Prostate surgery is a common treatment for prostate issues, like cancer. The choice to have this surgery depends on many factors, with age being key.
As men get older, they face a higher risk of prostate problems. Prostate surgery can be a good option, but knowing how age affects it is important.
It’s vital for both patients and doctors to understand the age limit for prostate surgery. This helps make the right treatment choices.
Key Takeaways
- The decision to undergo prostate surgery is influenced by multiple factors, including the patient’s overall health.
- Age is a critical factor in determining the suitability of prostate surgery.
- Recovery time after prostate operation varies among individuals.
- Understanding the implications of age on prostate surgery outcomes is essential.
- Patients should discuss their individual circumstances with their healthcare provider.
Understanding Prostate Surgery: An Overview
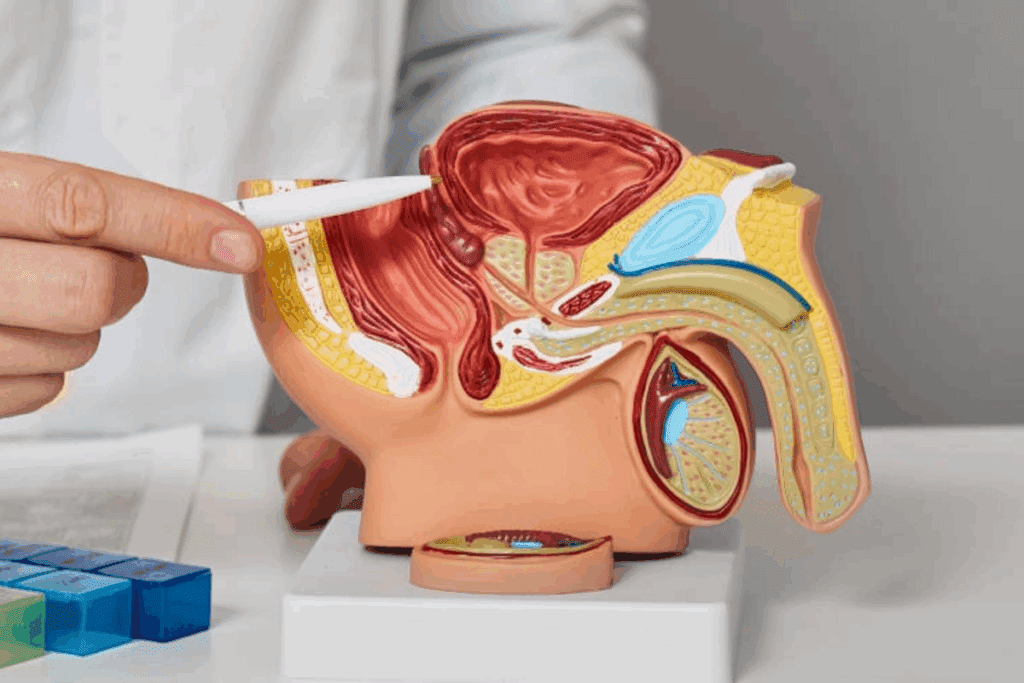
Prostate surgery is a range of treatments for prostate issues. These include prostate cancer, benign prostatic hyperplasia (BPH), and other prostate gland problems.
Choosing to have prostate surgery depends on several things. These include how severe the condition is, the patient’s health, and the surgery’s benefits and risks.
Common Types of Prostate Surgeries
There are many prostate surgeries, each with its own purpose. The most common ones are:
- Radical Prostatectomy: This surgery removes the prostate gland. It’s mainly for treating prostate cancer.
- Transurethral Resection of the Prostate (TURP): This surgery treats BPH by removing prostate tissue that blocks urine flow.
- Simple Prostatectomy: It removes the inner part of the prostate gland. This is often for BPH treatment.
Indications for Prostate Surgery
Prostate surgery is needed for several conditions. These include:
| Condition | Surgical Indication |
| Prostate Cancer | Radical Prostatectomy |
| Benign Prostatic Hyperplasia (BPH) | TURP or Simple Prostatectomy |
| Prostatitis or Prostate Abscess | Surgical drainage or other interventions |
It’s important for patients to know about the different prostate surgeries. This helps them make better choices about their treatment.
Age as a Factor in Prostate Surgery Decisions

Doctors look closely at a patient’s age when deciding if prostate surgery is right. They consider many things, with age being very important.
Chronological Age vs. Biological Age
Doctors use two types of age when checking if surgery is good for a patient. Chronological age is how old someone is in years. Biological age shows how well someone’s body is working. Both ages matter when deciding if surgery is a good choice.
A study in the Journal of Urology found that biological age is more important than chronological age for surgery results. This helps doctors make better choices for patients.
“The assessment of a patient’s biological age is essential in determining their suitability for prostate surgery, as it provides a more accurate reflection of their overall health status.”
How Age Affects Surgical Outcomes
Age can change how well surgery works. Older people might face more risks and take longer to get better. But, new surgery methods like robotic-assisted surgery help older men do better.
| Age Group | Complication Rate | Recovery Time |
| 65-70 | 15% | 6-8 weeks |
| 71-75 | 20% | 8-12 weeks |
| 76+ | 25% | 12+ weeks |
The table shows how age can change surgery results and recovery times. It’s key for patients and doctors to talk about these things before surgery.
In short, age is a big deal in deciding about prostate surgery. Knowing how age affects surgery can help patients choose the best treatment.
The Age Limit for Prostate Surgery: Is There One?
As men get older, deciding on prostate surgery is complex. It’s not just about how old they are. Their health and overall condition are key factors.
Medical Guidelines on Age Restrictions
Medical guidelines on age for prostate surgery vary. Some urological groups share insights on what to consider. There’s no strict age limit for everyone, but guidelines focus on a patient’s health and age.
Guidelines suggest a detailed assessment. This includes looking at the patient’s health, heart condition, and other important factors. It helps decide if surgery is right for them.
Case-by-Case Assessment Approach
Every patient is different when it comes to prostate surgery. Age is just one factor. Their health, the severity of their prostate issue, and what they want also matter.
- Looking at the patient’s overall health and medical history.
- Checking how severe the prostate problem is and its effect on their life.
- Talking about the surgery’s benefits and risks with the patient.
This personalized way helps doctors make choices that are best for each patient.
Prostate Surgery in Men Over 70
Men aged 70 and above can have prostate surgery. But, they must weigh the risks and benefits carefully. This is important to see if the surgery’s benefits are worth the risks, considering their health and how long they might live.
Risk-Benefit Analysis
For men over 70 thinking about prostate surgery, a detailed risk-benefit analysis is key. This looks at the patient’s overall health status. It checks for any other health issues, how bad the prostate symptoms are, and how surgery might affect their life quality.
Things like cardiovascular health, kidney function, and brain health are important in this review. It also looks at the chance of complications and if more treatments might be needed after surgery.
Success Rates and Complications
The success of prostate surgery in men over 70 depends on several things. These include the surgery method, the patient’s health, and the surgeon’s skill. Minimally invasive surgical techniques often work well for older patients. They tend to have fewer problems and heal faster.
But, surgery can have risks like trouble controlling urine, erectile issues, and infections. Talking to a healthcare provider is vital to understand these risks and how they might affect the individual patient.
Recovery times for prostate surgery vary. Most men can get back to their usual activities in a few weeks. The exact time depends on the surgery type and the patient’s health.
Prostate Surgery for Octogenarians (80+)
As more people live longer, the debate on prostate surgery for men over 80 grows. This topic is complex, needing careful thought about many factors.
Special Considerations for Very Elderly Patients
Men over 80 facing prostate surgery face special challenges. They often have more health issues and less energy. Careful patient selection is key to find those who can safely benefit from surgery.
Health problems like heart disease or diabetes can make surgery riskier. So, a detailed check before surgery is vital to understand the patient’s health.
Real-world Outcomes Data
Studies reveal that selected octogenarians can do well with prostate surgery. Real-world data offer insights into its success and safety for this age group.
Research shows that, with the right selection and care, many octogenarians see big improvements. They enjoy better quality of life and fewer symptoms.
Treatment for Prostate Cancer in 90-Year-Old Men
Treating prostate cancer in men over 90 is complex. It’s about finding the right balance between treatment benefits and risks. At this age, the main goal is to improve the patient’s quality of life, not just fight the cancer.
Surgical vs. Non-Surgical Approaches
Choosing between surgery and non-surgical methods for prostate cancer in older men is tough. Surgery, like prostatectomy, might be best for those with aggressive cancer and a long life ahead. But for men over 90, the risks of surgery, like complications and long recovery times, often seem too high.
Non-surgical options, like active surveillance, radiation therapy, and hormone therapy, are usually better for the elderly. They help manage the disease without causing too many side effects.
Quality of Life Priorities
For men in their 90s, quality of life is key in prostate cancer treatment. The aim is to keep them comfortable, reduce symptoms, and help them stay functional. Treatment plans are made just for each patient, considering their health, life expectancy, and what they want.
It’s also important to think about whether one can live without a prostate. Many men do well without it after prostatectomy. But, this surgery is rare in very elderly men because of the risks.
In summary, treating prostate cancer in 90-year-old men needs a careful and tailored approach. It’s about finding the right treatment balance to improve their quality of life.
Health Factors That Matter More Than Age
Health factors like comorbidities and functional status are key in deciding if someone can have prostate surgery. Age is important, but it’s not the only thing doctors look at.
Doctors don’t just look at how old you are when deciding if you can have prostate surgery. They also check your overall health. This includes looking at your comorbidities, how well you function, and your heart health.
Comorbidities and Their Impact
Comorbidities are other health problems you might have, like diabetes or heart disease. These can affect how risky surgery is and how well you’ll recover.
For example, someone with uncontrolled diabetes might face more risks during surgery. This could include problems with healing and a higher chance of infection. People with serious heart disease might need extra checks before surgery to lower their heart risks.
Functional Status Assessment
Your functional status is also important. It shows how well you can do everyday things and take care of yourself.
People who are more functional usually do better after surgery. This is because they are stronger and can recover faster. Doctors use this to guess how well you’ll do after surgery and how soon you’ll be back to normal.
Cardiovascular Health
Your cardiovascular health is also a big deal. If you have heart problems, you’re at higher risk for serious issues during surgery.
Before surgery, doctors do tests to check your heart. This might include stress tests or heart catheterizations. These help figure out if you need to do anything before surgery to make your heart safer.
By looking at these health factors, doctors can make better choices about surgery. This leads to better results and a better life for you.
How Long Is Prostate Surgery Recovery?
Recovering from prostate surgery depends on age, health, and the surgery type. Each person’s recovery time is different. It’s important to know what affects it.
Timeline for Recovery by Age Group
Recovery times vary with age. Younger men usually heal faster because they are healthier and have fewer health issues.
- Men under 60: Typically recover within 3-6 weeks.
- Men between 60-70: May take 6-8 weeks to recover.
- Men over 70: Recovery can take 8-12 weeks or longer.
Rehabilitation Considerations
Rehabilitation is key to getting better. It includes exercises and lifestyle changes to boost strength and improve health.
Key rehabilitation considerations include:
- Pelvic floor exercises to improve urinary continence.
- Physical activity to enhance overall health and reduce the risk of complications.
- Dietary changes to support healing and maintain a healthy weight.
Returning to Normal Activities
Going back to normal activities after surgery should be slow. Patients should avoid heavy lifting and strenuous activities for weeks.
It’s essential to follow the surgeon’s instructions on post-operative care and activity levels for a smooth recovery.
Understanding the recovery process and following post-surgery guidelines helps patients heal faster. They can get back to their normal activities sooner.
Life Expectancy After TURP Surgery
Men who have TURP surgery often wonder about their life expectancy and how their quality of life will improve. TURP, or transurethral resection of the prostate, helps treat BPH. This condition can really affect a man’s daily life.
Understanding Survival Rates by Age Group is key for men thinking about TURP. Studies show that TURP is safe for many ages. But, individual health factors greatly affect the results.
Survival Rates by Age Group
Looking at survival rates by age helps us see how well TURP works. Even older men can benefit from it, thanks to better surgery methods. Here’s what the data say:
- Men under 65 usually do well and recover quickly.
- Those 65 to 75 might face slightly lower survival rates because of health issues.
- Men over 75 can also see benefits from TURP, but their health and other conditions matter a lot.
Quality of Life Improvements
TURP surgery greatly improves quality of life. It helps with BPH symptoms like not being able to hold urine and needing to pee a lot. Men often sleep better, feel less pain, and can do more things they love.
In summary, while many factors affect life expectancy after TURP, it usually leads to good results. Men thinking about TURP should talk to their doctor. This way, they can understand the good and bad sides.
Is Prostate Removal Major Surgery?
Men facing prostate removal surgery often wonder about the procedure’s details and recovery. Prostate removal, or prostatectomy, is a major surgery. It’s complex and comes with risks.
The surgery is complex because it involves removing the prostate gland carefully. It must be done without harming nearby nerves and tissues. Different techniques, like open, laparoscopic, and robotic-assisted surgeries, are used.
Surgical Complexity and Risks
Risks of prostate removal surgery include infection, bleeding, and damage to nearby structures. But, new surgical methods have reduced these risks. A thorough preoperative evaluation is key to check the patient’s health and spot risks.
- Bleeding and hematoma formation
- Infection and wound complications
- Damage to surrounding nerves and tissues
Hospital Stay and Immediate Recovery
The hospital stay for prostate removal surgery varies. It depends on the surgery type and the patient’s health. Usually, patients stay 1-3 days. Right after surgery, they manage pain, follow catheter care, and slowly get back to normal activities.
Understanding the risks and recovery is key for patients. Talking to their healthcare provider helps. This way, men can prepare for the challenges and benefits of prostate removal surgery.
Can You Live Without a Prostate?
Many men live without a prostate after surgery. This is due to conditions like prostate cancer. The prostate gland is key to the male reproductive system. But, removing it is sometimes needed.
Physical Changes After Prostate Removal
Men face physical changes after prostate surgery. One big change is in urinary function. The prostate surrounds part of the urethra, affecting urine flow.
Urinary incontinence is common at first but usually gets better. Kegel exercises help a lot. Sexual function can also change. Erectile dysfunction is a possible side effect, but it varies by age and health.
Long-term Adaptation
Most men adapt well to life without a prostate. New surgical methods, like nerve-sparing prostatectomy, help a lot. They reduce long-term problems.
Men need to make lifestyle changes. They must do pelvic floor exercises to keep urine in. They might also need help for erectile dysfunction.
Regular check-ups with the doctor are key. This helps track recovery and solve any issues that come up.
Side Effects of Prostate Removal
Prostate removal is a common treatment for prostate cancer. It can change a patient’s quality of life. It’s important for patients to know these changes before deciding on surgery.
Urinary Function Changes
Urinary function is a big concern after prostate removal. Urinary incontinence is a common side effect. It can range from mild leakage to severe incontinence.
The severity and how long it lasts vary. Some patients see improvement over time. Pelvic floor exercises, like Kegel exercises, can help improve urinary control.
Sexual Function Impact
Sexual function is also affected by prostate removal. Erectile dysfunction (ED) is a common side effect. This is because nerves and blood vessels near the prostate can be damaged during surgery.
The extent of ED varies. Age, pre-surgery erectile function, and surgical technique play a role. Nerve-sparing techniques are used to try to preserve sexual function.
Other Quality of Life Considerations
Other aspects of quality of life can also be affected. Some patients may feel anxious or depressed after surgery. These emotional changes are common.
There can also be changes in organ function and physical condition. It’s important to talk to a healthcare provider about these possible effects. They can help manage them.
Patients should know about these possible side effects before choosing prostate removal. While it can save lives or improve quality of life, understanding the outcomes is key to making a good decision.
Alternative Treatments for Elderly Prostate Patients
Elderly men with prostate cancer have many treatment options. The choice depends on the cancer’s stage, the patient’s health, and personal wishes.
Active Surveillance
Active surveillance means watching the cancer closely. It’s for those with low-risk cancer. It helps avoid the side effects of aggressive treatments.
Benefits of Active Surveillance:
- It keeps quality of life high by avoiding treatment side effects
- It reduces the chance of treating cancers too much
- It lets doctors step in if the cancer starts to grow
Radiation Therapy Options
Radiation therapy is a choice for elderly prostate cancer patients. It kills or slows cancer cells with high-energy rays. There are two main types: external beam radiation therapy (EBRT) and brachytherapy.
Types of Radiation Therapy:
| Therapy Type | Description | Benefits |
| EBRT | Delivers radiation from outside the body | Non-invasive, precise targeting |
| Brachytherapy | Involves placing radioactive material inside the body near the tumor | Localized treatment, reduced side effects |
Hormone Therapy Approaches
Hormone therapy, or androgen deprivation therapy (ADT), lowers male hormones that help cancer grow. It’s often used with other treatments.
Considerations for Hormone Therapy:
- It can be used alone or with other treatments
- It may cause side effects like hot flashes and fatigue
- Regular checks are needed to see how well it works and manage side effects
At What Age Should I Stop Getting a PSA Test?
Age is key in deciding when to stop PSA tests for prostate cancer. As men age, weighing the benefits and risks of testing becomes more important.
Choosing to stop PSA tests isn’t easy. It depends on a man’s health, how long he might live, and his personal values. Usually, guidelines say men with a short life expectancy might not need more tests.
Screening Guidelines by Age
Many health groups have set rules for PSA screening based on age. For example:
- The United States Preventive Services Task Force (USPSTF) advises against routine PSA tests for men over 70.
- The American Cancer Society says men should talk to their doctors about PSA tests. They should think about their age, health, and what they prefer.
| Age Group | Guideline Recommendation |
| 70+ | USPSTF recommends against routine PSA screening |
| 65-69 | Consider life expectancy and health status |
| <65 | Discuss benefits and risks with healthcare provider |
Individual Risk Assessment
Age isn’t the only thing that matters. Other factors, like family history and ethnicity, also play a big role. These include:
- Family history of prostate cancer
- Ethnicity (e.g., African American men are at higher risk)
- Previous prostate issues or abnormal PSA results
- Presence of other health conditions that may impact life expectancy
Men with higher risk factors might need to keep getting tested, even if they’re older. Those with lower risk might safely stop testing sooner.
Ultimately, the decision to stop PSA testing should be made in consultation with a healthcare provider, taking into account individual circumstances and preferences.
Technological Advances Making Surgery Safer for Older Patients
New surgical technologies are changing prostate surgery for older patients. They offer safer and more effective treatments. These advancements have made surgeries better, with shorter recovery times and fewer problems.
Minimally Invasive Techniques
Modern prostate surgery often uses small incisions. This means less damage and pain for older patients. They also face a reduced risk of infection.
These surgeries are shorter, letting patients get back to their lives faster.
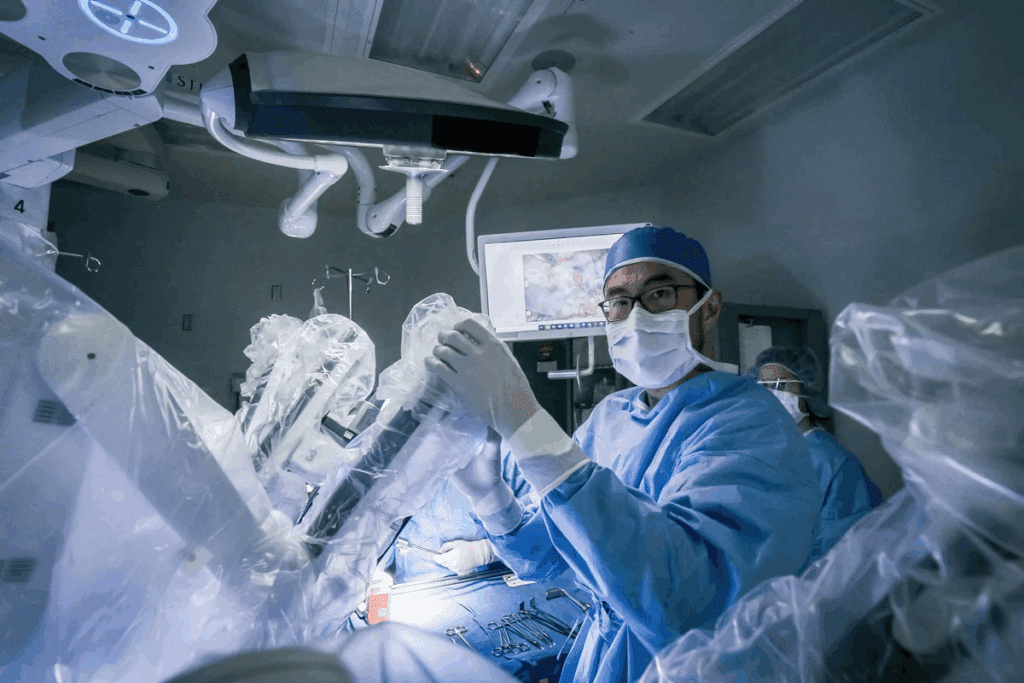
Robotic-Assisted Surgery Benefits
Robotic-assisted surgery is a big step forward in urology. It gives surgeons better control and precision. For older patients, it means improved surgical outcomes and a lower risk of complications.
The technology allows for more accurate surgery. It helps avoid damage to nerves and tissues.
Robotic-assisted surgery is great for older patients. It reduces blood loss, pain, and recovery time. This makes it a good choice for those with health issues that could make traditional surgery harder.
Conclusion: Personalized Approach to Prostate Surgery Across Age Groups
A personalized approach to prostate surgery looks at each patient’s unique factors, like age. Age is important, but not the only thing to consider. Biological age, overall health, and any other health issues also matter a lot.
In India, new advancements in prostate cancer surgery help older patients have successful surgeries. It’s all about checking the patient’s health carefully. This includes how well they function and their heart health to see if surgery is safe.
Healthcare providers can give each patient a treatment plan that fits their needs, no matter their age. This way, older patients get the right care. It balances treating cancer with the risks and side effects of surgery.
FAQ
What is the age limit for TURP surgery?
There’s no strict age limit for TURP surgery. It depends on your health and how bad your symptoms are.
Can an 80-year-old man have prostate surgery?
Yes, an 80-year-old man can have prostate surgery. It depends on his health, any other health issues, and the surgery’s benefits and risks.
What is the life expectancy after TURP surgery?
Life expectancy after TURP surgery varies. It depends on your age, health, and any other medical conditions you have.
Is prostate removal a major surgery?
Yes, removing the prostate is a major surgery. It affects your urine and sex life.
Can you live without a prostate?
Yes, living without a prostate is possible. But, you’ll need to make big lifestyle changes and manage side effects like incontinence and erectile dysfunction.
What are the side effects of prostate removal?
Side effects include incontinence, erectile dysfunction, and changes in bowel habits. These can vary from person to person.
At what age should I stop getting a PSA test?
Stopping PSA tests depends on your age, health, and medical conditions. Men with a short life expectancy may not need them.
What are the alternative treatments for elderly prostate cancer patients?
Elderly patients have options like active surveillance, radiation, and hormone therapy. The choice depends on the cancer’s stage, your health, and what you prefer.
How long is prostate surgery recovery?
Recovery time varies. It depends on your age, health, and the surgery type. It can take weeks to months.
Can prostate cancer be treated in men over 90?
Yes, men over 90 can be treated for prostate cancer. Treatment depends on their health, any other conditions, and life expectancy.
What are the benefits of robotic-assisted prostate surgery?
Robotic-assisted surgery offers precision, less blood loss, and faster recovery. It’s better than traditional surgery.
How do health factors influence the decision to undergo prostate surgery?
Your health, including any other conditions, affects if you’re a good candidate for surgery.
What is the success rate of prostate surgery?
Success rates vary. It depends on the surgery type, the surgeon’s skill, and your health.
Can you have your prostate gland removed?
Yes, removing the prostate gland is possible. But, consider the benefits and risks carefully before deciding.
Reference
- Mandel, P. (2017). Radical prostatectomy in patients aged 75 years or older: A review of indications and outcomes. Journal of Urology, 198(3), 856-862. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC6337955/





