surgery for severe seizures. It’s risky but can change lives for those who get it.
Most Painful Surgery: Brain Procedures and Pain Experience
Some brain surgeries are very painful, affecting patients’ recovery and life quality. The pain after brain surgery can vary a lot. It depends on the type of surgery done.
Factors Contributing to Extreme Discomfort
Many things can make pain after brain surgery worse. The surgery’s location and how complex it is matter a lot. Surgeries that cut more tissue or are near sensitive areas usually hurt more.
The way the surgery is done and how big the hole in the skull is also play a part. We’ll look into these details to see why some brain surgeries hurt more.
Post-Craniotomy Pain Syndrome
Post-craniotomy pain syndrome is a problem after some brain surgeries. It’s chronic pain that lasts long after the wound heals.
The reasons for this pain are not fully known. It’s thought to be from nerve damage, inflammation, and how sensitive a person is.
Managing post-craniotomy pain syndrome needs a full plan. This includes medicines, physical therapy, and sometimes more surgery.
Knowing the pain risks of different brain surgeries is key. It helps both patients and doctors make better choices about treatment.
Intraventricular Tumor Surgery: Navigating the Brain’s Inner Chambers
Intraventricular tumor surgery is a complex field in neurosurgery. It needs a lot of precision and skill. Tumors in the brain’s ventricular system are hard to reach because they are close to important brain parts and CSF pathways.
We will look into how to get to these tumors and the risks. This includes problems with CSF flow and the chance of hydrocephalus.
Accessing Tumors Within the Ventricular System
The ventricular system is a network of fluid-filled spaces in the brain. Tumors here can block CSF flow. This can cause high pressure in the brain and other issues. Getting to these tumors surgically is a big challenge.
Surgical Approaches: There are different ways to reach these tumors. These include going through the brain’s surface or through the corpus callosum. The best method depends on the tumor’s size, location, and the patient’s brain.
|
Surgical Approach |
Description |
Advantages |
Disadvantages |
|---|---|---|---|
|
Transcortical |
Access through the cerebral cortex |
Direct access to certain tumor locations |
Risk of cortical damage |
|
Transcallosal |
Access through the corpus callosum |
Less cortical disruption |
Risk of damage to the corpus callosum |
Risks of CSF Disruption and Hydrocephalus
One big risk of this surgery is messing with CSF flow. This can cause hydrocephalus. It’s when CSF builds up in the brain, leading to high pressure.
Management of CSF Disruption: To avoid these problems, doctors use special tools. They might use external ventricular drains or shunt systems to help with CSF flow after surgery.
In conclusion, surgery for tumors in the brain’s ventricular system is very complex. It needs careful planning and skill. Knowing the risks and challenges is key for both doctors and patients.
Skull Base Surgery: Operating at the Brain’s Foundation
The skull base is a complex area. Surgery here needs precision and skill. It involves removing tumors at the skull’s base, near vital nerves and blood vessels.
Challenges of Accessing Tumors at the Cranial Base
Getting to tumors at the cranial base is hard. The skull base is a tight space with complex anatomy. Surgeons face challenges due to nearby vital structures like nerves and blood vessels.
The skull base’s anatomy is intricate. Tumors here can be benign or cancerous. They often need a team of experts for treatment.
Critical Neurovascular Structures at Risk
Neurovascular structures are at risk in skull base surgery. These delicate structures need careful surgery to avoid harm. Problems can include stroke, nerve damage, and other brain issues.
At risk are cranial nerves and major arteries. Damage can lead to facial paralysis, vision loss, and swallowing problems.
Skull base surgery is very complex. It needs a skilled neurosurgical team. Knowing the challenges and risks is key for both doctors and patients.
Factors That Increase Surgical Risk in Brain Procedures
Surgical risks in brain procedures come from many sources. These include factors specific to the patient and the tumor itself. Knowing these factors is key for neurosurgeons to perform surgeries well. We will look at these risks in depth, showing how they affect surgery results.
Patient-Specific Risk Factors
Patient-specific factors greatly affect brain surgery risks. These include:
- Age: Older patients face higher risks because of less physical strength and health issues.
- Overall Health: Conditions like diabetes, high blood pressure, and heart disease can make surgery harder and recovery slower.
- Previous Surgeries or Treatments: Patients who have had brain surgeries or radiation before may face more complications.
Tumor Characteristics That Complicate Surgery
The type of tumor being treated also affects surgery risks. Important factors include:
- Tumor Location: Tumors in hard-to-reach brain areas make surgery more complex and risky.
- Tumor Size and Growth Pattern: Bigger tumors or those growing fast need more surgery, raising the risk of problems.
- Vascularity: Tumors with lots of blood vessels can increase the risk of bleeding during surgery.
In summary, both patient-specific factors and tumor characteristics are vital in determining brain surgery risks. By understanding these, neurosurgeons can plan and manage these risks better.
Recovery and Rehabilitation After High-Risk Brain Surgery
The journey to recovery after high-risk brain surgery is complex. It involves both immediate care and long-term rehabilitation. Understanding the challenges and support needed is key.
Immediate Post-Operative Complications
Patients are closely watched in intensive care units after surgery. They are at risk for complications like swelling, infection, or bleeding. Managing these complications is vital for a good recovery.
Some complications include:
- Cerebral edema or swelling
- Infection
- Hemorrhage or bleeding
- Seizures
- Hydrocephalus
A team of experts is needed to handle these issues. This team includes neurosurgeons, intensivists, nurses, and rehabilitation specialists.
Long-term Rehabilitation Needs
Rehabilitation is crucial for patients after high-risk brain surgery. The type and length of rehab depend on the surgery, the patient’s condition before surgery, and any complications.
Rehabilitation may include:
- Physical therapy to regain strength and mobility
- Occupational therapy to relearn daily living skills
- Speech therapy for patients with communication difficulties
- Cognitive rehabilitation to address memory and concentration issues
A tailored rehabilitation plan is essential. It helps meet each patient’s unique needs, improving their quality of life.
Advances in neurosurgery and care are important. But, comprehensive rehabilitation remains a key to better outcomes after high-risk brain surgery.
Modern Techniques Reducing Neurosurgical Risks
Modern neurosurgery has made big strides with new technologies. These advancements help make surgeries safer and more precise. This is a big win for patients.
Intraoperative MRI and Navigation Systems
Intraoperative MRI and navigation systems are key in modern neurosurgery. They let surgeons see the brain’s details in real-time. This helps them remove tumors more accurately and safely.
With intraoperative MRI, surgeons can see how much of the tumor they’ve removed. They can then make changes during the surgery. Navigation systems help plan the surgery and guide it, making it more precise.
Minimally Invasive and Endoscopic Approaches
Minimally invasive and endoscopic techniques have changed neurosurgery a lot. They cause less damage and pain, and patients recover faster. These methods use smaller cuts and disturb the brain less.
Endoscopic surgery is especially useful. It treats some conditions through small openings, avoiding big cuts. This lowers the chance of infection and brain damage.
|
Technique |
Benefits |
Applications |
|---|---|---|
|
Intraoperative MRI |
Real-time imaging, precise resection |
Tumor surgery, complex lesion removal |
|
Navigation Systems |
Enhanced accuracy, preoperative planning |
Various neurosurgical procedures |
|
Minimally Invasive Surgery |
Less tissue trauma, quicker recovery |
Blood vessel malformations, certain tumors |
|
Endoscopic Approaches |
Smaller incisions, reduced risk |
Pituitary tumors, certain brain cysts |
Using these modern methods, we can greatly lower the risks of neurosurgery. This leads to better results for patients and a better life for them.
Choosing a Neurosurgeon: The Impact of Surgical Experience
When it comes to complex brain surgery, the neurosurgeon’s experience is key. It greatly affects the outcome. Patients facing high-risk brain surgeries should pick a neurosurgeon with lots of experience.
Choosing a neurosurgeon is a big decision. It can greatly affect the success of the surgery. The volume-outcome relationship shows that more surgeries lead to better results.
Volume-Outcome Relationship in Complex Brain Surgery
Studies show that more surgeries mean fewer complications and deaths. This is true for brain surgery too. So, picking a neurosurgeon with lots of experience is crucial.
|
Surgical Volume |
Mortality Rate |
Complication Rate |
|---|---|---|
|
Low Volume |
5% |
15% |
|
High Volume |
2% |
8% |
Questions to Ask Before High-Risk Procedures
Before high-risk brain surgery, ask your neurosurgeon about their experience. Important questions include: “How many times have you done this surgery?” “What are your complication and mortality rates?” and “How do you reduce risks during and after surgery?”
These questions help you understand your neurosurgeon’s experience and the risks. This knowledge helps you make a better decision about your care.
It’s important to talk thoroughly with your neurosurgeon. This ensures all your concerns are heard. By choosing an experienced neurosurgeon, you improve your chances of a good outcome.
Informed Consent: Understanding the Full Spectrum of Risks
It’s key to know all the risks when getting neurosurgical care. Informed consent is more than a legal formality. It’s about giving patients the power to choose their care wisely. We think patients should know all about the risks and benefits of brain surgery.
Essential Information for Decision-Making
Brain surgery requires talking about risks, benefits, and other options. Patients need to know what the surgery is, what it can achieve, and possible problems. This includes the surgery’s risks and the risks of not doing it.
We make sure patients get all the facts they need. This includes the surgeon’s experience, the methods used, and what recovery will be like. With all the information, patients can choose what’s best for them.
Balancing Quality of Life with Surgical Intervention
Another important part of informed consent is weighing surgery’s benefits against its impact on life quality. Patients and their families must think if the surgery’s benefits are worth the risks and if it will really improve their life.
We work with patients to understand what matters most to them. This way, they can make choices that fit their unique situation and values.
Conclusion: Weighing the Risks and Benefits of Brain Surgery
Brain surgery is a complex and risky procedure. It can save lives or greatly improve them. In this article, we looked at some of the most dangerous surgeries, like brain stem surgery and clipping cerebral aneurysms.
Each surgery has its own risks and challenges. These include high mortality rates, complications, and long-term recovery needs. It’s important for patients and their families to understand these risks and benefits before making a decision.
Knowing the risks and benefits helps patients navigate brain surgery better. Modern techniques, like intraoperative MRI and navigation systems, have made outcomes better and risks lower. Choosing an experienced neurosurgeon and being aware of risk factors can also lead to a successful surgery.
In the end, brain surgery is a crucial option for treating serious conditions. By understanding the risks and benefits, we can work together to get the best results for patients going through these complex surgeries.
FAQ
What is the riskiest brain surgery?
Brain stem surgery is very risky. This is because the brain stem controls important body functions. It’s a complex and delicate procedure.
What are the most painful brain surgeries?
Deep brain tumor resection and skull base surgery are very painful. They can also cause long-term pain after surgery.
What factors increase the risk of brain surgery?
Age and health can affect the risk of brain surgery. So can the size and location of the tumor.
How can risks be minimized in neurosurgical procedures?
New techniques like intraoperative MRI and navigation systems help. They make surgery safer and improve outcomes.
Why is choosing an experienced neurosurgeon crucial?
Choosing a skilled neurosurgeon is key. Their experience can greatly improve the success and safety of the surgery.
What is the significance of informed consent in brain surgery?
Informed consent is vital. It makes sure patients understand the risks and benefits. This helps them make informed decisions.
What are the challenges of recovering from high-risk brain surgery?
Recovery is tough. It involves managing immediate complications and long-term needs. A good rehabilitation plan is crucial.
What are the risks associated with AVM resection?
AVM resection is complex. It deals with high-flow blood vessels. The Spetzler-Martin Grading System helps assess risks for planning.
What is awake craniotomy, and what are its challenges?
Awake craniotomy maps brain function in real-time. It’s done while the patient is awake. It’s challenging but allows for precise surgery.
What are the indications for hemispherectomy?
Hemispherectomy is for severe conditions like some types of epilepsy. It removes half of the brain. It requires careful thought about long-term effects.
JAMA Network. Evidence-Based Medical Insight. Retrieved from https://jamanetwork.com/journals/jamasurgery/fullarticle/1392156[5





